Abstract
The current pilot study evaluated feasibility, acceptability, and initial efficacy of a therapeutic Interactive Voice Response (IVR) system (“The Recovery Line”) for patients receiving methadone maintenance who continue to use illicit drugs. Patients were randomized (N=36) to four weeks of Treatment-as-Usual (TAU) or Recovery Line plus TAU. Ratings of The Recovery Line were high and remained stable throughout the study. However, despite instructions and reminders, patients used substantially less than the recommended daily use (<10 days of 28). Patients were more likely to report abstinence for opioids and cocaine on days they used the Recovery Line (p = .01) than those they did not. Conditions did not differ significantly on patient satisfaction, urine screen outcomes, or coping efficacy. As with other computer-based treatments, findings suggest the Recovery Line is acceptable and feasible. However, additional methods to increase patient utilization of automated systems and larger clinical trials are needed.
Keywords: Computer-based Treatment, IVR, Methadone Treatment, Opioid Related Disorders, Mobile Treatment
Automated, computer-based interventions have shown promise in treating substance use disorders. Such systems extend the effectiveness of patient self-management by providing motivational enhancement, assessment and feedback, accurate and detailed education, and specific skills training. These systems differ from electronic or “E-therapy” in which therapists provide counseling remotely (web-chat, text, email, or phone). Fully automated systems offer a number of potential advantages, including low cost, consistent delivery, and greater accessibility and availability of treatment, and increased flexibility of scheduling and convenience. Studies of computer-based treatments have found high user acceptance and utilization, and automated systems may even be preferable to one-on-one therapy among clients who dislike therapy or have concerns about confidentiality.
Automated computer-based systems can be mobile and delivered via cell phones or other devices, providing immediate therapeutic intervention from any place at any time. Individuals can use the system to practice skills in their own environment and can repeat this training frequently at their own pace. Easily accessible, real-time interventions may be helpful for less motivated or more difficult-to-treat populations, since these interventions require less effort to attend appointments and retrospectively recall specific behavior for therapeutic discussion. Some mobile interventions utilize sophisticated technologies such as smartphones and include applications and mobile websites, while others use traditional phone technology for delivery using Interactive Voice Response (IVR) systems. With IVR systems patients use key pad responses or voice commands to choose menu options, respond to prompts, and answer assessments. Many studies of IVR technology have been limited to patient reminders, brief assessments, and evaluations of self-monitoring, but more recently Therapeutic IVR (TIVR) technology has increased in flexibility and sophistication and incorporates more complex treatment components including self-monitoring, goal setting and coping skills rehearsal. Therapeutic IVR can effectively augment treatment for a range of psychiatric and behavioral health problems such as obsessive-compulsive disorder, depression, chronic pain, and medication adherence. In addition, TIVR systems show potential promise to augment brief interventions for substance users, including non-treatment seekers in primary care settings. However, although brief IVR systems have been shown to be acceptable and feasible to a range of patients, to our knowledge only two studies evaluated a TIVR with treatment seeking patients with problematic drug or alcohol use. Mosavel found that patient’s system use was heavily skewed with most patients having limited use and a few using extensively. Rose et al. evaluated TIVR following group CBT for alcohol use disorders and found high acceptability and ease of use as well as improved abstinence, self-efficacy, and coping skills efficacy compared to baseline values. However, both studies did not include a comparison condition.
Over the past 10 years, treatment admissions for opioid dependence have increased by fifty percent, in large part due to abuse of prescription pain relievers. Many programs, including those involved in the current study, have noted a substantial increase in patient volume with decreased reimbursement levels and therefore decreased staffing and higher caseloads. The dramatic increase in dependence has led to treatment need that exceeds the current system. Thus, there is a clear need to expand the reach and variety of therapeutic interventions available, especially those in methadone maintenance who typically receive limited face-to-face counseling. Technological interventions provide a means to extend the scarce treatment resources available, however, their feasibility, acceptability and efficacy must be demonstrated. TIVR represents an approach that has the potential to be more accessible, flexible, and cost effective than counseling and other potential technological interventions. The current pilot study was designed to evaluate feasibility, acceptability, and initial efficacy of a TIVR system (“The Recovery Line”) for opioid dependent patients receiving methadone maintenance who were continuing to use illicit drugs while enrolled in treatment.
Materials and Methods
Participants
Patients were recruited from November 2010 through July 2011 at the APT Foundation in New Haven, CT through clinic posters and flyers, brochures provided to counselors, and word-of-mouth. Seventy-five patients enrolled in methadone maintenance treatment who reported use of illicit drugs in the past 30 days expressed initial interest and participated in a brief screening. Exclusion criteria were 1) current suicide or homicide risk; 2) a DSM-IV current psychotic or bipolar disorder; 3) involvement in another treatment study; 4) inability to read or understand English; 5) a life-threatening or unstable medical problem. Seventeen (23%) were ineligible (16 for active psychiatric disorder, 1 for medical problems) and 12 (16%) who were potentially eligible refused treatment (1) or failed to return for consent (11). Forty-six patients signed informed consent and were further evaluated for eligibility. Five patients were excluded for current psychotic or bipolar disorder, one for an unstable medical problem, one was in another study, one withdrew, and two failed to complete the baseline assessment, yielding a final treatment comparison sample of 36.
Design and Procedures
Eligible participants (n = 36) were randomly assigned to four weeks of either Treatment-as-Usual (TAU, n = 18) or the Recovery Line plus Treatment-as-Usual (RL+TAU, n = 18). Participants completed weekly assessments and a comprehensive end-of-treatment assessment. Urine samples for toxicology analysis were also collected during weekly assessments. Participants received $20 per week as an incentive for completing weekly assessments and providing a urine sample. The study was approved by the Human Investigation Committee of Yale University School of Medicine the study was conducted in accordance with the Helsinki Declaration of 1975.
Measures
Patients assigned to the Recovery Line completed a brief interview each week to evaluate characteristics of the system patients liked and disliked, and any technical difficulties with the system. The interview was developed for this study and included three 5-point Likert scale items evaluating patient interest, perceived efficacy, and ease of use of the Recovery Line from “Not at all” to “Extremely” (e.g., “How interesting does the Recovery Line sound to you?, How helpful was the Recovery Line? How easy to use was the Recovery Line?). An additional single item 5-point Likert scale evaluated patient satisfaction with their continuing methadone treatment for patients in both conditions.
The Structured Clinical Interview for DSM-IV (SCID) was used to assess psychotic and mood disorders for exclusion criteria. Retention was evaluated as the number of weeks participants remained in the study. Urine samples for toxicology analyses were performed using a one-step immunochromatographic test (Redwood Toxicology Laboratory, Santa Rosa, CA) that included morphine/opiates (> 300 ng/ml cuttoff), oxycodone (> 100 ng/ml cuttoff), cocaine (> 300 ng/ml cuttoff), benzodiazepine (> 300 ng/ml cuttoff), methamphetamine (> 500 ng/ml cuttoff), and THC (> 50 ng/ml cuttoff). Missing urines were coded as positive for opioids. The proportion of urines negative for all drugs tested, for opioids (opiates and oxycodone), and for cocaine were computed. Self-reported drug use was assessed using Time Line Follow Back methodology. Coping skill effectiveness was evaluated with the Effectiveness of Coping Behaviors Inventory (ECBI). Scores on the ECBI have been found to predict post-treatment abstinence for alcohol dependent inpatients, and to improve for patients receiving a TIVR intervention for alcohol use disorders.
Treatments
Treatment-as-Usual (TAU)
The proposed system was meant to serve as an enhancement of current services being delivered, which included the requirement to attend one individual session per month and encouragement to attend open access groups (with 10 or more typically available Monday-Friday) covering a range of topics, including introduction to methadone, weekend planning, overdose planning, and spirituality. These are the services provided in the standard care comparison condition.
The Recovery Line plus Treatment-as-Usual (RL+TAU)
The RL+TAU condition involved a TIVR orientation session, four weeks of 24-hour access to the system, a patient notebook with summary Recovery Line information, and a weekly reminder from staff to use the system. A technical assistance line for system problems was available from 8:30-4:30, M-F and was staffed by the study Research Assistant.
Recovery Line Development
The Recovery Line system was developed for patients to use in their own environment and obtain immediate assistance, training, and support for improved coping. Modules were designed to be brief (<15 minute) and easy to understand. The system was developed using a 5-stage iterative process prior to efficacy testing which included 1) content generation based on CBT theory and principals, 2) expert review for language appropriateness and comprehensibility, 3) treatment provider acceptability feedback, 4) experienced patient acceptability feedback, and 5) target patient feasibility and acceptability testing. We set apriori criteria to evaluate acceptability and feasibility based on amount of system contact (at least 30 minutes of call time over one week of access) and patient-rated interest, helpfulness and ease of system use [50% ratings of at least 4 (out of 5) for interest, helpfulness and ease of use]. Prior feasibility pilot testing met the apriori criteria of at least 4 for interest (67%), helpfulness (50%), and ease of use (92%), and patients used the system for a mean of 82 minutes over one week. Based on system modifications, acceptability and feasibility measures from the current trial were expected to meet or exceed these values.
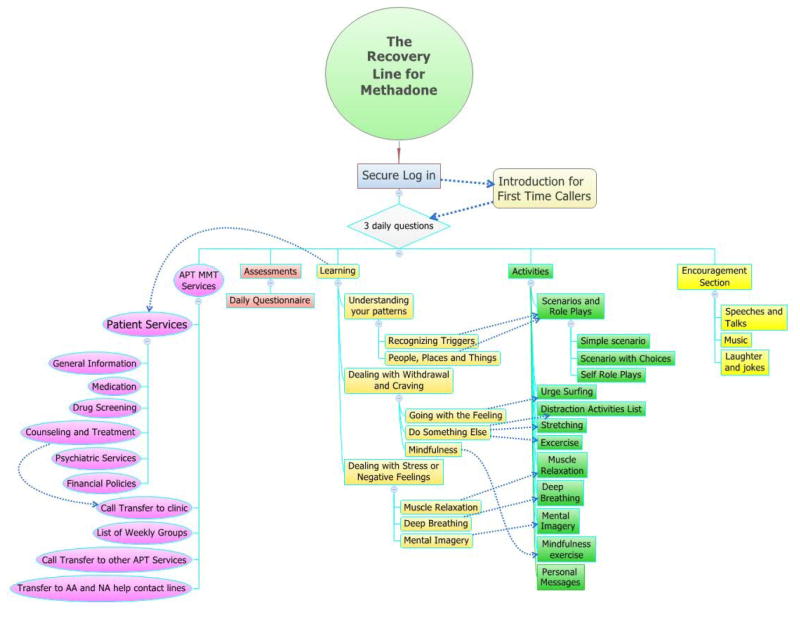
The core structure of the system was based on cognitive behavioral therapy from the NIDA-published manual for cocaine dependence and our prior work with CBT for opioid dependent patients in buprenorphine/naloxone treatment. As can be seen in Figure 1, system components included 1) Self-monitoring, 2) Coping with urges and cravings, 3) Identifying/avoiding risky situations, and 4) Managing moods and stress. For self-monitoring, a daily questionnaire of three items was included immediately upon system log in (“How are you doing?” “Have you taken your methadone today?” “Did you used illicit drugs since your last call?”). A more extensive assessment of current emotions and drug use situations was also developed which suggested modules based on problems identified in the assessment.
Figure 1.
Schematic of the Recovery Line for Methadone.
The other CBT components were separated into brief “Learning” and “Activity” modules. Learning modules provided straightforward didactic descriptions (e.g., urge surfing). Assessments at the end of the learning modules were used to confirm patient understanding and provide alternative explanations for incorrect responses to improve patient understanding. Activity modules included direct guidance for skills (e.g., deep breathing, guided exercise), and role-plays for concept learning (e.g., understanding patterns, avoiding risky situations). Role-plays present scenarios in three layers of increasing interactivity. For this “Learn, Choose, Do” approach, patients were presented different example scenarios in which they, 1) heard the correct choice provided, 2) selected between multiple choice options, and 3) recorded, played back and rated their own response. Patients received positive feedback for correct responses, and corrective feedback and suggestions for improving responses for incorrect responses. Additional system features were designed to maintain user interest and increase utilization and included recorded speeches, inspirational messages, jokes, laughter and music. Patients could choose to provide ratings at the end of any module.
Patient orientation and reminders
Following randomization, patients were given a 30 to 45 minute system orientation by a research assistant in a private office which included a Recovery Line notebook, an overview of the content and purpose of the system, instruction on how to log-in, and then 10–15 minutes of access to become familiar with the system. To help patients work calling into their daily routines, they selected a 2-hour call window during which they would plan to make daily calls. The call window served as a guideline, thus calling during the window was not required. The notebook and an accompanying wallet-size card included general information on the system, access numbers, and commonly used commands. At each weekly assessment, patients were reminded to use the system and seek help for any technical problems. Patients who did not call the system were contacted by the research assistant once per week to recommend system use.
Data analysis
Primary outcome measures to evaluate feasibility and acceptability were overall patient satisfaction, study retention, and RL+TAU patient ratings of the Recovery Line interest, perceived efficacy, and ease of use. Secondary outcomes of initial efficacy were urine results, self-reported substance use, and coping skills effectiveness. Due to the small sample size, we set p < .05 for “significant” results, and p < .10 for “marginally significant” results. Univariate comparisons of patients were conducted using chi-square tests for categorical variables and t-tests for interval and continuous variables. For outcomes with repeated measures, we used repeated-measures ANOVA for data with no-missing values (urine toxicology tests). For data with missing values (number of days of substance use each week) we used mixed model ANOVA with autoregressive 1 correlation structure since such models are designed for unbalanced repeated measures with missing data. Since there were marginally significant group differences in baseline characteristics that might have contributed to treatment outcome (sex, employment, and cocaine use), we evaluated differences in assigned condition both unadjusted and adjusted for baseline differences using analysis of covariance (ANCOVA). Retention was examined using Kaplan-Meier survival analysis on weeks in treatment. An exploratory analysis was conducted to evaluate the relationship between patient call data and self-reported drug use on the same day for patients in the RL+TAU condition. We used autoregressive General Estimating Equations (GEE) including patient as a random variable and controlling for day in treatment. All analyses made use of SPSS 19.0.
Results
Demographic and baseline characteristics are presented in Table 1. There were no statistically significant differences between the two treatment conditions, but several trends were controlled through covariance adjustments. Assessment completion was high with 88% of weekly assessments completed, including requested urine samples, and 89% of end of treatment assessments completed.
Table 1.
Demographic and clinical characteristics of methadone maintenance patients assigned to the Recovery Line plus treatment-as-usual (RL+TAU) or to treatment-as-usual (TAU) only.
| Characteristic | RL+TAU n = 18 | TAU n = 18 | p |
|---|---|---|---|
| Age, years, mean, (SD) | 40.3 (10.8) | 42.3 (9.5) | .55 |
| % Male, (n) | 28% (5) | 56% (10) | .09 |
| Race | .76 | ||
| %White, (n) | 67% (12) | 50% (9) | |
| % Black, (n) | 22% (4) | 33% (6) | |
| % Other, (n) | 11% (2) | 17% (3) | |
| % Employed (part or full), (n) | 0 (0) | 17% (3) | .07 |
| % High School or greater, (n) | 78% (14) | 83% (15) | .67 |
| Monthly income, $, mean (SD) | 152 (282) | 421 (711) | .15 |
| % Never married, (n) | 56% (10) | 33% (6) | .18 |
| Opioid dependence, years, mean, (SD) | 14.0 (12.6) | 14.7 (13.4) | .88 |
| % Prescription Drug Use, (n) | 11% (2) | 6% (1) | .66 |
| % History intravenous drug use, (n) | 33% (6) | 33% (6) | 1.0 |
| Days of opioid use in prior 30 days, mean (SD) | 4.6 (7.4) | 4.9 (9.6) | .90 |
| Days of cocaine use in prior 30 days, mean (SD) | 6.1 (8.8) | 11.3 (10.3) | .11 |
| Months of current methadone treatment, mean (SD) | 24.2 (22.9) | 19.2 (16.6) | .45 |
| Number of time in drug treatment before current treatment, mean (SD) | 6.2 (7.8) | 4.9 (4.4) | .55 |
| Number of times in methadone treatment before current treatment, mean (SD) | 2.4 (1.8) | 1.9 (0.9) | .35 |
Ratings of Acceptability and Perceived Efficacy
Patients completed three ratings (from 1–5) of the Recovery Line (interest, perceived efficacy, and ease of use) at each of the weekly assessments. Ratings did not change over the four weeks of study. Mean interest at the end of the study was 3.6 (SD =0.9), mean perceived efficacy was 3.7 (SD = 1.0), and mean ease of use was 4.8 (SD = 0.4). Ratings exceeded the apriori criteria of >50% ratings of 4 or 5 used in the development phase for all three measures (56% for interest, 61% for perceived efficacy, and 100% for ease of use). There were only 3 calls for technical assistance, two for help with logging in, and one for a problem with voice responses.
Recovery Line Use
Although intended for daily use, patients in the RL+TAU condition called the system on a mean of 9.9 days (SD=6.0) of the 28 study days, made a mean of 14.2 calls (SD=11.6), for a total of 121.9 (SD=84.3) mean total minutes of contact time. Only 27% of calls were made during the patient’s selected two hour call window. Most calls were brief (M = 9.3 minutes, SD=3.2) and outside clinic hours (58%). Sixty-one percent (11/18) of patients accessed modules in all of the four primary domains (self-monitoring, coping with urges and cravings, identifying/avoiding risky situations, and managing moods and stress). All patients (100%) accessed self-monitoring modules, 89% (16/18) accessed coping with urges and cravings modules, 78% (14/18) accessed identifying/avoiding risky situations, and 89% (16/18) accessed managing moods and stress modules. In addition, all patients (100%) accessed the encouragement section. Of 46 modules for which patients provided in-call ratings, 57% were rating 4 or 5 (M = 3.6, SD = 1.4).
An exploratory analysis was conducted to evaluate the relationship between patient call data and self-reported drug use on the same day for patients in the RL+TAU condition. GEE analyses indicated that patients were more likely to report abstinence for opioids and cocaine on days they used the Recovery Line (45%) than those that did not (34%; p .01).
Methadone Treatment Satisfaction
Ratings of satisfaction with methadone treatment (1 to 5) at the end of the study were high (M = 4.3, SD = 1.0) and did not differ between treatment conditions (RL+TAU, M = 4.1, SD = 1.2, TAU only, M = 4.4, SD = 0.8, p = .57 unadjusted, p = .62 adjusted).
Study Retention
No patients dropped out or voluntarily withdrew from the study. Three patients in the RL+TAU condition were transferred to another treatment clinic by the methadone clinic and one patient was incarcerated. All patients in the TAU condition remained in the study for the full four weeks (M = 4.0), which was marginally longer than patients in RL+TAU (M = 3.6, p = .07, unadjusted and p = .30 adjusted).
Substance use
For self-reported opioid use there was no significant main effect for condition, time, nor their interaction (all p’s > .33). For cocaine use, the interaction of condition by time was marginally significant (p = .054 for the adjusted test and p = .10 for the adjusted test). Weekly mean values suggested that differences between conditions were greater in weeks one (1.6 for RL+TAU and 2.9 for TAU, d = .54) and four (1.1 for RL+TAU and 2.8 for TAU, d = .69). The main effect of condition was marginally significant for the unadjusted test (p = .10, 1.5 for RL+TAU and 2.6 for TAU, d = .47) and significant for the adjusted test (p = .047, d = .51). There was no significant main effect of time.
Cannabis was the only other self-reported drug, but was reported with insufficient frequency to evaluate. There was no difference between conditions on proportion of urine screens negative for opioids (0.79 for RL+TAU and 0.75 for TAU, p = .73, d = .11, unadjusted, p = .67, d= .17, adjusted). Similarly for the proportion of urine screen negative for cocaine, there was no significant difference between conditions, although the mean values for the RL+TAU condition were nominally higher than those of the TAU only condition (0.44 for RL+TAU and 0.28 for TAU, p = .20, d = .44, unadjusted, p = .13, d= .53, adjusted).
Methadone Counseling
Conditions did not differ on the number of counseling session beyond the required minimum (RL+TAU, M= 3.3, SD = 9.5, TAU only, M = 1.0, SD = 1.0, p = .30 unadjusted, p = .72 adjusted), nor on the number of additional support groups attended (i.e., NA, AA: RL+TAU, M = 2.0, SD = 6.5, TAU only, M = 1.0, SD = 2.9, p = .56 unadjusted, p = .62 adjusted).
Coping Skills
Internal reliability of the ECBI at baseline was high (Chronbach’s α=.95). ECBI scores were compared pre-treatment to post-treatment across conditions. There were no significant time (p = .92), condition (p = .39), nor interaction effects (p = .15, d = .38), although the RL+TAU scores nominally improved (0.67 to 0.82) compared to a decline for TAU only (0.67 to .54). The adjusted analysis showed the same pattern of non-significant results. However, ECBI scores were significantly correlated with reduced self-reported cocaine use (r = .41, p = .03).
Discussion
Findings from the randomized pilot study suggested that the Recovery Line is a promising ancillary intervention for methadone patients with ongoing drug use and warrants study in a larger clinical trial. Patients used the system on almost 10 of the 28 days and found the system interesting, helpful, and easy to use, and rated most modules positively. Calls were generally brief (< 10 minutes), but most patients accessed the majority of the content domains. Most patients who were potentially eligible participated in the study (84%), and no patients dropped out or voluntarily withdrew. An advantage of the current TIVR system is that call logs provide detailed records of patient module access which could be used to more finely evaluate how use of specific coping skills modules may be associated with drug use behavior over time and potentially in real-time. Although ratings of interest and perceived utility were good, there is room to improve. Similarly, despite instructions during the orientation and reminders during treatment to use the Recovery Line on a daily basis, only a minority used the system on a close to daily basis. Many patients reported that they had forgotten to use it. This appears to be a common characteristic of patient driven automated systems. Although patients report liking such systems, many fail to use them at recommended levels (Mosavel, 2005;. This suggests that reminder calls or texts, or scheduled daily calls to the patient may increase patient use. Additional methods to increase patient utilization while maintaining patient satisfaction and efficacy will be a focus of future work by our group.
Although measures of acceptability and feasibility were generally positive, clinical outcome findings in this small, randomized trial were mixed. For self-reported drug use there were marginally significant reductions in cocaine use of 1.7 days/week, but not other drugs. Similarly, patients in the Recovery Line condition were more likely to report abstinence on days they used the line than those they did not. Urine screen results were not significantly different between conditions, although they were in the expected direction for cocaine, and effect sizes were moderate to large (d’s ≥ .44). Given that cocaine use is often associated with poorer treatment outcome and greater dropout rates in methadone maintenance, and that limited treatment options are available for continued use in methadone maintenance, the findings suggest that additional evaluation with a larger sample size is warranted. This is particularly encouraging given the short (4-week) duration of Recovery Line Use and that patients used the system less than was anticipated.
The current findings are consistent with other positive results of computer-based interventions for substance abuse. Studies evaluating brief interventions for alcohol and tobacco have shown small to moderate effect sizes. Carroll and colleagues found that bi-weekly computerized CBT4CBT provided in standard substance abuse clinics improved substance use outcomes (urine screen and continued abstinence) compared to standard treatment alone, and improvements were maintained after treatment. In a study of opioid-dependent patients receiving buprenorphine, Bickel and colleagues found that computer-based behavioral skills training plus contingency management showed similar efficacy to counselor provided skills training plus contingency management. Although the current study uses IVR technology, the Recovery Line is more similar to these sophisticated computer-based interventions that include interactive therapeutic components that the brief self-monitoring and assessment IVR interventions. To our knowledge, the current study represents the only evaluation of a computer-based treatment system with therapeutic modules for continued drug use among patients in methadone maintenance.
Several limitations of the study should be noted. First, the study was designed as a pilot trial to evaluate feasibility, acceptability, and initial efficacy and thus the sample size was small, with power only to detect large effects. Second, despite random assignment, there were several marginally significant differences on baseline variables that may have affected treatment outcome, including gender, employment and cocaine use. We attempted to control for these differences statistically, which provided similar findings to the unadjusted results, but controlling via randomized stratification would be preferred, requiring a larger sample size. There was also a marginally significant difference in retention with three patients in the Recovery Line condition being transferred to another methadone treatment program and one being incarcerated. Although patients did not refuse the Recovery Line or drop out of the treatment condition, the differential retention may have affected other outcomes. A final limitation was the lack of follow-up assessment following the intervention. Since continued skill training effects are often noted following the end of counseling, future studies should include a follow-up period to evaluate possible emergent effects. It is also possible that treatment effects may not be as durable as other psychosocial treatments, which could lead to loss of treatment gains over time. However, given the relatively low cost of the Recovery Line, it may be feasible to provide patients with continued access rather than providing a specific access termination. In addition, alternative models of delivery and implementation for automated interventions should be explored. The addition of the non-automated components such as weekly assessments and reminder calls may limit generalizability to community settings. Research on implementation of automated systems by treatment providers is necessary for translation to treatment settings.
The findings from the current trial suggest that automated ancillary treatment for methadone maintenance is feasible and acceptable to patients and may positively affect clinical outcomes. This type of intervention can support methadone treatment and provide patients the opportunity for easily accessible, on-demand therapeutic contact beyond standard care. In addition to treatment of continued drug use as evaluated in the current pilot, the Recovery Line may be helpful for initiating and maintaining abstinence, treatment retention, and relapse prevention, and additional research of these uses is needed. Treatment admissions for opioid agonist treatment in the U.S. have increased dramatically in the past 10 years, and access to opioid agonist treatment is rapidly expanding internationally. Thus, there is a clear need for readily available psychosocial services, especially in more rural areas. Since IVR technologies are easily scalable, the Recovery Line has the potential to be easily and rapidly implemented in a variety of domestic as well as international contexts to provide a low-cost, accessible intervention to support and enhance opioid dependence treatment.
Acknowledgments
The research was supported by the National Institute on Drug Abuse Grants K01 DA022398 (B.M. & T.F.), RO1 DA019511 and R01 DA020576 (C.C., & D.F.), R01 DA025991 (D.F.), K24DA000445 (R.S.), K23 DA024050 (D.B.), P50 DA09241 (SB) and through the State of Connecticut, Department of Mental Health and Addiction Services support of the Connecticut Mental Health Center (B.M.). This study was presented in part at the 2011 annual Convention of the American Psychological Association in Washington, D.C.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Baer L, Greist JH. An interactive computer-administered self-assessment and self-help program for behavior therapy. Journal of Clinical Psychiatry. 1997;58:23–28. [PubMed] [Google Scholar]
- Bender BG, Apter A, Bogen DK, Dickinson P, Fisher L, Wamboldt FS, Westfall JM. Test of an interactive voice response intervention to improve adherence to controller medications in adults with asthma. Journal of the American Board of Family Medicine: JABFM. 2010;23:159–165. doi: 10.3122/jabfm.2010.02.090112. [DOI] [PubMed] [Google Scholar]
- Bewick BM, Trusler K, Barkham M, Hill AJ, Cahill J, Mulhern B. The effectiveness of web-based interventions designed to decrease alcohol consumption--a systematic review. Preventive Medicine. 2008;47:17–26. doi: 10.1016/j.ypmed.2008.01.005. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Christensen DR, Marsch LA. A review of computer-based interventions used in the assessment, treatment, and research of drug addiction. Substance Use & Misuse. 2011;46:4–9. doi: 10.3109/10826084.2011.521066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Marsch LA, Buchhalter AR, Badger GJ. Computerized behavior therapy for opioid-dependent outpatients: a randomized controlled trial. Experimental & Clinical Psychopharmacology. 2008;16:132–143. doi: 10.1037/1064-1297.16.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budman SH. Behavioral health care dot-com and beyond: Computer-mediated communications in mental health and substance abuse treatment. American Psychologist. 2000;55:1290–1300. [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Elliott JC, Bolles JR, Carey MP. Computer-delivered interventions to reduce college student drinking: A meta-analysis. Addiction. 2009;104:1807–1819. doi: 10.1111/j.1360-0443.2009.02691.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM. A cognitive-behavioral approach: Treating cocaine addiction. Rockville, MD: NIDA; 1998. [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Nuro KF, Rounsaville BJ. Computer-assisted delivery of cognitive-behavioral therapy for addiction: a randomized trial of CBT4CBT. American Journal of Psychiatry. 2008;165:881–888. doi: 10.1176/appi.ajp.2008.07111835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Rounsaville BJ. Enduring effects of a computer-assisted training program for cognitive behavioral therapy: A 6-month follow-up of CBT4CBT. Drug & Alcohol Dependence. 2009;100:178–181. doi: 10.1016/j.drugalcdep.2008.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ, Nich C, Gordon LT, Wirtz PW, Gawin F. One year follow-up of psychotherapy and pharmacotherapy for cocaine dependence: Delayed emergence of psychotherapy effects. Arch Gen Psychiatry. 1994;51:989–997. doi: 10.1001/archpsyc.1994.03950120061010. [DOI] [PubMed] [Google Scholar]
- Cavanagh K, Shapiro DA. Computer treatment for common mental health problems. Journal of Clinical Psychology. 2004;60:239–251. doi: 10.1002/jclp.10261. [DOI] [PubMed] [Google Scholar]
- Dyches H, Alemagno S, Llorens SA, Butts JM. Automated telephone-administered substance abuse screening for adults in primary care. Health Care Management Science. 1999;2:199–204. doi: 10.1023/a:1019000231214. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders - Clinician Version (SCID) Washington, D.C: American Psychiatric Association Press, Inc; 1997. [Google Scholar]
- Greist JH, Marks IM, Baer L, Kobak KA, Wenzel KW, Hirsch M, Clary CM. Behavior therapy for obsessive-compulsive disorder guided by a computer or by a clinician compared with relaxation as a control. Journal of Clinical Psychiatry. 2002;63:138–145. doi: 10.4088/jcp.v63n0209. [DOI] [PubMed] [Google Scholar]
- Hardin JW, Hilbe JM. Generalized Estimating Equations. Boca Roton, FL: Chapman & Hall; 2003. [Google Scholar]
- Kaminer Y, Litt MD, Burke RH, Burleson JA. An interactive voice response (IVR) system for adolescents with alcohol use disorders: a pilot study. American Journal on Addictions. 2006;1:122–125. doi: 10.1080/10550490601006121. [DOI] [PubMed] [Google Scholar]
- Klein AA, Slaymaker VJ, Dugosh KL, McKay JR. Computerized continuing care support for alcohol and drug dependence: a preliminary analysis of usage and outcomes. Journal of Substance Abuse Treatment. 2012;42:25–34. doi: 10.1016/j.jsat.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kranzler HR, Abu-Hasaballah K, Tennen H, Feinn R, Young K. Using daily Interactive Voice Response technology to measure drinking and related behaviors in a pharmacotherapy study. Alcoholism: Clinical & Experimental Research. 2004;28:1060–1064. doi: 10.1097/01.alc.0000130806.12066.9c. [DOI] [PubMed] [Google Scholar]
- Kypri K, Saunders JB, Gallagher SJ. Acceptability of various brief intervention approaches for hazardous drinking among university students. Alcohol & Alcoholism. 2003;38(6):626–628. doi: 10.1093/alcalc/agg121. [DOI] [PubMed] [Google Scholar]
- Litman GK, Stapleton J, Oppenheim AN, Peleg M, Jackson P. Relationship between coping behaviors, their effectiveness and alcoholism relapse and survival. British Journal of Addiction. 1984;79:283–291. doi: 10.1111/j.1360-0443.1984.tb00276.x. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E. Individualized assessment and treatment program for alcohol dependence: results of an initial study to train coping skills. Addiction. 2009;104:1837–1838. doi: 10.1111/j.1360-0443.2009.02693.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maremmani I, Pani P, Mellini A, Pacini M, Marini G, Lovrecic M, Shinderman M. Alcohol and cocaine use and abuse among opioid addicts engaged in a methadone maintenance treatment program. Journal of Addictive Disease. 2007;26:61–70. doi: 10.1300/J069v26n01_08. [DOI] [PubMed] [Google Scholar]
- Marsch LA. Technology-based interventions targeting substance use disorders and related issues: an editorial. Substance Use & Misuse. 2011;46:1–3. doi: 10.3109/10826084.2011.521037. [DOI] [PubMed] [Google Scholar]
- Moore BA, Barry DT, Sullivan LE, O’Connor PG, Cutter CJ, Schottenfeld RS, Fiellin DA. Counseling and directly observed medication for primary care buprenorphine/naloxone maintenance: A pilot study. Journal of Addiction Medicine. 2012;6:205–211. doi: 10.1097/ADM.0b013e3182596492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore BA, Fazzino T, Garnet B, Cutter CJ, Barry DT. Computer-based interventions for drug use disorders: A systematic review. Journal of Substance Abuse Treatment. 2011;40:215–223. doi: 10.1016/j.jsat.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosavel M. The use of a telephone-based communication tool by low-income substance abusers. J Health Commun. 2005;10:451–463. doi: 10.1080/10810730591009925. [DOI] [PubMed] [Google Scholar]
- Mundt JC, Bohn MJ, King M, Hartley MT. Automating standard alcohol use assessment instruments via interactive voice response technology. Alcoholism: Clinical & Experimental Research. 2002;26:207–211. [PubMed] [Google Scholar]
- Mundt JC, Perrine MW, Searles JS, Walter D. An application of interactive voice response (IVR) technology to longitudinal studies of daily behavior. Behavior Research Methods, Instruments & Computers. 1995;27:351–357. [Google Scholar]
- Myung SK, McDonnell DD, Kazinets G, Seo HG, Moskowitz JM. Effects of Web- and computer-based smoking cessation programs: meta-analysis of randomized controlled trials. Archives of Internal Medicine. 2009;169:929–937. doi: 10.1001/archinternmed.2009.109. [DOI] [PubMed] [Google Scholar]
- Naylor MR, Helzer JE, Naud S, Keefe FJ. Automated telephone as an adjunct for the treatment of chronic pain: A pilot study. Journal of Pain. 2002;3:429–438. doi: 10.1054/jpai.2002.129563. [DOI] [PubMed] [Google Scholar]
- Naylor MR, Helzer JE, Rathmell JP. Therapeutic Interactive Voice Response for chronic pain reduction and relapse prevention. Pain. 2008;134:335–345. doi: 10.1016/j.pain.2007.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naylor MR, Naud S, Keefe FJ, Helzer JE. Therapeutic Interactive Voice Response (TIVR) to reduce analgesic medication use for chronic pain management. Journal of Pain. 2010;11:1410–1419. doi: 10.1016/j.jpain.2010.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osgood-Hynes DJ, Greist JH, Marks IM, Baer L, Heneman SW, Wenzel KW, Vitse HM. Self-administered psychotherapy for depression using a telephone-accessed computer system plus booklets: An open U.S.-U.K. study. Journal of Clinical Psychiatry. 1998;59:358–365. doi: 10.4088/jcp.v59n0704. [DOI] [PubMed] [Google Scholar]
- Portnoy DB, Scott-Sheldon LAJ, Johnson BT, Carey MP. Computer-delivered interventions for health promotion and behavioral risk reduction: a meta-analysis of 75 randomized controlled trials, 1988–2007. Preventive Medicine. 2008;47:3–16. doi: 10.1016/j.ypmed.2008.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rooke S, Thorsteinsson E, Karpin A, Copeland J, Allsop D. Computer-delivered interventions for alcohol and tobacco use: a meta-analysis. Addiction. 2010;105:1381–1390. doi: 10.1111/j.1360-0443.2010.02975.x. [DOI] [PubMed] [Google Scholar]
- Rose GL, MacLean CD, Skelly J, Badger GJ, Ferraro TA, Helzer JE. Interactive voice response technology can deliver alcohol screening and brief intervention in primary care. Journal of General Internal Medicine. 2010;25:340–344. doi: 10.1007/s11606-009-1233-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose GL, Skelly JM, Badger G, MacLean CD, Malgeri MP, Helzer JE. Automated screening for at-risk drinking in a primary care office using Interactive Voice Response. Journal of Studies on Alcohol and Drugs. 2010;71:734–738. doi: 10.15288/jsad.2010.71.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose GL, Skelly JM, Badger GJ, Naylor MR, Helzer JE. Interactive voice response for relapse prevention following cognitive-behavioral therapy for alcohol use disorders: a pilot study. Psychological Services. 2012;9:174–184. doi: 10.1037/a0027606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Searles JS, Perrine MW, Mundt JC, Helzer JE. Self-report of drinking by touch-tone telephone: Extending the limits of reliable daily contact. Journal of Studies on Alcohol. 1995;56:375–382. doi: 10.15288/jsa.1995.56.375. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Ecological momentary assessment (EMA) in studies of substance use. Psychological Assessment. 2009;21:486–497. doi: 10.1037/a0017074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson TL, Kivlahan DR, Bush KR, McFall ME. Telephone self-monitoring among alcohol use disorder patients in early recovery: a randomized study of feasibility and measurement reactivity. Drug & Alcohol Dependence. 2005;79:241–250. doi: 10.1016/j.drugalcdep.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Sobel LC, Sobel MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Allen JP, Litten RZ, editors. Measuring alcohol consumption: psychosocial and biochemical methods. Totowa, NJ: Human Press; 1992. pp. 41–72. [Google Scholar]
- Substance Abuse and Mental Health Services Administration Office of Applied Studies. The TEDS Report: Substance Abuse Treatment Admissions Involving Abuse of Pain Relievers: 1998 and 2008. Rockville, MD: 2010. [Google Scholar]
- Sullivan LE, Moore BA, O’Connor PG, Barry DT, Chawarski MC, Schottenfeld RS, Fiellin DA. The association between cocaine use and treatment outcomes in patients receiving office-based buprenorphine/naloxone for the treatment of opioid dependence. American Journal on Addictions. 2010;19:53–58. doi: 10.1111/j.1521-0391.2009.00003.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson A, Darke S, Ross J, Teesson M. The effect of persistence of cocaine use on 12-month outcomes for the treatment of heroin dependence. Drug and Alcohol Dependence. 2006;81:293–300. doi: 10.1016/j.drugalcdep.2005.08.010. [DOI] [PubMed] [Google Scholar]