Abstract
Context
Performance measures, particularly pay-for-performance, may have unintended consequences for safety-net institutions caring for disproportionate shares of Medicaid or uninsured patients.
Objective
Describe emergency department (ED) compliance with proposed length of stay measures for admissions (8 hours) and discharges, transfers, and observations (4 hours) by safety-net status.
Design, Setting, and Participants
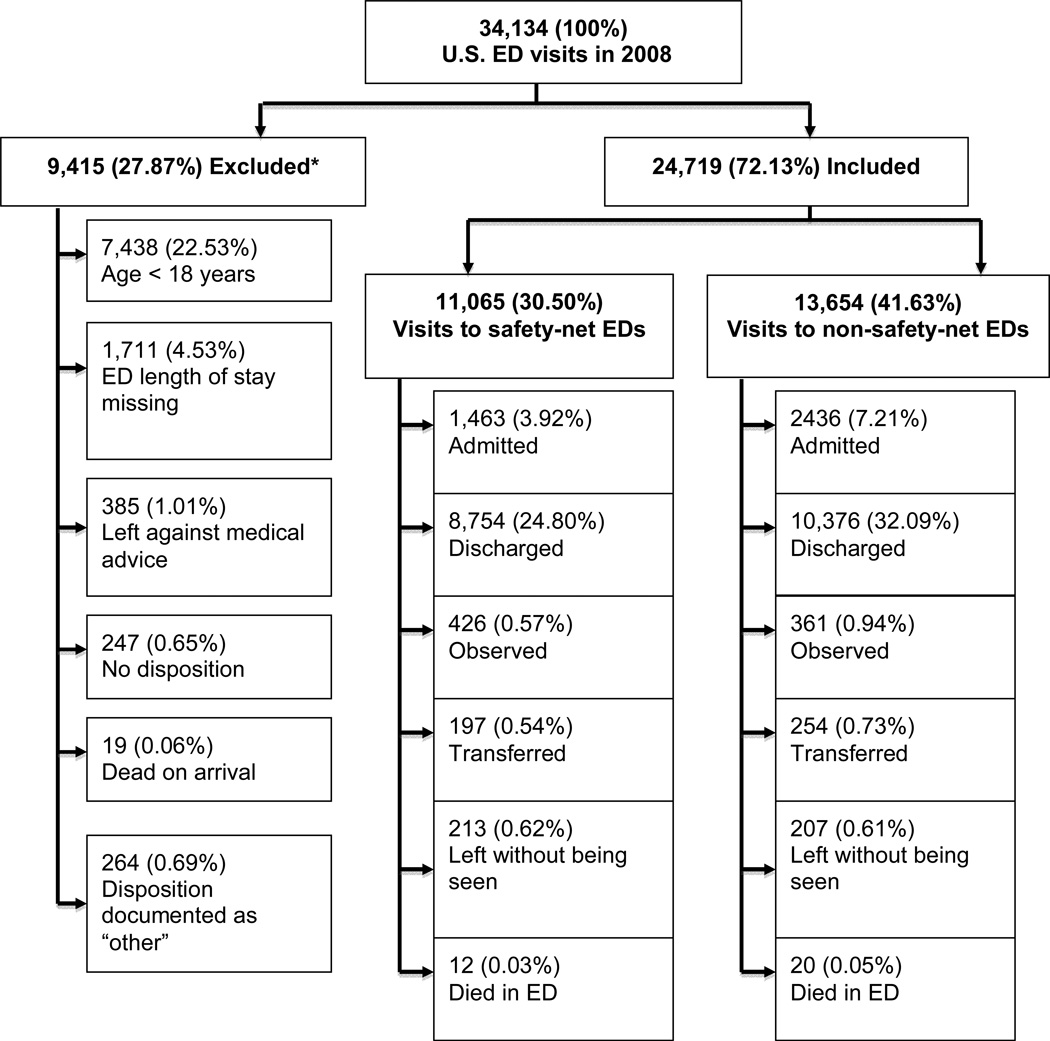
2008 National Hospital Ambulatory Medical Care Survey (NHAMCS) ED data were stratified by safety-net status (CDC definition) and disposition (admission, discharge, observation, transfer). The 2008 NHAMCS is a national probability sample of 396 hospitals (90.2% unweighted response rate) and 34,134 patient records. Visits were excluded for age <18, missing length of stay, or dispositions of: missing, “other”, left against medical advice, dead on arrival. Median and 90th percentile ED lengths of stay were calculated for each disposition and admission/discharge subcategories (critical care, psychiatric, routine) stratified by safety-net status. Multivariate analyses determined associations with length of stay measure compliance. Results are presented as odds ratios with 95% confidence intervals.
Main Outcome
ED length of stay measure compliance by disposition and safety-net status.
Results
27.87% of the 2008 ED visits from the weighted NHAMCS dataset were excluded leaving 72.13% for analysis. Of these, 42.3% were to safety-net and 57.7% to non-safety-net EDs. The median (interquartile range) ED lengths of stay for safety-net and non-safety-net ED visits respectively are as follows: 269 minutes (178, 397) and 281 (178, 401) for admissions, 156 (95, 239) and 148 (88, 238) for discharges, 355 (221, 675) and 298 (195, 440) for observations, and 235 (155, 378) and 239 (142, 368) for transfers. Safety-net status is not independently associated with compliance with ED length of stay measures for admissions (OR 0.83, [95%CI 0.52, 1.34]), discharges (1.03 [0.83, 1.27]), observations (1.05 [0.57, 1.95]), transfers (1.30 [0.70, 2.45]), or subcategories except psychiatric discharges (1.67 [1.02, 2.74]).
Conclusion
Compliance with proposed ED length of stay measures for admissions, discharges, transfers, and observations does not differ significantly between safety-net and non-safety-net hospitals.
Introduction
Performance measures and pay for performance schemes aim to improve quality of care in all arenas of health care, including the emergency department (ED). Performance measures established by the Centers for Medicare and Medicaid Services (CMS) and The Joint Commission are among the most widely distributed and well known. In January 2009, the Department of Health and Human Services contracted with the National Quality Forum (NQF) to vet quality and efficiency measures for use in reporting on and improving healthcare quality. When selecting new measures for implementation, CMS is encouraged to choose from among measures approved by the NQF.
One of the main concerns has been the potential for unintended consequences of such measures on facilities that provide care to vulnerable populations. Such consequences are of particular concern to EDs. While all EDs must, by law, provide care to any patient presenting to their doors, those identified as safety-net EDs provide a disproportionate share of services to patients with Medicaid and the uninsured. The number of EDs qualifying as safety-net providers has increased from 43% in 2000 to 63% in 2007.1
In 2008, the NQF approved two quality measures related to ED length of stay: the median time from arrival to ED departure for admitted patients and for discharged patients.2 While these measures do not stipulate specific acceptable timeframes for ED length of stay or prescribe a given percentage of ED patients that must meet these goals, other organizations have suggested a median or 90th percentile less than 4 hours for discharged patients and less than 8 hours for those admitted to the hospital.3,4 If these measures are tied to pay for performance, chronically underfunded safety-net EDs could be at risk for further reductions in funding which could only exacerbate the lack of resources available in those settings.
This study examines the performance of U.S. EDs with respect to length of stay targets of 4 hours for patients discharged to home, transferred to another hospital, or admitted to observation and 8 hours for those admitted to an inpatient bed. We hypothesize that safety-net EDs perform worse on the ED length of stay measures than non-safety-net EDs as measured by medians and 90th percentiles.
Methods
Study Design
We analyzed data from the 2008 National Hospital Ambulatory Medical Care Survey (NHAMCS). NHAMCS is an annual, national probability sample survey of visits to EDs of non-institutional general and short-stay hospitals conducted by the Centers for Disease Control and Prevention (CDC) National Center for Health Statistics.5 NHAMCS data are derived through a multistage estimation procedure that produces unbiased estimates.6 The 2008 NHAMCS dataset was obtained from 431 of 463 Emergency Service Areas (93.1% unweighted ED response rate) and a total of 34,134 patient visits. This is a publicly available dataset with no patient identifiers and therefore this study was exempt from review by the institutional review board of the University of California, San Francisco.
We examined ED length of stay for all adult ED visits from 2008 stratified by disposition and hospital safety-net status. Adults were defined as individuals 18 years and older. ED length of stay is defined as the interval between time of ED arrival and time of ED departure (either admission or discharge). In the 2008 NHAMCS ED visit survey tool, individual ED visits could have multiple dispositions. For example, a single ED visit could have a disposition of admission to the hospital and admission to observation. To create mutually exclusive categories, we assigned ED visits with a single disposition of admission, discharge, observation, transfer, left without being seen, and died in the ED according to the following hierarchy:
Patients < 18 years old, missing ED length of stay data, those with no answer to disposition, dead on arrival, left against medical advice, and disposition of “other” were excluded;
Those with any disposition of “transfer” were considered transferred;
Of the remaining, those with any disposition of admission to observation were considered admitted to observation;
Of the remaining, those with any disposition of admission to the hospital were considered admitted to the hospital;
Of the remaining, those with any disposition of left before medical screening exam or left after medical screening exam were considered as left without being seen;
Of the remaining, those with any disposition of died in the ED were considered to have died in the ED;
Of the remaining, those with any disposition of “no follow-up planned”, “return if needed/PRN”, “return/refer to physician/clinic for follow-up”, or “refer to social services” were considered “discharged”.
Admitted and discharged patients were grouped into categories designated by the NQF’s National Voluntary Consensus Standards for Emergency Care, which was conducted under contract from CMS: critical care, psychiatric, and routine (non-critical care, non-psychiatric) admissions.2 We identified psychiatric visits as those with a primary ICD-9 code meeting those established by the Healthcare Cost and Utilization Project (HCUP) Mental Health and Substance Abuse Clinical Classifications Software (CCS-MHSA).7
Safety-net status was determined according to the CDC definition: more than 30% of total ED visits with Medicaid as expected source of payment, more than 30% of total ED visits with self-pay or no charge as the expected pay source (considered uninsured), or a combined Medicaid and uninsured patient pool greater than 40% of total ED visits.8
We obtained the following demographic and presenting characteristics: patient age, sex, race, ethnicity, triage acuity, and clinician type (attending physician, resident/intern physician, nurse practitioner [NP]/physician assistant [PA], or other/missing). For the 2008 NHAMCS survey, race and ethnicity were entered by hospital personnel according to each hospital’s usual practice. Data abstractors were instructed not to ask patients for this information and, for those cases where the race or ethnicity were not known or obvious, to enter what they felt was most appropriate. The National Center for Health Statistics replaced missing values with imputed values randomly assigned from patient records with similar characteristics. Safety-net EDs provide care for a disproportionate volume of patients with Medicaid and the uninsured who are themselves over-represented by racial and ethnic minorities. We therefore included race and ethnicity in our analyses to investigate if either were independently associated with compliance with the proposed ED length of stay targets. Triage acuity is defined by the immediacy with which a patient should be seen (immediate, 1–14 minutes, 15–60 minutes, >1 hour-2hours, >2 hours-24 hours, no triage, or unknown). Additionally, we obtained hospital ED characteristics including hospital setting (rural, urban), hospital ownership type (non-profit, government, proprietary), and location (northeast, midwest, south, west).
Statistical Analysis
We present unweighted and weighted characteristics of ED visits in descriptive terms. ED length of stay data is presented as medians (interquartile range) and 90th percentiles stratified by ED safety-net status and patient disposition. Ninety-five percent confidence intervals and p-values were calculated using standard methods accounting for the complex survey design and sampling weights.
We chose to analyze the data with respect to the suggested ED length of stay goals of a median or 90th percentile less than 4 hours for discharged patients and less than 8 hours for those admitted to the hospital as suggested by the Accreditation Council for Graduate Medical Education and Ontario Ministry of Health, respectively.3,4 We created separate bivariate models to assess the association between ED safety-net status and performance on ED length of stay goals for patients admitted to the hospital (stratified by all admissions, critical care admissions, psychiatric admissions, and routine admissions [all non-critical care and psychiatric admissions]), discharged (stratified by all discharges, psychiatric discharges, and routine discharges [all non-psychiatric discharges]), those admitted to an observation unit, those transferred to another hospital, and those who left without being seen.
To determine independent associations with compliance with the proposed ED length of stay targets, we developed multivariate models stratified by disposition type. All predictors (ED safety-net status, patient demographics, ED provider type, presenting acuity, ED setting, hospital ownership, and hospital location) except patient insurance (since this was factored into the ED safety-net status) were included in the multivariate models. Results are presented as odds ratios with 95% confidence intervals. All analyses were performed using SAS (version 9.2; SAS Institute, Cary, North Carolina) and Sudaan, version 10.0 (RTI International, Research Triangle, North Carolina) to account for the complex sampling design and the patient weights.
Sensitivity Analysis
Patients who left without being seen could potentially lower the median length of stay and result in harm, depending on the characteristics of the patients who left. Similarly, patients who died in the ED may also lower the median length of stay. We determined the number of unweighted observations, weighted percentage of visits, and ED lengths of stay among patients who left without being seen and among those who died in the ED, stratified by ED safety-net status. To explore the impact these two patient groups have on median length of stay and on compliance with the proposed length of stay target for admitted patients (<8 hours), we constructed a multivariate model, incorporating both patient groups into the admitted patient group.
Results
27.9% of the weighted visits in the 2008 NHAMCS dataset met exclusion criteria. Leaving 72.1% for analysis. Of the latter, 42.3% were seen in safety-net and 57.7% in non-safety-net EDs (Figure).
Figure.
CONSORT diagram showing 2008 U.S. ED visit data from NHAMCS dataset (unweighted observations [weighted percentages]) and study inclusion/exclusion. *Visits may have met more than 1 exclusion criterion. Percentages in each column do not equal the total due to rounding.
Overall, patients going to safety-net EDs were more likely to be young and minority compared with non-safety-net EDs. They were less likely to need emergent or urgent care in both admitted and discharged populations. Patient demographic and presenting characteristics as well as hospital characteristics stratified by patient disposition and ED safety-net status are shown in Table 1(for admitted patients) and eTables 1–4 (for patients who were discharged, admitted to observation, transferred, and left without being seen, respectively), with the exception of those who died in the ED, as there were only 32 unweighted observations in this category (12 in safety-net and 20 in non-safety-net EDs). Triage categories of “immediate” and “1–14 minutes” were combined for these analyses.
Table 1.
Patient demographic and presenting characteristics and hospital characteristics for admitted patients stratified by ED safety-net status among U.S. ED visits for 2008.
| Unweighted No. (Weighted Percentage, %) [95% CI] by ED Safety-Net Status |
Weighted P-Value |
||
|---|---|---|---|
| Safety-Net | Non-Safety-Net | ||
| All patients | 1463 (100) | 2436 (100) | |
| Patient age (years) | <0.001 | ||
| 18–25 | 117 (6.9) [5.1, 8.7] | 102 (3.4) [2.4, 4.4] | |
| 26–64 | 826 (53.1) [49.4, 56.8] | 1093 (45.4) [42.5, 48.3] | |
| >64 | 520 (40.0) [36.3, 43.7] | 1241 (51.2) [48.1, 54.3] | |
| Patient sex | 0.41 | ||
| Female | 733 (51.7) [47.6, 55.8] | 1308 (53.8) [51.3, 56.3] | |
| Male | 730 (48.3) [44.2, 52.4] | 1128 (46.2) [43.7, 48.7] | |
| Patient race/ethnicity | 0.02 | ||
| White, non-Hispanic | 832 (63.1) [54.7, 71.5] | 1782 (73.4) [68.9, 77.9] | |
| Black/African American, non-Hispanic | 391 (23.9) [17.0, 30.8] | 329 (13.4) [9.7, 17.1] | |
| Hispanic | 192 (11.1) [5.8, 16.4] | 210 (9.6) [6.1, 13.1] | |
| Other | 48 (1.9) [0.9, 2.9] | 115 (3.7) [2.3, 5.1] | |
| Patient insurance type | <0.001 | ||
| Private | 283 (21.1) [17.4, 24.8] | 695 (27.3) [24.2, 30.4] | |
| Medicare | 601 (46.5) [42.2, 50.8] | 1240 (51.3) [47.6, 55.0] | |
| Medicaid | 338 (17.1) [13.0, 21.2] | 186 (7.6) [6.0, 9.2] | |
| Uninsured | 164 (10.8) [8.4, 13.2] | 107 (3.8) [2.9, 4.7] | |
| Other/Unknown | 77 (4.5) [2.9, 6.0] | 208 (9.9) [5.8, 14.0] | |
| Clinician type | 0.78 | ||
| Resident/intern | 234 (14.4) [6.4, 22.4] | 355 (14.3) [9.0, 19.6] | |
| NP/PA | 101 (6.2) [3.7, 8.7] | 127 (5.0) [3.2, 6.8] | |
| Attending | 1095 (76.3) [68.5, 84.1] | 1890 (78.2) [72.5, 83.9] | |
| Other/Missing | 33 (3.2) [1.9, 4.5] | 64 (2.6) [1.4, 3.8] | |
| Patient triage acuity (minutes) | 0.56 | ||
| <15* | 459 (31.6) [26.3, 36.9] | 882 (37.4) [31.9, 42.9] | |
| 15–60 | 591 (41.3) [34.2, 48.4] | 1010 (41.7) [37.2, 46.2] | |
| 61–120 | 106 (9.5) [5.0, 14.0] | 187 (7.7) [5.5, 9.9] | |
| >120 | 32 (3.2) [1.3, 5.1] | 69 (2.3) [0.5, 4.1] | |
| Unknown | 275 (14.4) [6.4, 22.4] | 288 (10.9) [7.2, 14.6] | |
| Hospital setting | 0.45 | ||
| Rural | 139 (15.0) [5.0, 25.0] | 271 (11.3) [4.0, 18.6] | |
| Urban | 1324 (85.0) [75.0, 95.0] | 2165 (88.7) [81.4, 96.0] | |
| Hospital owner | 0.007 | ||
| Non-profit | 1038 (78.1) [69.3, 86.9] | 2066 (87.4) [80.7, 94.1] | |
| Government | 370 (17.1) [9.1, 25.1] | 142 (3.6) [0.7, 6.5] | |
| Proprietary | 55 (4.8) [0.7, 8.9] | 228 (9.0) [2.7, 15.3] | |
| Hospital location | 0.02 | ||
| Northeast | 368 (19.0) [9.0, 29.0] | 663 (23.9) [16.6, 31.2] | |
| Midwest | 259 (20.6) [8.3, 32.9] | 664(27.3) [19.9, 34.7] | |
| South | 646 (47.9) [35.6, 60.2] | 587 (25.1) [16.7, 33.5] | |
| West | 190 (12.5) [5.1, 19.9] | 542 (23.7) [15.7, 31.7] | |
| ED Diagnosis Subcategory | 0.76 | ||
| Critical | 175 (12.5) [9.4, 15.6] | 293 (13.2) [10.3, 16.1] | |
| Routine (non-psychiatric, non-critical) | 1132 (83.6) [80.5, 86.7] | 2042 (83.7) [80.4, 87.0] | |
| Psychiatric | 156 (3.9) [2.3, 5.5] | 101 (3.2) [2.2, 4.2] | |
NP = Nurse practitioner
PA = Physician assistant
Triage categories “Immediate” and “1–14 minutes” were combined for the purpose of this analysis
For admitted patients, median (IQR) ED length of stay was 269 (178, 397) in safety-net EDs compared with 281 (178, 401) minutes in non-safety-net EDs, respectively. Critical care admissions accounted for 12.5% of all admissions via safety-net EDs and 13.2% in non-safety-net EDs in 2008. Median (IQR) ED length of stay for critical care admissions was 236 (149, 371) and 248 (157, 346) minutes for safety-net and non-safety-net EDs, respectively. Psychiatric admissions accounted for 3.9% of all admissions via safety-net EDs and 3.2% in non-safety-net EDs, with median (IQR) ED length of stay of 253 (172, 506) and 290 (173, 579) minutes, respectively. For discharged patients, the median (IQR) ED length of stay in safety-net EDs was 156 (95, 239) minutes and 148 (88, 238) minutes in non-safety-net EDs. Complete results of the median and 90th percentile ED lengths of stay stratified by patient disposition and ED safety-net status of U.S. ED visits for 2008 are presented in Table 2. Median lengths of stay for admitted (or the subgroups of critical care, routine, psychiatric admissions), discharged patients (or the subgroups of routine, psychiatric), transferred, observed, or died in the ED patients were similar in the safety-net and non-safety-net EDs. The mean ED lengths of stay among those who left without being seen in non-safety net EDs were shorter (97 vs 120 minutes).
Table 2.
Median and 90th percentile ED length of stay for safety-net and non-safety-net hospitals, NHAMCS 2008.
| Safety-net | Non-safety-net | |||||||
|---|---|---|---|---|---|---|---|---|
| Unweighted Observations (No.) |
Weighted Percentages (%)* |
Median ED Length of Stay (95% CI) (in minutes) |
90th Percentile ED Length of Stay (95% CI) (in minutes) |
Unweighted Observations (No.) |
Weighted Percentages (%) |
Median ED Length of Stay (95% CI) (in minutes) |
90th Percentile ED Length of Stay (95% CI) (in minutes) |
|
| Admissions | 1463 | 3.92 | 269 (178, 397) | 595 (478, 1067) | 2436 | 7.21 | 281 (178, 401) | 576 (529, 615) |
| Critical | 175 | 0.49 | 236 (149, 371) | 542 (422, 1149) | 293 | 0.95 | 248 (157, 346) | 520 (420, 756) |
| Routine (non-critical and non-psychiatric) | 1132 | 3.28 | 271 (187, 395) | 583 (474, 1029) | 2042 | 6.03 | 285 (180, 407) | 572 (525, 610) |
| Psychiatric | 156 | 0.15 | 253 (172, 506 | 908 (434, 1167) | 101 | 0.23 | 290 (173, 579) | 734 (581, 914) |
| Discharges | 8754 | 24.80 | 156 (95, 239) | 347 (323, 368) | 10376 | 32.09 | 148 (88, 238) | 348 (330, 366) |
| Routine (non-psychiatric) | 8299 | 24.02 | 155 (94, 236) | 342 (316, 362) | 10030 | 31.14 | 147 (87, 236) | 344 (328, 361) |
| Psychiatric | 455 | 0.79 | 205 (130, 332) | 534 (417, 688) | 346 | 0.96 | 186 (98, 307) | 513 (397, 716) |
| Admitted to observation | 426 | 0.57 | 355 (221, 675) | 1335 (933, 1719) | 361 | 0.94 | 298 (195, 440) | 904 (530, 1237) |
| Transferred | 197 | 0.54 | 235 (155, 378) | 535 (421, 776) | 254 | 0.73 | 239 (142, 368) | 522 (417, 653) |
| Left without being seen | 213 | 0.62 | 120 (62, 215) | 353 (308, 441) | 207 | 0.61 | 97 (46, 204) | 274 (250, 375) |
| Died in ED | 12 | 0.03** | 128 (35, 211) | 238*** | 20 | 0.05** | 121 (33, 167) | 195 (136, 352) |
Weighted percentages represent percentage of total estimated ED visits from the 2008 NHAMCS dataset, including those excluded from further analyses in this study
<30 visits, analyses considered unreliable by the National Center for Health Statistics
CIs not produced because of small n (n=12)
Results of the bivariate (ED length of stay by patient disposition and ED safety-net status alone) and multivariate models for odds of failing to comply with a target ED length of stay less than 8 hours for admissions is shown in Table 3 (eTables 5–7 depict the results of the bivariate and multivariate models for subcategories of admitted patients [critical care, routine, and psychiatric]). Results of the bivariate (ED length of stay by patient disposition and ED safety-net status alone) and multivariate models for odds of failing to comply with the proposed ED length of stay less than 4 hours for discharges, admitted to observation, and transferred to another hospital are shown in Tables 4 (eTables 8 and 9 for routine and psychiatric discharge subcategories), and eTables 10–11, respectively.
Table 3.
Multivariate adjusted odds of ED length of stay > 8 hours for admitted ED patients, NHAMCS 2008.
| Weighted Event Rate 15.8% |
Adjusted Odds Ratio [95% CI] |
|
|---|---|---|
| BIVARIATAE WITH ED PAYER MIX ONLY | ||
| ED payer mix | ||
| Non-safety-net | 15.9 | 1 [Reference] |
| Safety-net | 15.7 | 0.99 [0.60, 1.62] |
| MULTIVARIATE WITH ALL PREDICTORS | ||
| ED payer mix | ||
| Non-safety-net | 15.9 | 1 [Reference] |
| Safety-net | 15.7 | 0.83 [0.52, 1.34] |
| Patient age (years) | ||
| 18–25 | 13.9 | 1 [Reference] |
| 26–64 | 18.6 | 1.54 [0.90, 2.62] |
| >64 | 13.2 | 1.07 [0.63, 1.80] |
| Patient sex | ||
| Female | 17.6 | 1 [Reference] |
| Male | 13.9 | 0.74 [0.57, 0.95] |
| Patient race/ethnicity | ||
| White, non-Hispanic | 13.4 | 1 [Reference] |
| Black/African American, non-Hispanic | 24.8 | 1.99 [1.26, 3.15] |
| Hispanic | 18.5 | 1.52 [1.01, 2.29] |
| Other | 12.0 | 0.72 [0.33, 1.55] |
| Clinician type | ||
| Resident/intern | 25.0 | 1.75 [1.16, 2.64] |
| NP/PA | 22.6 | 1.58 [0.99, 2.54] |
| Attending | 13.9 | 1 [Reference] |
| Missing/Unknown | 8.9 | 0.61 [0.24, 1.53] |
| Patient triage acuity (in minutes) | ||
| <15* | 12.5 | 1 [Reference] |
| 15–60 | 17.5 | 1.44 [1.10, 1.89] |
| 61–120 | 20.2 | 1.78 [1.11, 2.86] |
| >120 | 28.8 | 2.41 [1.24, 4.69] |
| Unknown | 14.2 | 1.22 [0.83, 1.80] |
| Hospital setting | ||
| Rural | 8.9 | 0.55 [0.23, 1.34] |
| Urban | 16.8 | 1 [Reference] |
| Hospital owner | ||
| Non-profit | 16.1 | 1 [Reference] |
| Government | 20.7 | 1.30 [0.81, 2.09] |
| Proprietary | 8.0 | 0.56 [0.29, 1.11] |
| Hospital location | ||
| Northeast | 23.5 | 1.74 [0.94, 3.24] |
| Midwest | 14.8 | 0.99 [0.58, 1.67] |
| South | 13.6 | 1 [Reference] |
| West | 12.4 | 0.85 [0.53, 1.36] |
NP = Nurse practitioner
PA = Physician assistant
Triage categories “Immediate” and “1–14 minutes” were combined for the purpose of this analysis
Table 4.
Multivariate adjusted odd of ED length of stay > 4 hours for discharged ED patients, NHAMCS 2008.
| Weighted Event Rate 24.4% |
Adjusted Odds Ratio [95% CI] |
|
|---|---|---|
| BIVARIATAE WITH ED PAYER MIX ONLY | ||
| ED payer mix | ||
| Non-safety-net | 24.4 | 1 [Reference] |
| Safety-net | 24.4 | 1.00 [0.82, 1.22] |
| MULTIVARIATE WITH ALL PREDICTORS | ||
| ED payer mix | ||
| Non-safety-net | 24.4 | 1 [Reference] |
| Safety-net | 24.4 | 1.03 [0.83, 1.27] |
| Patient age (in years) | ||
| 18–25 | 20.2 | 1 [Reference] |
| 26–64 | 24.4 | 1.25 [1.12, 1.40] |
| >64 | 30.3 | 1.77 [1.53, 2.04] |
| Patient sex | ||
| Female | 26.6 | 1 [Reference] |
| Male | 21.3 | 0.76 [0.69, 0.82] |
| Patient race/ethnicity | ||
| White, non-Hispanic | 22.3 | 1 [Reference] |
| Black/African American, non-Hispanic | 28.0 | 1.27 [1.09, 1.49] |
| Hispanic | 29.2 | 1.28 [1.06, 1.54] |
| Other | 23.2 | 0.94 [0.71, 1.26] |
| Clinician type | ||
| Resident/intern | 37.5 | 1.60 [1.31, 1.96] |
| NP/PA | 19.4 | 0.78 [0.64, 0.96] |
| Attending | 24.0 | 1 [Reference] |
| Other | 17.4 | 0.67 [0.41, 1.12] |
| Patient triage acuity (in minutes) | ||
| <15* | 30.7 | 1 [Reference] |
| 15–60 | 29.0 | 0.86 [0.70, 1.04] |
| 61–120 | 17.3 | 0.46 [0.36, 0.60] |
| >120 | 22.0 | 0.66 [0.48, 0.93] |
| Unknown | 19.5 | 0.55 [0.40, 0.75] |
| Hospital setting | ||
| Rural | 11.9 | 0.36 [0.28, 0.46] |
| Urban | 27.1 | 1 [Reference] |
| Hospital owner | ||
| Non-profit | 24.7 | 1 [Reference] |
| Government | 28.6 | 1.06 [0.76, 1.48] |
| Proprietary | 18.5 | 0.60 [0.43, 0.85] |
| Hospital location | ||
| Northeast | 28.9 | 1.10 [0.87, 1.40] |
| Midwest | 19.9 | 0.77 [0.59, 1.01] |
| South | 24.1 | 1 [Reference] |
| West | 25.5 | 0.93 [0.70, 1.22] |
NP = Nurse practitioner
PA = Physician assistant
Triage categories “Immediate” and “1–14 minutes” were combined for the purpose of this analysis
ED safety-net status is not independently associated with ED length of stay for patients admitted, discharged, transferred, or admitted to observation. This was true not only for all ED admissions and discharges, but for the subcategories tested as well (critical care, psychiatric, and routine) with the exception of psychiatric discharges (OR 1.67 [95%CI 1.02, 2.74]). Non-white race is independently associated with longer ED length of stay among admissions, a finding consistent with prior reports.9 Male sex is independently associated with shorter ED length of stay for psychiatric admissions and non-psychiatric discharges. Lower triage acuities are independently associated with prolonged ED length of stays among admissions and with shorter ED length of stays among those discharged. Clinician type (NP/PA or resident) is independently associated with prolonged ED lengths of stay for admitted (resident only), discharged patients (NP/PA and resident), and transferred (resident only) patients.
eTable 12 shows the results of the sensitivity analysis in which we incorporated patients who left without being seen or died in the ED into the admission category. This did not significantly alter the outcome (odds ratio for ED length of stay >8 hours in safety-net EDs was 0.83 [95% CI 0.52, 1.33] relative to non-safety-net EDs which is nearly identical to the results of the original model).
Comment
While many are concerned that performance measures, particularly those linked to payment (i.e. pay for performance), may ultimately penalize safety-net institutions who are already underfunded and care for a disproportionate volume of patients with poorer healthcare status, our findings suggest that those regarding ED length of stay will not.10 Our results show that both safety-net and non-safety-net EDs perform well on the ED length of stay goals that have been proposed, with median ED lengths of stay for both ED types well under 8 hours for admissions and 4 hours for discharges.3,4
Beyond this, however, we find that evaluating median LOS alone fails to tell the full story; the 90th percentile results are more revealing. Both safety-net and non-safety-net hospitals demonstrate poor performance with the ED length of stay goals when the 90th percentile is used. Lengths of stay among routine and critical care admissions at safety-net hospitals had a 90th percentile of nearly 10 hours each, and for psychiatric admissions were greater than 15 hours. The 90th percentile ED lengths of stay for these same dispositions were only slightly better at non-safety-net EDs. The 90th percentile ED lengths of stay among non-psychiatric discharges approached 6 hours regardless of safety-net status. The 90th percentile ED length of stay was more than 22 and 15 hours for psychiatric discharges at safety-net and non-safety-net institutions, respectively.
Previous literature demonstrates that the median ED length of stay has increased over time, approximately 3.5% per year.11 Our findings about the 90th percentile ED LOS are particularly concerning, given that this measure is often seen as a surrogate marker for crowding.12 It is plausible that ED length of stay for patients with certain psychiatric conditions, for example, is skewed by an abundance of intoxicated patients requiring time to sober before being able to be safely discharged. While this may be true, prior research has demonstrated significantly longer ED lengths of stay for psychiatric admissions as a result of a lack of psychiatric inpatient beds.13 In general, it is now widely accepted that ED boarding (the practice of admitted patients remaining in the ED due to lack of an available staffed inpatient bed), alternatively known as access block, plays the largest role in crowding in the ED.14 In other words, ED crowding is the result of hospital crowding. ED crowding has been associated with adverse effects such as the timeliness and quality of care, patient satisfaction, and increased rates of medication errors, in both pediatric and adult populations.15–24
Prolonged ED lengths of stay may be the consequence of poor throughput secondary to ED inefficiencies or the result of lack of output (i.e. no inpatient bed available for an admitted patient to move to). While currently there is no accepted ED length of stay target in the U.S., Graff suggested that 2 hours is “best practice”.25 ED throughput targets of 4 to 8 hours are currently being tested in Canada, New Zealand, and Australia.3,26,27 The ultimate cause of poor performance on ED throughput measures may differ between nations and individual institutions, and thus solutions to this problem may differ. Lessons learned from the implementation of perhaps the most aggressive attempt to regulate ED throughput, may be particularly valuable. In 2005, English EDs were mandated to have 98% of their patients leave within 4 hours of arrival (either discharged or in an inpatient hospital bed). Weber et al, in a qualitative study of the implementation of the “four hour rule”, found that success was dependent upon a collaborate approach between the ED and hospital leadership. Viewing the mandate as an ED rule rather than a hospital rule only encouraged conflict among staff. Additionally, focusing on the target rather than on the patient potentially places patients at risk.28
Our study has several limitations. Data collection for the NHAMCS survey is conducted by the U.S. Census Bureau. NHAMCS attempts to safeguard against the introduction of errors at this stage through requiring hospital staff to perform the actual visit sampling and data collection from the medical record. NHAMCS field staff conducts completeness checks on site before forwarding data and clerical staff performs edits upon receipt of the data in an attempt to reduce errors. The inclusion of self-reported data fields, such as insurance status, and variables with high non-response rates, such as race/ethnicity, may introduce inaccuracies. NHAMCS analysts use imputation in the case of missing variables that may contribute to inaccurate data as well.
This study includes the latest available data on U.S. ED visits (2008). It is unclear what effect, if any, the current recession and resultant increase in uninsured and Medicaid populations will have on ED visit volume or length of stay and their distribution among safety-net and non-safety-net EDs. Additionally, effects of the sweeping healthcare reform currently underway remain to be seen. Analysis of ED visit rates following healthcare reform in Massachusetts has been mixed.29
A critical piece of the implementation of payment rules based on performance metrics is careful consideration of its financial impact on safety-net institutions. Our findings show that compliance with proposed ED length of stay measures for admitted, discharged, transferred and observed patients do not differ between safety-net and non-safety-net hospitals, and could be a useful measure for assessing throughput across these institutions.
Supplementary Material
ACKNOWLEDGEMENTS
Funding/Support: This work was supported by the NIH/NCRR/OD UCSF-CTSI grant KL2 RR024130 (Dr. R. Hsia) and the Robert Wood Johnson Foundation Physician Faculty Scholars Program (Dr. R. Hsia).
Role of the Sponsor: The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Dr. Fee had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Drs. C. Fee and R. Hsia contributed equally to this work as senior authors.
Study concept and design: Drs. C. Fee, R. Hsia, and H. Burstin
Acquisition of data: Dr. R. Hsia and Ms. Maselli.
Analysis and interpretation of data: Ms. Maselli, Drs. C. Fee, R. Hsia, and H. Burstin
Drafting of the manuscript: Drs. C. Fee and R. Hsia.
Critical revision of the manuscript for important intellectual content: Drs. C. Fee, R. Hsia, H. Burstin, and Ms. Maselli.
Statistical analysis: Ms. Maselli and Drs. C. Fee and R. Hsia.
Obtained funding: Dr. R. Hsia
Study supervision: Drs. C. Fee and R. Hsia
Financial Disclosures: Dr. C. Fee has received consultancy fees from Google, and honoraria from the University of California, San Francisco Office of Continuing Medical Education for organizing and speaking at an annual CME course. Dr. H Burstin is a paid employee of the National Quality Forum.
Additional Contributions: None.
REFERENCES
- 1.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of US emergency department visits, 1997–2007. JAMA. 2010 Aug 11;304(6):664–670. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Quality Forum (NQF) National Voluntary Consensus Standards for Emergency Care: A Consensus Report. Washington, DC: NQF; 2009. [Google Scholar]
- 3.Ontario Ministry of Health and Long-Term Care. [Accessed July 25, 2011];Ontario Wait Times: Emergency Room Wait Times. 2010 http://www.health.gov.on.ca/en/pro/programs/waittimes/edrs/targets.aspx.
- 4.Accreditation Council for Graduate Medical Education. [Accessed July, 25, 2011];Emergency Medicine Guidelines. 2011 http://www.acgme.org/acWebsite/RRC_110/110_guidelines.asp.
- 5.Centers for Disease Control and Prevention. NHAMCS Scope and Sample Design. [Accessed July, 25, 2011];Scope and Sample Design. 2010 Available at: http://www.cdc.gov/nchs/ahcd/ahcd_scope.htm#nhamcs_scope.
- 6.Centers for Disease Control and Prevention. NHAMCS Estimation Procedures. [Accessed July 25, 2011];Ambulatory Health Care Data. 2010 http://www.cdc.gov/nchs/ahcd/ahcd_estimation_procedures.htm#nhamcs_procedures.
- 7.Owens PLMR, Stocks C. Healthcare Cost and Utilization Project (HCUP) 2010 [Google Scholar]
- 8.Burt CW, Arispe IE. Characteristics of emergency departments serving high volumes of safety-net patients: United States, 2000. Vital Health Stat. 2004 May;13(155):1–16. [PubMed] [Google Scholar]
- 9.Pines JM, Localio AR, Hollander JE. Racial disparities in emergency department length of stay for admitted patients in the United States. Acad Emerg Med. 2009 May;16(5):403–410. doi: 10.1111/j.1553-2712.2009.00381.x. [DOI] [PubMed] [Google Scholar]
- 10.Wang CJ, Conroy KN, Zuckerman B. Payment reform for safety-net institutions--improving quality and outcomes. N Engl J Med. 2009 Nov 5;361(19):1821–1823. doi: 10.1056/NEJMp0907656. [DOI] [PubMed] [Google Scholar]
- 11.Herring A, Wilper A, Himmelstein DU, et al. Increasing length of stay among adult visits to U.S. Emergency departments, 2001–2005. Acad Emerg Med. 2009 Jul;16(7):609–616. doi: 10.1111/j.1553-2712.2009.00428.x. [DOI] [PubMed] [Google Scholar]
- 12.Carr BG, Kaye AJ, Wiebe DJ, Gracias VH, Schwab CW, Reilly PM. Emergency department length of stay: a major risk factor for pneumonia in intubated blunt trauma patients. J Trauma. 2007 Jul;63(1):9–12. doi: 10.1097/TA.0b013e31805d8f6b. [DOI] [PubMed] [Google Scholar]
- 13.Chang G, Weiss AP, Orav EJ, et al. Hospital Variability in Emergency Department Length of Stay for Adult Patients Receiving Psychiatric Consultation: A Prospective Study. Ann Emerg Med. 2011 Jan 10; doi: 10.1016/j.annemergmed.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 14.Moskop JC, Sklar DP, Geiderman JM, Schears RM, Bookman KJ. Emergency department crowding, part 1--concept, causes, and moral consequences. Ann Emerg Med. 2009 May;53(5):605–611. doi: 10.1016/j.annemergmed.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 15.Fee C, Weber EJ, Maak CA, Bacchetti P. Effect of emergency department crowding on time to antibiotics in patients admitted with community-acquired pneumonia. Ann Emerg Med. 2007 Nov;50(5):501–509. 509 e501. doi: 10.1016/j.annemergmed.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 16.Pines JM, Localio AR, Hollander JE, et al. The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Ann Emerg Med. 2007 Nov;50(5):510–516. doi: 10.1016/j.annemergmed.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 17.Pines JM, Iyer S, Disbot M, Hollander JE, Shofer FS, Datner EM. The effect of emergency department crowding on patient satisfaction for admitted patients. Acad Emerg Med. 2008 Sep;15(9):825–831. doi: 10.1111/j.1553-2712.2008.00200.x. [DOI] [PubMed] [Google Scholar]
- 18.Sills MR, Fairclough D, Ranade D, Kahn MG. Emergency department crowding is associated with decreased quality of care for children with acute asthma. Ann Emerg Med. 2011 Mar;57(3):191–200. e197. doi: 10.1016/j.annemergmed.2010.08.027. [DOI] [PubMed] [Google Scholar]
- 19.Pines JM, Prabhu A, Hilton JA, Hollander JE, Datner EM. The effect of emergency department crowding on length of stay and medication treatment times in discharged patients with acute asthma. Acad Emerg Med. 2010 Aug;17(8):834–839. doi: 10.1111/j.1553-2712.2010.00780.x. [DOI] [PubMed] [Google Scholar]
- 20.Pines JM, Shofer FS, Isserman JA, Abbuhl SB, Mills AM. The effect of emergency department crowding on analgesia in patients with back pain in two hospitals. Acad Emerg Med. 2010 Mar;17(3):276–283. doi: 10.1111/j.1553-2712.2009.00676.x. [DOI] [PubMed] [Google Scholar]
- 21.Kulstad EB, Sikka R, Sweis RT, Kelley KM, Rzechula KH. ED overcrowding is associated with an increased frequency of medication errors. Am J Emerg Med. 2010 Mar;28(3):304–309. doi: 10.1016/j.ajem.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 22.Mills AM, Baumann BM, Chen EH, et al. The impact of crowding on time until abdominal CT interpretation in emergency department patients with acute abdominal pain. Postgrad Med. 2010 Jan;122(1):75–81. doi: 10.3810/pgm.2010.01.2101. [DOI] [PubMed] [Google Scholar]
- 23.Mills AM, Shofer FS, Chen EH, Hollander JE, Pines JM. The association between emergency department crowding and analgesia administration in acute abdominal pain patients. Acad Emerg Med. 2009 Jul;16(7):603–608. doi: 10.1111/j.1553-2712.2009.00441.x. [DOI] [PubMed] [Google Scholar]
- 24.Pines JM, Pollack CV, Jr, Diercks DB, Chang AM, Shofer FS, Hollander JE. The association between emergency department crowding and adverse cardiovascular outcomes in patients with chest pain. Acad Emerg Med. 2009 Jul;16(7):617–625. doi: 10.1111/j.1553-2712.2009.00456.x. [DOI] [PubMed] [Google Scholar]
- 25.Graff L, Stevens C, Spaite D, Foody J. Measuring and improving quality in emergency medicine. Acad Emerg Med. 2002 Nov;9(11):1091–1107. doi: 10.1111/j.1553-2712.2002.tb01563.x. [DOI] [PubMed] [Google Scholar]
- 26.Commonwealth of Australia. A national health and hospitals network: further investments in Australia's health. Australian Government; 2010. [Google Scholar]
- 27.New Zealand Ministry of Health. [Accessed July 25, 2011];Emergency Departments. 2011 http://www.moh.govt.nz/emergencydepartments.
- 28.Weber EJ, Mason S, Carter A, Hew RL. Emptying the corridors of shame: organizational lessons from England's 4-hour emergency throughput target. Ann Emerg Med. 2011 Feb;57(2):79–88. e71. doi: 10.1016/j.annemergmed.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 29.Smulowitz P, Landon BE, Burke L, Baugh C, Gunn H, Lipton R. Emergency department use by the uninsured after health care reform in Massachusetts. Intern Emerg Med. 2009 Dec;4(6):501–506. doi: 10.1007/s11739-009-0313-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.