Abstract
Previous investigations have identified individuals who meet criteria for DSM-IV-TR substance dependence as applied to caffeine, but there is little research on treatments for caffeine dependence. This study aimed to thoroughly characterize individuals who are seeking treatment for problematic caffeine use. Ninety-four individuals who identified as being psychologically or physically dependent on caffeine, or who had tried unsuccessfully to modify caffeine consumption participated in a face-to-face diagnostic clinical interview. They also completed measures concerning caffeine use and quitting history, reasons for seeking treatment, and standardized self-report measures of psychological functioning. Caffeine treatment seekers (mean age 41 yrs, 55% women) consumed an average of 548 mg caffeine per day. The primary source of caffeine was coffee for 50% of the sample and soft drinks for 37%. Eighty-eight percent reported prior serious attempts to modify caffeine use (mean 2.7 prior attempts) and 43% reported being advised by a medical professional to reduce or eliminate caffeine. Ninety-three percent met criteria for caffeine dependence when generic DSM-IV-TR substance dependence criteria were applied to caffeine use. The most commonly endorsed criteria were withdrawal (96%), persistent desire or unsuccessful efforts to control use (89%), and use despite knowledge of physical or psychological problems caused by caffeine (87%). The most common reasons for wanting to modify caffeine use were health-related (59%) and not wanting to be dependent on caffeine (35%). This investigation reveals that there are individuals with problematic caffeine use who are seeking treatment, and suggests that there is a need for effective caffeine dependence treatments.
Keywords: Caffeine Dependence, DSM, Caffeine Withdrawal, Diagnosis, Treatment
Characterization of Individuals Seeking Treatment for Caffeine Dependence
Caffeine is the most widely used behaviorally active drug in the world. In the United States more than 85% of adults and children regularly consume caffeine (Frary, Johnson, & Wang, 2005). Mean daily caffeine consumption among adult caffeine consumers in the United States has been estimated to be 280 mg/day, the equivalent of about 2 cups of coffee, or 7 twelve oz cans of caffeinated soft drinks (Barone & Roberts, 1996). Caffeine is generally considered to be safe when consumed at normal dietary doses; however, it is not completely innocuous. Heavy caffeine use (> 400 mg per day) is associated with increased risk for health problems and pregnancy complications (Nawrot et al., 2003). Caffeine can increase symptoms of anxiety and insomnia. Moreover, caffeine has reinforcing effects and produces physical dependence such that acute abstinence results in withdrawal symptoms that at times can be severe (Juliano & Griffiths, 2004). Importantly, many regular caffeine users report an inability to quit or reduce caffeine use despite wanting to do so (Hughes, Oliveto, Liguori, Carpenter, & Howard, 1998).
The Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) does not recognize a diagnosis of substance dependence on caffeine (American Psychiatric Association, 2000); while the ICD-10 does (World Health Organization, 1992a, 1992b). The rationale for the exclusion from the DSM-IV was that additional clinical data were needed that demonstrate that caffeine users have difficulty stopping use, difficulty switching to decaffeinated products, and continue to use caffeine despite having knowledge of that caffeine aggravates their health (Hughes, 1994). Since that time, one population study and four clinical studies have identified individuals who meet the DSM-IV-TR criteria for substance dependence when applied to caffeine use (Hughes et al., 1998; Jones & Lejuez, 2005; Oberstar, Bernstein, & Thuras, 2002; Strain, Mumford, Silverman, & Griffiths, 1994; Svikis, Berger, Haug, & Griffiths, 2005). These studies reveal that caffeine use can be problematic for some individuals and that professional assistance may be warranted. To date, there exist only a handful of empirical studies and case reports on individuals receiving treatment for problematic caffeine use (Bernard, Dennehy, & Keefauver, 1981; Bryant, Dowell, & Fairbrother, 2002; Foxx & Rubinoff, 1979; James et al., 1988; James, Stirling, & Hampton, 1985). No prior study has evaluated the demand for treatment for problematic caffeine use or the characteristics such treatment seekers.
The present study sought to identify and characterize individuals who were interested in treatment for problematic caffeine use. Participants were queried about their caffeine use and quitting history, reasons for seeking treatment, and treatment preferences and goals. Structured clinical interviews were conducted to assess mental health and drug use history, and DSM-IV-TR substance dependence criteria applied to caffeine.
Method
Participants
Participants were adult men and women who responded to advertisements offering assistance to quit or reduce caffeine consumption for people who feel that that they “are psychologically or physically dependent on caffeine” or “have tried unsuccessfully to quit using caffeinated products in the past”. There was no mention of monetary compensation in the ads. To be eligible for the face-to-face interview callers had to report using at least 100 mg caffeine per day and express an interest in receiving caffeine treatment. Callers were also informed that illicit drug users were not eligible and thus may have self-selected out of the study. A total of 275 individuals completed the phone screening and 94 individuals (55.3% women, 80% Caucasian, 75% employed) with a mean age of 41 years (range 18 to 65; SD=12.3) comprised the final study sample. (One individual with current alcohol dependence and one individual with a current psychotic disorder were excluded based on the face-to-face interview). All participants were high school graduates, 67% had earned a bachelor’s degree and more than 30% had a graduate degree. Tobacco use was reported by 6% of participants (range was 4-40 cigarettes per day). Alcohol use was reported by 54%, with 32% reporting at least weekly use of alcohol as follows: 1-3 drinks per week (n=24); 4-7 drinks per week (n=4), and >15 drinks per week (n=2).
Procedure and Measures
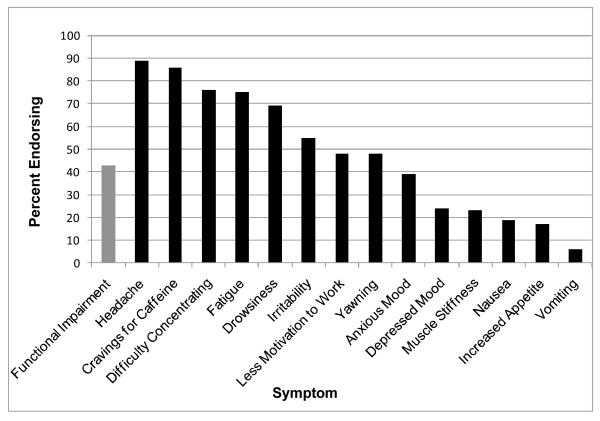
Upon arrival to the clinic participants provided informed consent and completed self-report measures and a structured clinical interview. Participants were compensated $20 for the 2-4 hr session. Specifically, participants completed a demographic and medical history questionnaire as well as the Caffeine Exposure Questionnaire (CEQ) (see Harrell & Juliano, 2009; Svikis et al., 2005), which instructed participants to indicate the number of servings and typical serving size of caffeinated products consumed in a typical day including coffee, tea, soft drinks, chocolate, foods, caffeine-containing medications/dietary supplements, and other1. Data were then entered into a spreadsheet that calculated total daily caffeine exposure based on standard caffeine concentrations and values obtained from manufacturers (Barone & Roberts, 1984, 1996; Juliano, Anderson, & Griffiths, 2011). Participants also completed a Caffeine History Questionnaire in which they documented caffeine-related advice received from health professionals, past attempts to quit or reduce caffeine use, and rated desire and confidence to quit caffeine use and to reduce caffeine use. They also indicated the latency to consume caffeine upon awakening. To characterize the emotional functioning of caffeine treatment seekers relative to normative data participants also completed the Beck Depression Inventory (BDI) (Beck & Steer, 1987), State Trait Anxiety Inventory (STAI) (Spielberger, 1983), and Profile of Mood States (POMS) (McNair, Lorr, & Droppleman, 1992). Following self-report assessments, the Structured Clinical Interview for DSM-IV Axis-I Disorders – Patient Edition (SCID-I/P) (First, Spitzer, & Williams, 1991) was administered by a Master’s or Doctoral level clinician. Caffeine dependence, caffeine withdrawal, and other features of caffeine use (e.g., age of first regular use) were also assessed via the Composite International Diagnostic Interview, Substance Abuse Module, Section E Version 4.1 (SAM-Section E) (Cottler, Robins, & Helzer, 1989). To assess withdrawal participants were asked if they had experienced any of 14 possible symptoms of caffeine withdrawal (see Figure 1) when abstaining from caffeine, or had used caffeine to avoid experiencing withdrawal, as well as if withdrawal had ever interfered with functioning.
FIGURE 1.
Endorsement of caffeine withdrawal symptoms by caffeine treatment seekers (N = 94). Black bars show the percentage of participants that endorsed the specified withdrawal symptom; gray bar shows the percentage of participants that indicated that withdrawal symptom(s) produced a significant functional behavioral impairment of daily activities.
Results
Phone screen data (N = 275)
Telephone screening was completed for 275 individuals (60% female; mean age = 40.0 yrs). In response to the question “Are you interested in receiving assistance to modify your caffeine use” 91% responded “yes”, with 51% reporting that they would like assistance to reduce caffeine use and 40% reporting that they would like assistance to quit using caffeine. Seven percent indicated that they might be interested in assistance and 2.3% said they were not interested. Among the 258 callers who responded, more than half were interested in face-to-face counseling (59.3%) with 47.3% interested in one-on-one counseling and 12% interested in group counseling. Nearly 25% were interested in a self-help booklet and 4.3% were interested in assistance via telephone. There were no differences between those not interviewed (n = 181) and the final interview sample (n = 94) in terms of age, gender, daily caffeine use, age of first regular caffeine use, desire to modify caffeine use or confidence, alcohol use, lifetime drug use, or history of drug, alcohol, or mental health treatment. However, those interviewed were significantly less likely to be smokers, 6% vs. 25%, X2 = 14.61(1, N =275) = p < .001, less likely to have been advised by a health professional to modify caffeine use, 43% vs. 58%, X2 (1, N = 274) = 6.17, p = .013, and had more years of formal education, X 2(7, N = 273) = 33.07, p < .001.
Daily Caffeine Consumption Patterns
Participants (N = 94) reported consuming a mean of 547.8 mg of caffeine per day (SD = 470.4; Median = 387.5, range = 120 mg to 2667 mg). Participants reported daily consumption of soft drinks (74%), roasted or ground coffee (56%), cocoa/chocolate (36%), bag or leaf tea (34%), instant tea (10%), instant coffee (7%), and caffeine-containing medications (6%). The primary source of caffeine (i.e., 50% greater than next largest caffeine source) was coffee for 50% of the sample, soft drinks for 37%, and tea for 5%. Most participants (81%) reported having their first caffeinated product within 60 min of waking, with 30% reporting caffeine use within 15 min of waking. The mean age of onset of regular caffeine consumption was 15.9 yrs (SD = 6.4).
History of Caffeine Reduction or Quit Attempts
Eighty-eight percent reported at least one past serious attempt to quit or reduce caffeine (M = 2.7, SD = 3.1). Sixty-two percent reported at least one past attempt to quit caffeine use, with 62% unable to maintain abstinence for 30 days or more. Fifty-four percent reported a past serious attempt to reduce caffeine use, with 70% unable to maintain the reduced amount for 30 days or more. Forty-three percent reported being advised by a health professional to modify caffeine use for reasons including cardiovascular problems, fibrocystic breast disease, pregnancy, anxiety, headaches, urinary problems, gastric problems, hypoglycemia, and sleep difficulties. Some participants reported that a doctor had advised caffeine reduction as a means to reduce caloric intake from caffeinated sugary soft drinks. Only 20% of those advised to modify caffeine use reported having been given advice on how to do so. Mean desire to modify caffeine use on a 0 to 10 scale was 7.79 (SD = 2.18), while the mean rating for confidence in achieving one’s ideal caffeine use goal was 4.16 (SD = 3.05). Sixty percent of participants reported a goal of caffeine reduction, while 40% reported a goal of complete abstinence. As shown in Table 1, health concerns were the most common reason for wanting to modify caffeine use (59%) followed by not wanting to be dependent on caffeine (35%).
Table 1.
Participants (N= 94) Were Asked the Open Ended Question: “What Are Your Reasons for Wanting to Modify your Caffeine Use at This Time?” The Most Commonly Reported Responses Are Categorized Below
| Percentage | |
|---|---|
| Any health problems/concerns | 58.9% |
| General health problems/concerns | 46.2% |
| Cardiovascular problems/concerns | 6.4% |
| Gastrointestinal problems/concerns | 5.1% |
| Frequent urination/bladder problems | 3.8% |
| Dental health | 3.8% |
| Other specific health problem/concerns | 2.6% |
| Do not want to be addicted/dependent/ | 34.6% |
| controlled by caffeine | |
| Weight concerns | 17.9% |
| Improve insomnia or sleep difficulties | 16.7% |
| Improve psychological functioning/ | |
| functioning | 11.5% |
| Reduce anxiety/jitteriness | 10.3% |
| Avoid withdrawal cycle | 9.0% |
| (e.g., headache) | |
| Monetary cost | 9.0% |
| Reduce (non-sleep/non-anxiety related) | |
| negative physical effects (e.g., nausea) | 7.7% |
| For children/better role model for children | 5.1% |
| Advice of health professional | 3.8% |
| Plans to get pregnant | 2.6% |
Caffeine Withdrawal
When queried about 14 possible caffeine withdrawal symptoms, 96% of participants reported two or more caffeine withdrawal symptoms when abstaining from caffeine, with a mean of 6.8 symptoms (SD 2.82). The rates of endorsement of specific withdrawal symptoms are shown in Figure 1, with headache being the most frequently endorsed (89%). Forty-three percent reported functional impairment due to withdrawal and provided examples such as being unable to work, sleeping at work, missing activities on vacation, and being unable to attend church.
Caffeine Dependence
Table 2 presents the rates of endorsement (past year) of the seven DSM-IV-TR dependence criteria as applied to caffeine use. Ninety-three percent of participants fulfilled DSM-IV-TR criteria for substance dependence as applied to caffeine by endorsing at least three of the seven diagnostic criteria, with 55% of participants endorsing at least five of seven criteria. When only four of the DSM-IV-TR criteria that seem most applicable to caffeine were considered (i.e., withdrawal; persistent desire or unsuccessful efforts to cut down or control use; continued use despite knowledge of a persistent or recurrent physical or psychological problem; and tolerance, Strain et al., 1994), 89% of participants met criteria. As an even more conservative approach, when tolerance was omitted 79% met criteria (i.e., endorsed all three remaining criteria).
Table 2.
Rates of Endorsement of Criteria for DSM-IV-TR Substance Dependence Applied to Caffeine for the Present Study Sample
| SUBSTANCE DEPENDENCE CRITERIA --PAST YEAR |
|
|---|---|
| 1. Tolerance | 70% (61-79) |
| Need for increased amounts to achieve desired effects |
65% (55-75) |
| Diminished effect with continued use of same amount |
53% (43-63) |
| 2. Withdrawal | 96% (92-100) |
| The characteristic withdrawal syndrome |
94% (89-99) |
| Substance is taken to avoid withdrawal symptoms |
92% (87-97) |
|
3. Substance is often taken in larger
amounts or for longer time than intended |
38% (28-48) |
|
4. Persistent desire or unsuccessful effort to
cut down or control substance use |
89% (83-96) |
| Strong desire to stop | 45% (34-55) |
| Strong desire to cut down | 82% (74-90) |
| Strong desire to control | 89% (83-95) |
| Tried to stop | 65% (55-75) |
| Tried to cut down | 80% (72-88) |
| Tried to control | 80% (72-88) |
|
5. Great deal of time is spent in activities
necessary to obtain, use, or recover from the effects of the substance |
61% (51-71) |
| A lot of time obtaining | 36% (26-46) |
| A lot of time using | 56% (46-66) |
| A lot of time recovering from the effects |
14% (7-21) |
|
6. Important social, occupational, or
recreational activities are given up or reduced because of use |
8% (3-13) |
|
7. Continued use despite knowledge of
physical or psychological problems caused or exacerbated by caffeine |
87% (80-94) |
| Physical problems | 83% (75-91) |
| Sleep difficulties | 50% (40-60) |
| Frequent urination | 48% (38-58) |
| Stomach problems | 36% (26-46) |
| Fast or irregular heartbeat/chest pain | 29% (20-38) |
| Psychological problems | 67% (57-76) |
| Anxious, jittery, or nervous | 45% (35-55) |
| Irritated or angry | 39% (29-49) |
| Paranoia | 5% (1-9) |
Data in columns show the prevalence of endorsement of criteria or symptom; 95% confidence intervals are shown in parentheses; absence of a percentage and/or confidence interval indicates that it was not measured or reported in the study.
Psychiatric History and Self-Reported Mood Data
Anxiety and mood disorders were the most prevalent current diagnoses (17% each) and lifetime diagnoses (26% and 42% respectively). Twelve percent of the sample had a past history of alcohol dependence, while few had lifetime history of dependence on an illicit drug. The prevalence rates of these and other diagnoses are presented in Table 3. The mean STAI-state score for the sample was 35.1 (SD = 11.4), which is similar to adult normative data (Spielberger, 1983). The mean STAI-trait score was slightly elevated in the sample (M = 40.3; SD = 10.4), compared to adult normative data (M = 34.9: SD = 9.2) (Spielberger, 1983). The POMS Total Mood Disturbance score (Mean = 23.5, SD = 32.5) and individual factor scores were similar to scores obtained from adult normative samples (McNair et al., 1992). Nine percent of the sample scored greater than15 on the BDI (an indicator of depression, Beck & Steer, 1987).
Table 3.
DSM-IV-TR Current and Lifetime Disorder Prevalence for Caffeine Treatment Seekers (N = 94)
| Current | Lifetime | |
|---|---|---|
| Mood Disorder | 17% | 42% |
| Major Depressive Disorder | 9% | 35% |
| Bipolar Disorder | 4% | 5% |
| Dysthymic Disorder | 4% | 4% |
| Anxiety Disorder | 17% | 26% |
| Generalized Anxiety Disorder | 9% | 9% |
| Specific Phobia | 5% | 7% |
| Obsessive-Compulsive Disorder | 3% | 4% |
| Panic Disorder | 3% | 6% |
| Posttraumatic Stress Disorder | 2% | 4% |
| Agoraphobia w/o Panic | 1% | 1% |
| Social Phobia | 0% | 1% |
| Eating Disorder | 2% | 5% |
| Bulimia Nervosa | 2% | 3% |
| Anorexia Nervosa | 0% | 1% |
| Eating Disorder NOS | 0% | 1% |
| Substance-Related Disorder | 7% | 33% |
| Nicotine Dependence | 6% | 24% |
| Alcohol Abuse | 1% | 4% |
| Alcohol Dependence | - | 13% |
| Cocaine Dependence | - | 3% |
| Cocaine Abuse | - | 1% |
| Marijuana Abuse | - | 2% |
Associations between Caffeine Dependence, Caffeine Use, and Other Variables of Interest
Additional analyses were conducted to explore possible correlates of caffeine dependence (defined as meeting 3 of 3 of the most applicable criteria), and caffeine consumption. Caffeine consumption (log transformed for normality) did not differ among those who did (n = 74) and did not (n = 20) fulfill a caffeine dependence diagnosis [raw score mean = 549 mg vs. 544 mg, t (1, 92) = -.041, p = .967]. There were also no differences in the likelihood of caffeine dependence based on primary source of caffeine (coffee vs. soft drinks) or gender. Pearson correlations revealed that greater caffeine consumption was associated with older age, r = .285, p = .005, shorter latency to consume caffeine upon awakening, r = -.265, p = .019, and lower desire to quit caffeine use, r = -.370, p < .001. Caffeine consumption was not associated with desire to reduce caffeine use, confidence in achieving one’s caffeine use goal, alcohol use, gender, or any of the affect-related measures.
Discussion
This study identified individuals who were seeking assistance to modify their caffeine use and determined the characteristics and motivations of such individuals. Not surprisingly our sample on average had high levels of consumption -- nearly double the caffeine intake (548 mg) of the typical adult caffeine consumer in the U.S. (280 mg; Barone & Roberts, 1996). However, daily caffeine exposure varied widely (120 mg – 2667 mg), with a range similar to that reported in a prior study that assessed for problematic caffeine use (Strain et al., 1994). A diagnosis of caffeine dependence was not necessarily indicative of high daily exposure to caffeine as approximately 25% of those meeting dependence criteria consumed less than the U.S. population mean of 280 mg. This is not too surprising as experimental research has shown that daily consumption of as little as 100 mg caffeine per day is sufficient to produce physical dependence (Griffiths et al., 1990). Soft drinks were the primary source of caffeine for a substantial portion of the sample (37%), which indicates that problematic caffeine use is not limited to coffee.
Nearly 90% of those interviewed reported that they had tried unsuccessfully in the past to reduce or eliminate caffeine, with an average of 2.7 previous attempts. This is consistent with data showing that individuals seeking assistance for other drug dependencies typically have a history of failed quit attempts (Shiffman, Brockwell, Pillitteri, & Gitchell, 2008). It also provides evidence that not all caffeine users can simply quit using caffeine on their own, an attitude that is likely held by some health professionals, as has been in the past for drugs such as nicotine and marijuana (Budney, Radonovich, Higgins, & Wong, 1998).
Forty percent of the sample indicated a goal of complete caffeine cessation, whereas 60% indicated a goal of caffeine reduction. Greater caffeine consumption was associated with less desire for complete cessation. Caffeine is a unique drug of dependence in that it is difficult to completely avoid, and moderate use is not associated with harm in most cases. Thus, caffeine reduction appears on the surface to be a reasonable goal. However, in the present study, participants reported prior unsuccessful attempts at both caffeine cessation and reduction. Future research is necessary to determine the likelihood of achieving success with caffeine reduction and/or cessation. On average participants reported a strong desire to modify caffeine use but had relatively low confidence that they could achieve their ideal caffeine use goals. This is concerning because confidence that one can change behavior, or self-efficacy, is an important predictor of health behavior change (Shiffman et al., 2000; Strecher, Becker, & Rosenstock, 1986). The relatively low confidence ratings in the current study further suggest that individuals who identify as having problematic caffeine use may require professional assistance.
Forty-three percent of participants reported having been advised by a health professional to modify caffeine use for health (e.g., cardiovascular) or psychological (e.g., anxiety) problems, with only 20% reporting that they received any specific advice on how to do so. Patients may benefit from treatment assistance when advised by health professionals to curtail caffeine use. There are very few studies assessing physicians’ knowledge and practices pertaining to caffeine (Hughes, Amori, & Hatsukami, 1988; Anderson, Juliano, & Schulkin, 2009).
The most common reason offered by participants for wanting to quit or reduce caffeine consumption were general or specific health concerns (58.9%) which is consistent with a prior population based study (Hughes & Oliveto, 1997). Interestingly, some participants reported that they viewed caffeine modification as a means to lose weight because their caffeinated beverages of choice were sugary soft drinks. There is evidence that caffeine in soft drinks maintains caffeine self-administration (Liguori & Hughes, 1997) and that soft drink consumption is associated with obesity and other negative health outcomes (Vartanian, Schwartz, & Brownell, 2007). Thus, it could be speculated that overcoming one’s dependency on caffeine could have secondary beneficial effects on health and weight due to reduced exposure to caloric sugary soft drinks. This hypothesis should be evaluated in future studies.
DSM-IV-TR Caffeine Dependence Criteria
Ninety-three percent of the sample fulfilled DSM-IV-TR criteria for substance dependence applied to their caffeine use. We also evaluated the rate of caffeine dependence using only the four DSM criteria that seem most meaningful to the assessment of problematic caffeine use (use despite harm, withdrawal, persistent desire or unsuccessful efforts to control use, and tolerance) and found that 89% of participants fulfilled criteria. This high rate observed among caffeine treatment seekers contrasts with 9% fulfilling at least 3 of these 4 criteria in a non-treatment seeking population based study (Hughes et al., 1998).
The most commonly endorsed criterion was caffeine withdrawal (96%). Prior experimental research has demonstrated that habitual caffeine use is largely maintained by the avoidance of withdrawal symptoms (Juliano & Griffiths, 2004). The most common withdrawal symptom reported in the current investigation was headache (89%) and 43% reported that caffeine withdrawal caused significant functional impairment (e.g., unable to work). Future research is needed to evaluate the role of caffeine withdrawal in an individual’s perception that his or her caffeine use is problematic as well as in the outcomes of caffeine quit attempts. The caffeine withdrawal syndrome is a research diagnosis in the DSM-IV-TR. The present findings add to the empirical database supporting caffeine withdrawal as a valid and clinically important diagnosis.
Eighty-nine percent of participants met the criterion of a persistent desire or unsuccessful efforts to cut down or control use. This is not surprising given that this sample was actively seeking treatment and most had made previous unsuccessful attempts to reduce or quit using caffeine in the past. However, it is notable that this criterion was the most commonly endorsed (56%) in a (non-treatment seeking) population based study of DSM substance dependence criteria as applied to caffeine (Hughes et al., 1998). A total of 87% of the present sample endorsed continued use of caffeine despite knowledge of persistent or recurrent physical or psychological problems that they believe to be caused or exacerbated by caffeine. These data suggest that, like other recreational drugs, caffeine use can be difficult to stop even when there is awareness that caffeine is causing harm.
We also compared individuals who did and did not fulfill all three of the caffeine dependence criteria most applicable to caffeine, but we did not identify any differences in level of caffeine consumption, primary source of caffeine, or gender. Future studies, ideally with larger sample sizes, should evaluate the statistical and conceptual relevance of the individual substance dependence criteria to the caffeine dependence syndrome, as well as identify meaningful correlates of a caffeine dependence diagnosis.
Limitations and Future Research Directions
The sample was comprised mostly of individuals from the greater Baltimore-Washington D.C. metropolitan area. Large scale epidemiological studies are needed to determine the prevalence of caffeine dependence and the demand for caffeine treatment in the general population. Our interview sample consisted only of individuals who were interested in face-to-face counseling for problematic caffeine use, which excluded 40% of callers who expressed interest in other forms of assistance (e.g., self-help booklet). Future research should address this gap. Our final sample did not include individuals who used illicit drugs, were alcohol dependent, or psychotic. It should be noted, however, that there did not appear to be high demand for caffeine treatment among such individuals. Although not formally excluded, callers who were smokers, less formally educated, and more likely to have been advised by a medical professional to modify caffeine use were less likely to attend the in person interview. Thus, our interview sample may not reveal the full range of characteristics of individuals who are caffeine dependent and/or who may benefit from assistance. Regular use of energy drinks was low among our sample, which could be a function of lower energy drink consumption in prior years, the older age of participants, or the fact that we did not explicitly ask about energy drinks. Energy drinks continue to grow in popularity and it is possible that a greater number of individuals will experience problematic energy drink use and may seek treatment in the future. The intentional combined use of caffeine and alcohol also appears to be increasing and may be associated with increased harm (O’Brien, Arria, Howland, James, & Marczinski, 2011; Reissig, Strain, & Griffiths, 2009). The need for treatments for the combined use of caffeine and alcohol is a potentially important area of inquiry.
Summary
A sample of individuals who were actively seeking treatment for problematic caffeine use and who were interested in participating in a formal structured treatment program were identified. These individuals were highly educated, had a wide range of caffeine consumption, were primarily coffee and soft drink consumers, and had high rates of clinical dependence on caffeine using generic DSM substance dependence criteria. Moreover, our sample did not have high rates of co-morbid psychopathology and were seeking psychological treatment specific to problematic caffeine use. These findings suggest that caffeine dependence should be recognized as a clinical syndrome and that effective treatments for problematic caffeine use should be developed.
Acknowledgments
The authors would like to thank Mary Cosimano, Jenna Cohen, Kristen McCausland, and Kimberly Mudd for their assistance with participant recruitment, data collection, and data management. This research was funded by a grant from the National Institute on Drug Abuse (R01 DA03890).
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the finalcopyediting, fact-checking, and proofreading required for formal publication. It is not thedefinitive, publisher-authenticated version. The American Psychological Association and itsCouncil of Editors disclaim any responsibility or liabilities for errors or omissions of thismanuscript version, any version derived from this manuscript by NIH, or other third parties. Thepublished version is available at www.apa.org/pubs/journals/ADB
A more recent version of this measure includes energy drinks as an explicit category.
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. American Psychiatric Press; Washington D.C.: 2000. Text Revision. [Google Scholar]
- Anderson BL, Juliano LM, Schulkin J. Caffeine’s implications for women’s health and survey of obstetrician-gynecologists’ caffeine knowledge and assessment practices. Journal of Womens Health (Larchmt) 2009;18:1457–1466. doi: 10.1089/jwh.2008.1186. doi: 10.1089=jwh.2008.1186. [DOI] [PubMed] [Google Scholar]
- Barone JJ, Roberts HR. Caffeine consumption. Food and Chemical Toxicology. 1996;34:119–129. doi: 10.1016/0278-6915(95)00093-3. doi:10.1016/0278-6915(95)00093-3. [DOI] [PubMed] [Google Scholar]
- Beck A, Steer R. Beck Depression Inventory Manual. Psychological Corp; New York: 1987. [Google Scholar]
- Bernard ME, Dennehy S, Keefauver LW. Behavioral treatment of excessive coffee and tea drinking: A case study and partial replication. Behavior Therapy. 1981;12:543–548. doi:10.1016/S0005-7894(81)80092-5. [Google Scholar]
- Bryant CM, Dowell CJ, Fairbrother G. Caffeine reduction education to improve urinary symptoms. British Journal of Nursing. 2002;11:560–565. doi: 10.12968/bjon.2002.11.8.10165. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Radonovich KJ, Higgins ST, Wong CJ. Adults seeking treatment for marijuana dependence: a comparison with cocaine-dependent treatment seekers. Experimental and Clinical Psychopharmacology. 1998;6:419–426. doi: 10.1037//1064-1297.6.4.419. doi: 10.1037/1064-1297.6.4.419. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Robins LN, Helzer JE. The reliability of the CIDI-SAM: a comprehensive substance abuse interview. British Journal of Addiction. 1989;84:801–814. doi: 10.1111/j.1360-0443.1989.tb03060.x. doi:10.1111/j.1360-0443.1989.tb03060.x. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Williams J. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. New York State Psychiatric Institute; New York: 1991. [Google Scholar]
- Foxx RM, Rubinoff A. Behavioral treatment of caffeinism: reducing excessive coffee drinking. Journal of Applied Behavioral Analysis. 1979;12:335–344. doi: 10.1901/jaba.1979.12-335. doi: 10.1901/jaba.1979.12-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frary CD, Johnson RK, Wang MQ. Food sources and intakes of caffeine in the diets of persons in the United States. Journal of the American Dietetic Association. 2005;105:110–113. doi: 10.1016/j.jada.2004.10.027. doi:10.1016/j.jada.2004.10.027. [DOI] [PubMed] [Google Scholar]
- Griffiths RR, Evans SM, Heishman SJ, Preston KL, Sannerud CA, Wolf B, Woodson PP. Low-dose caffeine physical dependence in humans. Journal of Pharmacology and Experimental Therapeutics. 1990;255:1123–1132. [PubMed] [Google Scholar]
- Harrell PT, Juliano LM. Caffeine expectancies influence the subjective and behavioral effects of caffeine. Psychopharmacology (Berl) 2009;207:335–342. doi: 10.1007/s00213-009-1658-5. doi: 10.1007/s00213-009-1658-5. [DOI] [PubMed] [Google Scholar]
- Hughes JR. Caffeine withdrawal, dependence, and abuse. In: Widiger TA, Frances AJ, Pincus HA, First MB, Ross R, Davis W, editors. DSM-IV Sourcebook. American Psychiatric Association; Washington, D.C.: 1994. pp. 129–134. [Google Scholar]
- Hughes JR, Amori G, Hatsukami DK. A survey of physician advice about caffeine. Journal of Substance Abuse. 1988;1:67–70. doi: 10.1016/s0899-3289(88)80009-9. doi:10.1016/S0899-3289(88)80009-9. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Oliveto AH. A systematic survey of caffeine intake in Vermont. Experimental and Clinical Psychopharmacology. 1997;5:393–398. doi: 10.1037//1064-1297.5.4.393. doi: 10.1037/1064-1297.5.4.393. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Oliveto AH, Liguori A, Carpenter J, Howard T. Endorsement of DSM-IV dependence criteria among caffeine users. Drug and Alcohol Dependence. 1998;52:99–107. doi: 10.1016/s0376-8716(98)00083-0. doi:10.1016/S0376-8716(98)00083-0. [DOI] [PubMed] [Google Scholar]
- James JE, Paull I, Cameron-Traub E, Miners JO, Lelo A, Birkett DJ. Biochemical validation of self-reported caffeine consumption during caffeine fading. Journal of Behavioral Medicine. 1988;11:15–30. doi: 10.1007/BF00846166. doi: 10.1007/BF00846166. [DOI] [PubMed] [Google Scholar]
- James JE, Stirling KP, Hampton BA. Caffeine fading: Behavioral treatment of caffeine abuse. Behavior Therapy. 1985;16:15–27. doi:10.1016/S0005-7894(85)80052-6|. [Google Scholar]
- Jones HA, Lejuez CW. Personality correlates of caffeine dependence: the role of sensation seeking, impulsivity, and risk taking. Experimental and Clinical Psychopharmacology. 2005;13:259–266. doi: 10.1037/1064-1297.13.3.259. doi: 10.1037/1064-1297.13.3.259. [DOI] [PubMed] [Google Scholar]
- Juliano LM, Anderson BA, Griffiths RR. Caffeine. In: Lowinson JH, Ruiz P, Millman RB, Langrod JG, editors. Substance Abuse: A Comprehensive Textbook. Fifth Edition Lippincott, Williams, & Wilkins; Baltimore: 2011. pp. 335–353. [Google Scholar]
- Juliano LM, Griffiths RR. A critical review of caffeine withdrawal: empirical validation of symptoms and signs, incidence, severity, and associated features. Psychopharmacology (Berl) 2004;176:1–29. doi: 10.1007/s00213-004-2000-x. doi: 10.1007/s00213-004-2000-x. [DOI] [PubMed] [Google Scholar]
- Liguori A, Hughes JR. Caffeine self-administration in humans: 2. A within-subjects comparison of coffee and cola vehicles. Experimental and Clinical Psychopharmacology. 1997;5:295–303. doi: 10.1037//1064-1297.5.3.295. doi: 10.1037/1064-1297.5.3.295. [DOI] [PubMed] [Google Scholar]
- McNair D, Lorr M, Droppleman L. Edits Manual for the Profile of Mood States. Educational and Industrial Testing Service; San Diego: 1992. [Google Scholar]
- Nawrot P, Jordan S, Eastwood J, Rotstein J, Hugenholtz A, Feeley M. Effects of caffeine on human health. Food Additives & Contaminants. 2003;20:1–30. doi: 10.1080/0265203021000007840. [DOI] [PubMed] [Google Scholar]
- Oberstar JV, Bernstein GA, Thuras PD. Caffeine use and dependence in adolescents: one-year follow-up. Journal of Child and Adolescent Psychopharmacology. 2002;12:127–135. doi: 10.1089/104454602760219162. doi:10.1089/104454602760219162. [DOI] [PubMed] [Google Scholar]
- O’Brien MC, Arria M, Howland J, James JE, Marczinski CA. Caffeine, alcohol, & youth: A toxic mix. Journal of Caffeine Research. 2011;1:15–21. doi: 10.1089/jcr.2011.1202. doi:10.1089/jcr.2011.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reissig CJ, Strain EC, Griffiths RR. Caffeinated energy drinks--a growing problem. Drug and Alcohol Dependence. 2009;99:1–10. doi: 10.1016/j.drugalcdep.2008.08.001. doi:10.1016/j.drugalcdep.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Balabanis MH, Paty JA, Engberg J, Gwaltney CJ, Liu KS, Paton SM. Dynamic effects of self-efficacy on smoking lapse and relapse. Health Psychology. 2000;19:315–323. doi: 10.1037//0278-6133.19.4.315. doi: 10.1037/0278-6133.19.4.315. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG. Individual differences in adoption of treatment for smoking cessation: demographic and smoking history characteristics. Drug and Alcohol Dependence. 2008;93:121–131. doi: 10.1016/j.drugalcdep.2007.09.005. doi:10.1016/j.drugalcdep.2007.09.005. [DOI] [PubMed] [Google Scholar]
- Spielberger C. Manual for the State-Trait Anxiety Inventory: STAI (Form Y) Consulting Psychologists Press; Palo Alto, CA: 1983. [Google Scholar]
- Strain EC, Mumford GK, Silverman K, Griffiths RR. Caffeine dependence syndrome. Evidence from case histories and experimental evaluations. JAMA. 1994;272:1043–1048. doi: 10.1001/jama.1994.03520130081037. [PubMed] [Google Scholar]
- Strecher V, B. D, Becker M, Rosenstock I. The role of self-efficacy in achieving health behavior change. Health Education Quarterly. 1986;13:73–91. doi: 10.1177/109019818601300108. doi: 10.1177/109019818601300108. [DOI] [PubMed] [Google Scholar]
- Svikis DS, Berger N, Haug NA, Griffiths RR. Caffeine dependence in combination with a family history of alcoholism as a predictor of continued use of caffeine during pregnancy. American Journal of Psychiatry. 2005;162:2344–2351. doi: 10.1176/appi.ajp.162.12.2344. doi: 10.1176/appi.ajp.162.12.2344. [DOI] [PubMed] [Google Scholar]
- Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. American Journal of Public Health. 2007;97:667–675. doi: 10.2105/AJPH.2005.083782. doi: 10.2105/AJPH.2005.083782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. World Health Organization; Geneva, Switzerland: 1992a. [Google Scholar]
- World Health Organization . International Statistical Classification of Diseases and Related Health Problems, 10th Revision. Vol. 1. World Health Organization; Geneva, Switzerland: 1992b. [Google Scholar]