Abstract
Background & Aims
In patients with chronic liver disease, race plays a role in rate of liver transplantation and patient survival after transplantation. It is not known however how race and ethnicity influence the presentation, etiology and outcomes in patients with acute liver failure (ALF).
Methods
A retrospective cohort study was conducted utilizing the ALF Study Group database to assess differences between racial and ethnic groups in subjects with ALF.
Results
In the cohort of 927 subjects (81.8% white, 12.8% black and 5.4% Asian), enrolled between January 1998 and March 2006, age, gender and level of education were comparable among the groups. Differences were found in the prevalence of psychiatric illness and the use of medications. Racial groups also differed with respect to etiology of ALF. Whites presented more frequently with acetaminophen toxicity (51% vs. 27%, P <0.001). By day 21, 228 (30%) whites, 46 (39%) blacks, and 11 (22%) Asians had died. There were no statistically significant differences found in overall mortality after adjustment for potential confounders including etiology of ALF, degree of encephalopathy, age, gender, admission laboratory values and region. The odds of liver transplantation were higher among Asians and Hispanics however this finding was attenuated in Asians after adjustment for the above confounders (adjusted OR 1.50; 95% CI 0.72-3.13 and 1.89; 95% CI 1.08 – 3.30, respectively).
Conclusion
In patients with ALF, there were no significant differences in survival or rate of liver transplantation among racial and ethnic groups except for transplantation in Hispanics.
Introduction
In 1999, the United States Congress charged the Institute of Medicine with the task of identifying factors which are responsible for racial and ethnic disparities in healthcare and designing strategies to address these inequities.1 The results of this investigation highlighted differences for racial and ethnic minorities in access to, and delivery of care for cardiovascular, renal and general medical conditions.2 Prior data substantiates such disparities in the treatment for chronic liver disease and its sequelae.3 With respect to liver transplantation, the only curative therapy for end stage liver disease, blacks are sicker at the time of listing, more likely to die once listed and less likely to be transplanted than whites.4 Further, several studies have demonstrated that blacks and Asians have worse graft survival after transplantation as well as poorer 2-year and 5-year overall survival.5, 6 However, these data focus on outcomes in chronic liver dysfunction and failure. In acute liver failure (ALF), the role that disparities may play in clinical outcomes has not been well established.
ALF is a potentially fatal condition characterized by severe hepatic injury with resultant liver dysfunction and encephalopathy.7, 8 Although the case fatality rate in ALF has improved considerably from the 80% or greater quoted for the pre-liver transplantation period,9 an overall death rate of 30% still remains.10 Approximately half of patients recover with supportive care and the use of N-acetylcysteine if indicated; however, liver transplantation remains the last resort for < 50% of patients with ALF.
Given the scarcity of available organs for transplantation, it is important to define prognostic markers of poor outcomes and the need for transplantation. While clinical prognostic factors are well described,11 there are limited data on the effect of race and ethnicity on outcomes in ALF. One study reported that non-Caucasian ethnicity was associated with a four fold increase in mortality after transplantation for seronegative ALF.12 This finding, while limited by the size of the cohort studied and its focus on ALF patients undergoing transplantation, suggests that the same racial and ethnic differences noted in chronic liver disease may be present in ALF. Therefore, the goal of this study was to assess differences in presentation, etiologies, and outcomes between racial and ethnic groups in the setting of ALF.
Methods
Study Population and Data Source
We conducted a retrospective cohort study using the U.S. Acute Liver Failure Study Group (ALFSG) database.7, 13 The ALFSG, an initiative sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases, compiled data from 27 academic centers for subjects presenting for the management of ALF. To be considered for enrollment, subjects were required to have had ALF, as defined by: 1) a prothrombin time >15 seconds or International Normalized Ratio (INR) ≥1.5; 2) evidence of hepatic encephalopathy;14 3) illness of <26 weeks in duration; and 4) absence of a prior history of chronic liver disease.13 Once considered a potential study subject, informed consent was obtained from the appropriate guardian or health care proxy. All subjects enrolled in ALFSG over the age of 15 years between January 1, 1998 and March 30, 2006 were eligible for inclusion in the study.
Main Study Outcomes
The primary endpoints were death and liver transplantation which were determined for all subjects from medical record review by ALF study personnel at all study sites. Secondary outcomes included transplant-free survival and post liver transplantation survival for those transplanted during the study period.
Data Collection
At the time of study enrollment, the following clinical variables were collected for the ALFSG database: 1) demographics; 2) comorbidities; 3) admission laboratory data; 4) social history; and 5) etiology of ALF. Racial group was determined by study personnel and categorized according to the National Institutes of Health (NIH) classification scheme. Given the small sample size for the American Indian or Alaskan Native and Native Hawaiian and other Pacific Islander groups and the heterogeneous nature of these groups precluding their combination, these distinctions were omitted from the statistical analysis. Ethnicity was classified into two groups also according to the NIH classification: 1) non-Hispanic whites and 2) Hispanics or Latinos. Comorbidities collected at the time of study enrollment were established by the legal next of kin or prior medical history, if available. Etiologies of ALF were established on the basis of serologies, biopsy and/or post specimens. The final diagnosis identified in the database for each subject was the etiology utilized in this study.
Given the number of study sites who contributed information to the AFLSG, a regional variable was created. The regions were based on the US regional subdivisions as identified by the US census bureau.
Statistical analyses
Categorical variables were summarized by frequencies and proportions, and continuous variables were summarized by means and standard deviations. Categorical variables were compared with a χ2 test or Fisher’s exact test as appropriate. Continuous variables were compared using a Student’s t-test, Wilcoxon rank sum, ANOVA or Kruskal-Wallis based on the distribution of data and number of groups being compared.
For all patients, follow-up began on the date of hospital admission. Follow-up ended on the date of death or 21 days after study enrollment, the assessment time point defined by the ALF study protocol.7 For those individuals who died on the date of hospital admission, a time to event of 0.5 days was allotted for the analysis. In all analyses exploring an association between race and outcome, whites represented the reference group as this was the largest group in the cohort.
Kaplan-Meier15 survival analysis and Cox16 proportional hazards modeling were performed to determine the overall survival, survival without transplantation and post transplantation survival by race and ethnicity. Survival curves were compared with log rank statistics. Univariable associations with a level of significance ≤0.10 (P≤0.10) were included in the multivariable model. Potential confounders, specifically age, gender, degree of encephalopathy, and etiology of ALF were included in all multivariable models, without regard to level of statistical significance as they were deemed clinically significant. By convention, any variable missing more than 25% of entries was omitted from all multivariable analyses. Standard model checking procedures including visual inspection of diagnostic log-log plots and calculation of standard test statistics for the violation of the proportional hazards assumption were employed.
Logistic regression was utilized to compare the likelihood of liver transplantation in the groups. Univariable associations with a level of significance ≤0.10 (P≤0.10) were included in the multivariable model as well as the potential confounders listed above. Standard model checking procedures were employed.
For all analyses, an interaction between race and etiology of ALF was tested by including a multiplicative interaction term. This interaction term was not significant in any model and therefore was not included in the final adjusted models.
Statistical significance was declared for a hypothesis test for a P-value <0.05. Analyses were performed using STATA version 10 (StataCorp, College Station, TX). Sample size discussion removed secondary to space limitation.
Results
Race
Baseline Characteristics
The ALF cohort included 973 subjects of whom 927 were included for review. Of these, 758 (81.8%) were white, 119 (12.8%) were black or African American, and 50 (5.4%) were Asian. The racial groups were similar in gender, years of education, and age (Table 1). For comorbidities, the groups were different with respect to the presence of psychiatric illness, hypertension and former polysubstance abuse. Whites bore the burden of psychiatric illness in the cohort with 30.5% having an identifiable psychiatric diagnosis at the time of study enrollment (P <0.01). Twenty percent of blacks had hypertension, in comparison to 11.6% of whites and 8.0% of Asians (P=0.02). Prior polysubstance abuse was reported in 23.2% of whites, 18.5% of blacks, and 6.0% of Asians (P=0.01). However, there were no differences in current alcohol use or injection drug use among the groups (Table 2).
Table 1.
Baseline Characteristics and Etiology of ALF by Race
| Variable | Race | P | ||
|---|---|---|---|---|
|
| ||||
| White | Black | Asian | ||
| N (%) | 758 (81.8) | 119 (12.8) | 50 (5.4) | |
| Male sex | 235 (31.0) | 40 (33.6) | 16 (32.0) | 0.85 |
| Age† | 38 (28-49) | 37 (29-47) | 39.5 (29-56) | 0.42 |
| Years of Education† | 12 (12-15) | 12 (12-15) | 12 (12-15) | 0.86 |
|
| ||||
| Etiology | ||||
|
| ||||
| Acetaminophen | 390 (51.5) | 33 (27.7) | 10 (20.0) | <0.01* |
| Hepatitis A/B/C/E | 63 (8.3) | 23 (19.3) | 13 (26.0) | |
| Drug Induced | 113 (14.9) | 29 (24.4) | 12 (24.0) | |
| Other Viruses | 7 (0.9) | 1 (0.8) | 1 (2.0) | |
| Indeterminate | 103 (13.6) | 18 (15.1) | 8 (16.0) | |
| Other | 82 (10.8) | 15 (12.6) | 6 (12.0) | |
Median (Interquartile Range)
χ2 analysis used for overall comparison
Table 2.
Comorbidities, Medications and Laboratory Values by Race
| Variable | Race | P | ||
|---|---|---|---|---|
|
| ||||
| White | Black | Asian | ||
| N (%) | 758 (81.8) | 119 (12.8) | 50 (5.4) | |
| Comorbidities | ||||
|
| ||||
| Psychiatric Disorders | 231 (30.5) | 16 (13.4) | 4 (8.0) | <0.01 |
| Hypertension | 88 (11.6) | 24 (20.2) | 4 (8.0) | 0.02 |
| Former Polysubstance Abuse | 176 (23.2) | 22 (18.5) | 3 (6.0) | 0.01 |
| Former Intravenous Drug Use | 25 (3.3) | 8 (6.7) | 0 | 0.08 |
| Alcohol Use | 286 (38.1) | 46 (39.7) | 11 (22.0) | 0.06 |
|
| ||||
| Medications | ||||
|
| ||||
| Anesthetics | 19 (2.5) | 1 (0.8) | 1 (2.0) | 0.66 |
| Anti-tuberculosis Agents | 8 (1.1) | 2 (1.7) | 1 (2.0) | 0.73 |
| Antibiotics | 95 (12.5) | 10 (8.4) | 7 (14.0) | 0.40 |
| Anticonvulsants | 53 (7.0) | 7 (5.9) | 0 | 0.14 |
| Estrogen | 69 (9.1) | 4 (3.4) | 2 (4.0) | 0.06 |
| Herbals | 29 (3.8) | 4 (3.4) | 8 (16.0) | <0.01 |
| Anti-psychotics | 186 (24.5) | 15 (12.6) | 2 (4.0) | <0.01 |
| Fresh Frozen Plasma | 383 (50.5) | 52 (43.7) | 22 (44) | 0.28 |
| Sedation | 362 (47.8) | 38 (31.9) | 19 (38) | <0.01 |
|
| ||||
| Encephalopathy | ||||
|
| ||||
| Presentation† | 1 ( 1-1 ) | 1 ( 1-1 ) | 1 ( 1-2 ) | 0.67 |
| Maximal† | 3 ( 2-4 ) | 3 ( 2-4 ) | 3 (1-4 ) | 0.96 |
|
| ||||
| Laboratory Values | ||||
|
| ||||
| Blood Urea Nitrogen† | 19 (9-35) | 13 (6-28) | 13 (7-24) | <0.01 |
| Creatinine† | 1.8 (0.9-3.2) | 1.6 (0.9-3.1) | 1.2 (0.9-2.4) | 0.11 |
| Glucose† | 116 (91-153) | 108 (73-133) | 126 (97-147) | 0.01 |
| Albumin | 2.9 (1.6) | 2.6 (0.6) | 2.6 (0.7) | 0.16 |
| Bilirubin† | 6.6 (3.7-17.7) | 18.3 (5.8-25.3) | 20.2 (5.9-27.5) | <0.01 |
| Aspartate Aminotransferase† | 1962 (595-6214) | 928 (356-2830) | 1025 (251-2241) | <0.01 |
| Alanine Aminotransferase† | 2352 (811-5220) | 1057 (359-2760) | 1008 (269-2600) | <0.01 |
| Alkaline Phosphatase† | 142 (103-193) | 171 (121-239) | 121 (93-157) | <0.01 |
| International Normalized Ratio† | 2.7 (2.0-4.4) | 2.5 (2.0-4.0) | 2.8 (1.9-5.0) | 0.54 |
| Ammonia† | 100 (61-170) | 75 (57-127) | 92 (45-152) | 0.31 |
| MELD | 32.7 (9.3) | 33.9 (8.1) | 33.0 (9.6) | 0.42 |
Median (Interquartile Range)
With respect to medications, whites were more likely to be on estrogen preparations and Asians were more likely to have been on an herbal supplement (P=0.06 and P<0.01, respectively). Additionally, whites were more likely to be on anti-psychotic agents than other racial groups, an observation that is congruent with the highest burden of psychiatric illness being found in this group.
Certain laboratory data did differ for the groups on presentation however no differences were noted among the groups with respect to MELD scores (Table 2).
Etiology of ALF
The most common etiology of ALF among all groups, but particularly among whites, was acetaminophen toxicity [51.5% vs. 27.7% for Blacks (P<0.01) and 20.0% for Asians (P<0.01)]. Asians were more likely to suffer from viral hepatitis induced ALF, particularly Hepatitis B (26.0%). Blacks and Asians were more likely to have drug induced ALF than whites (P=0.01).
Mortality
In total, 305 deaths occurred within the entire cohort over the 21 day period of follow up. Of these, 285 occurred in the racial groups being studied. Two hundred twenty-eight of 758 (30%) white subjects, 46 of 119 (39%) black subjects, and 11 of 50 (22%) Asian subjects died over the course of the study.
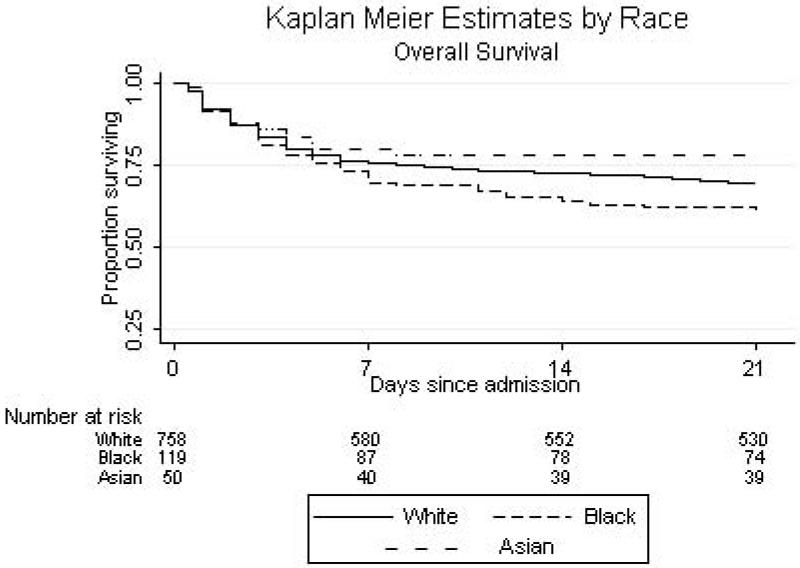
Kaplan Meier
Kaplan Meier analysis of time to death was performed for all groups (Figure 1a). There was no statistically significant difference found between the groups (P=0.10) across all time points in the Kaplan Meier analysis. Survival at 21 days was not significantly different between the groups (P=0.07).
Figure 1.
a: Unadjusted Kaplan Meier Survival Estimates by Race, Overall Survival. Overall log rank statistic: P=0.10.
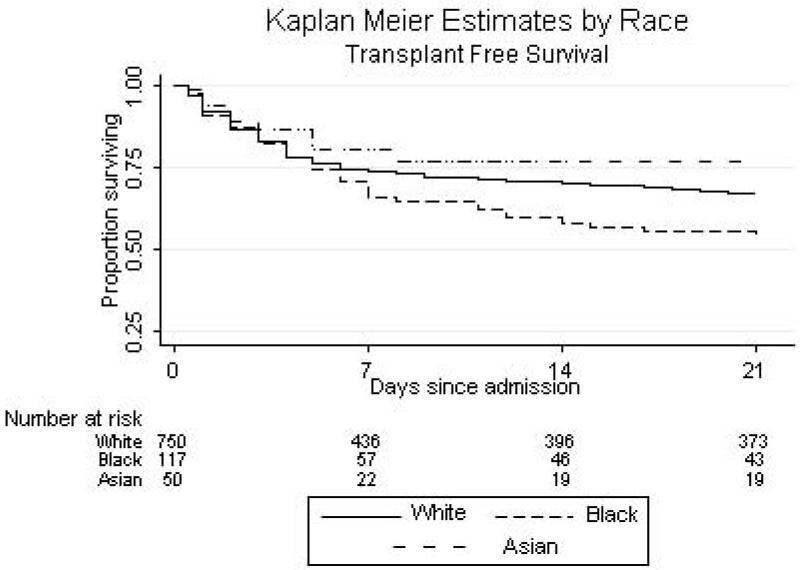
b: Unadjusted Kaplan Meier Survival Estimates by Race, Transplant Free Survival. Overall log rank statistic: P=0.08.
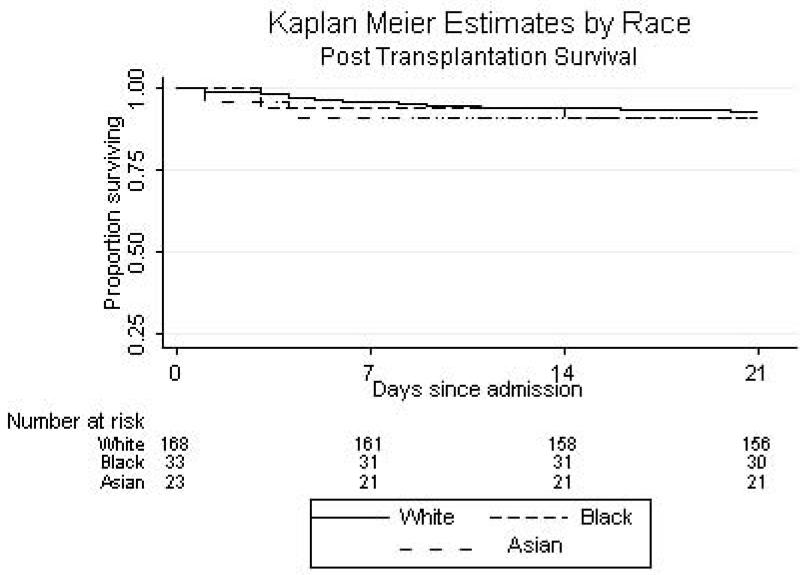
c: Unadjusted Kaplan Meier Survival Estimates by Race, Post Transplantation Survival. Overall log rank statistic: P=0.21.
Cox Proportional Hazards
In Cox proportional hazards modeling, the adjusted risk of death was 1.17 for blacks (95% CI 0.83 – 1.66) and 0.74 among Asians (95% CI 0.38 – 1.41).
Secondary analyses were conducted to examine transplant-free survival and post-liver transplantation survival by censoring at the time of liver transplantation and thereby ameliorating the survival benefit afforded by transplantation. The Kaplan Meier estimates for transplant-free survival were not significantly different (P=0.08, Figure 1b). In Cox adjusted analyses, the risk of death did not differ from whites in any group [blacks (HR 1.13, 95% CI 0.79-1.64) and Asians (HR 0.78, 95% CI 0.39-1.54)]. In the immediate post-liver transplantation period, 12 whites (54.6%), 3 blacks (13.6%), and 2 Asians (9.1%) died (Table 3). Of these 17 subjects, the causes of death included cardiac, cerebrovascular collapse in the setting of cerebral edema, sepsis and multiorgan system failure. While the sample was small, the causes of death did not differ by race.
Table 3.
Hazard Ratios for Mortality Endpoints and Odds Ratios for Transplantation by Race
| Overall Mortality | |||
|
| |||
| Race | Number of Deaths N(%) |
Unadjusted HR HR (95% CI) |
Adjusted HR* HR (95% CI) |
| White | 228 (80.0) | Reference | Reference |
| Black | 46 (16.1) | 1.32 (0.96-1.81) | 1.17 (0.83-1.66) |
| Asian | 11 (3.9) | 0.71 (0.39-1.31) | 0.74 (0.38-1.41) |
|
| |||
| Transplant Free Mortality (Censoring at time of Transplant) | |||
|
| |||
| Race | Number of Deaths N(%) |
Unadjusted HR HR (95% CI) |
Adjusted HR* HR (95% CI) |
| White | 213 (80.7) | Reference | Reference |
| Black | 42 (15.9) | 1.37 (0.98-1.90) | 1.13 (0.79-1.64) |
| Asian | 9 (3.4) | 0.72 (0.37-1.40) | 0.78 (0.39-1.54) |
|
| |||
| Post Transplant Mortality | |||
|
| |||
| Race | Number of Deaths N(%) |
Unadjusted HR HR (95% CI) |
Adjusted HR* HR (95% CI) |
| White | 12 (70.6) | Reference | Reference |
| Black | 3 (17.6) | 1.29 (0.36-4.58) | NA |
| Asian | 2 (11.8) | 1.25 (0.28-5.60) | NA |
|
| |||
| Transplantation | |||
|
| |||
| Race | Number of Transplants N(%) |
Unadjusted HR OR (95% CI) |
Adjusted HR* OR (95% CI) |
| White | 168 (75.0) | Reference | Reference |
| Black | 33 (14.7) | 1.64 (1.03–2.61) | 0.96 (0.54-1.71) |
| Asian | 23 (10.3) | 2.80 (1.52–5.16) | 1.50 (0.72-3.13) |
Adjusted models were adjusted for the following variables: age, gender, primary etiology of ALF, presenting level of hepatic encephalopathy, log transformed bilirubin, log transformed inr, log transformed creatinine, alt and region.
Transplantation
In the cohort, a total of 250 subjects were transplanted. The 224 subjects with complete data were utilized for this subgroup analysis. In this group, 168 subjects (75.0%) were white, 33 (14.7%) were black, and 23 (10.3%) were Asian. In unadjusted logistic regression focusing on those subjects deemed eligible for transplantation, Asians were more likely to be transplanted (OR 2.80, 95% CI 1.52-5.16). In the adjusted analysis, this finding was attenuated (OR 1.50, 95% CI 0.72-3.13). The rate of liver transplantation for blacks was not significantly different from whites (Table 3).
Subgroup Analyses
In subgroup analyses, each etiology of ALF was explored separately. For acetaminophen toxicity, no statistically significant mortality differences were noted among the groups. Additionally, for viral hepatidities (A/B/C/E), drug induced liver injury and indeterminate hepatitis, no statistically significant differences were found in adjusted analyses.
When years of education, a marker of socioeconomic status, was included in the fully adjusted models, there was a difference in the hazard of death between the racial groups. As this variable was missing for many subjects, a sensitivity analysis was performed using only patients with complete data. When this subset of subjects was analyzed, level of education had no bearing on the association between race and mortality or transplantation (data not shown).
Ethnicity
Of the subjects, 685 (88.1%) were non-Hispanic whites and 93 (11.9%) were Hispanic or Latino. While ethnic groups were not different with respect to gender, they were different with respect to age (P=0.01). Hispanics were less likely to have psychiatric diagnoses and a history of substance abuse (data not shown). They were also more likely to be on anti-tuberculosis agents at the time of ALF presentation but less likely to be on antipsychotics (P<0.01 and P<0.01, respectively).
For laboratory parameters, though there were differences noted, there were no differences between Hispanics and non-Hispanic whites for other prognostic factors such as level of encephalopathy on presentation. Lastly, Hispanics were less likely to have had acetaminophen toxicity (30.1 % vs. 53.9%) and more likely to have had drug induced liver injury (29.0% vs. 13.4%) as the underlying etiology for their ALF.
In Kaplan Meier analysis of the survival data for ethnicity, there was no statistically significant difference in the survival curves for Hispanics and non-Hispanic whites (P=0.30). In the Cox adjusted analysis, a non-significant difference was noted between Hispanics and non-Hispanic whites in overall mortality (HR 1.31; 95% CI 0.90 – 1.92). Further, Hispanics were more likely to be transplanted for ALF even after adjustment for ALF etiology and other potential confounders (adjusted OR 1.89; 95% CI 1.08 – 3.30).
Discussion
To examine whether there were differences in outcomes for ALF by race and ethnicity, we analyzed data provided by the ALFSG. This is the first study of its kind to evaluate this clinical question. We did not find statistically significant differences in overall mortality between racial and ethnic groups after adjustment for confounders such as etiology of acute liver dysfunction. While this finding was incongruent with our a priori hypothesis, we did demonstrate several differences between the groups for etiology and presentation in this ALF cohort.
In chronic liver disease, it is well documented that socioeconomic status (SES) and race play an important role in the receipt of curative and palliative therapies. Race and SES-related disparities have been well described for liver transplantation,3, 4, 6, 17 invasive procedures such as port-systemic shunting and esophagogastroduodenoscopy for variceal hemorrhage,3 and disease specific therapies for Hepatitis C.18, 19 In ALF, only a few studies have explored such disparities. Our study suggests that in the setting of ALF, 3 week outcomes in patients managed at tertiary care centers do not differ based on race or ethnicity. Further, in our cohort, measures of disease severity and surrogates for socioeconomic factors which were available for review appeared to have no effect on the outcomes of these subjects. Our results are in contrast to the data from chronic liver disease studies in which disease-specific, socioeconomic and patient level factors are thought to influence the outcomes observed in minority patients.4, 20
The acuity of hepatic dysfunction coupled with the necessity to make swift clinical judgments distinguishes this clinical scenario from that of chronic liver disease. Further, differences in disease etiology, access and resource allocation and bias in referral are other attributes which differentiate the two scenarios of ALF and chronic liver disease and thus may in fact help to explain the differences in outcomes. However, given that we did not directly compare these disease processes and further we did not have data to explore questions of referral and access we can only speculate about such differences in minority outcomes.
While no definitive differences were noted in the mortality experience of racial and ethnic groups over the 21 day period of observation, noteworthy differences were found with respect to etiology of ALF and characteristics on presentation in the groups. When we explored the overall prevalence of the etiologies of ALF, we found that the most common etiology of ALF was acetaminophen toxicity, a finding well aligned with prior research.21 Further, the prevalence of acetaminophen induced ALF was higher in whites than in other racial groups. Additionally, women were more likely to present with ALF from acetaminophen toxicity in all racial groups. This finding may reflect an increase in medication use in women and/or a decrease in the ability to detoxify the harmful effects of the active metabolite of acetaminophen. In contrast to the high prevalence of acetaminophen toxicity in whites, Asians bore the burden of the viral hepatidities, particularly that of Hepatitis B.
The etiologic signature of ALF in the racial and ethnic groups may in part be described by other findings noted during the course of this analysis. Firstly, a preceding psychiatric diagnosis was reported more frequently in whites than in other groups. It is unclear whether this demonstrates a true difference in prevalence rates between the groups or a failure to diagnose psychiatric disorders in patients of different socioeconomic and racial backgrounds on the basis of access to care, patient reluctance or true under-diagnosis of such conditions. Prior studies have shown differences in diagnosis and treatment of mental illness based on race.22 Studies have also demonstrated that race, as well as income and health insurance status, play a role in access to and utilization of mental health services. The difference in the use of psychiatric medications is at least in part a reflection of these unmeasured factors. Such disparate rates of psychiatric illness however may explain some of the differences in acetaminophen toxicity noted in the cohort, specifically with the burden of acetaminophen induced ALF noted in whites. Secondly, a difference in medication usage, for instance an increased prevalence of herbal use in Asians, also speaks to the presence of more drug induced etiologies of ALF in this group.
Examination of laboratory data revealed many notable findings as well. Whites were more likely to have higher median markers of renal dysfunction, aminotransferase elevations and less severe hyperbilirubinemia than other groups. These laboratory findings likely reflect the burden of acetaminophen toxicity in this sub-cohort and have been well documented in a prior study of acetaminophen induced ALF.21 While the remaining groups had more drug-induced liver injury and viral hepatitis, there were no differences in level of encephalopathy noted at presentation or maximal level of encephalopathy achieved, factors which are viewed as surrogates of disease severity. This would suggest that the acuity of ALF on presentation to tertiary care centers was similar between the groups with the differences reflecting underlying etiology rather than any true referral bias.
Lastly, we found that Asians and Hispanics were more likely to be transplanted for ALF, a finding attenuated with adjustment for the underlying etiology of ALF in Asians but not in Hispanics. As noted above, both Asians and Hispanics had comparable survival to whites in the cohort. These findings probably reflect the fact that these groups had a higher prevalence of viral hepatitis and drug-induced liver disease, both of which carry a poor prognosis without transplantation. In the era of transplantation, survival for patients with these etiologies of ALF has improved greatly. In the case of Hispanics, this association may have retained statistical significance as a result of residual confounding. However, this finding deserves further study.
This study had several potential limitations. First, while this study is the largest of its kind to investigate ALF outcomes in racial and ethnic groups, the sample sizes noted in these groups remained small. It may therefore be reasonable to repeat this work in a larger cohort of subjects with ALF or once more subjects have been enrolled in the ALF trial. Second, additional investigation of ALF outcomes in racial and ethnic groups at one and two years after liver transplantation is also warranted to explore issues of graft dysfunction and mortality in subjects not transplanted for chronic liver diseases. Third, there may have been misclassification of comorbidities as these were collected from the next of kin or the medical record. Fourth, this study focused on clinical factors and outcomes of ALF patients, and many psychosocial factors were unmeasured and relatively unexplored. There is always concern that more limited access to care may result in late presentation and referral in this disease process. Once a patient is transferred to a tertiary care center, however, such forces appear to have less of an impact on clinical outcomes. Given further information about the disease course prior to presentation and length of time prior to presentation to a tertiary care facility for evaluation may help to clarify some of these issues. Multiple comparisons discussion removed secondary to space limitation.
In summary, this is the first comprehensive study to examine the effect of race and ethnicity on presentation, etiology, and outcomes in ALF. We observed no statistically significant racial disparities with respect to mortality in the setting of ALF in a cohort of subjects managed at tertiary care centers across the United States.
Acknowledgement
The authors would like to take this opportunity to thank James D. Lewis, MD, MSCE and Vincent Lo Re III, MD, MSCE for their careful and detailed review of this manuscript.
Supported by NIDDK grant no. U-01-58369
Abbreviations
- ALF
Acute Liver Failure
- ALFSG
Acute Liver Failure Study Group
- CI
Confidence Interval
- HR
Hazard Ratio
- OR
Odds Ratio
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Institute of Medicine of the National Academies; Mar 15, 2007. http://www.iom.edu/?id=4475&redirect=0. [PubMed] [Google Scholar]
- 2.Smedley BDSA, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academies Press; 2003. [PubMed] [Google Scholar]
- 3.Nguyen GC, Segev DL, Thuluvath PJ. Racial disparities in the management of hospitalized patients with cirrhosis and complications of portal hypertension: a national study. Hepatology. 2007;45:1282–9. doi: 10.1002/hep.21580. [DOI] [PubMed] [Google Scholar]
- 4.Reid AE, Resnick M, Chang Y, et al. Disparity in use of orthotopic liver transplantation among blacks and whites. Liver Transpl. 2004;10:834–41. doi: 10.1002/lt.20174. [DOI] [PubMed] [Google Scholar]
- 5.Nair S, Eustace J, Thuluvath PJ. Effect of race on outcome of orthotopic liver transplantation: a cohort study. Lancet. 2002;359:287–93. doi: 10.1016/S0140-6736(02)07494-9. [DOI] [PubMed] [Google Scholar]
- 6.Ananthakrishnan AN, Saeian K. Racial differences in liver transplantation outcomes in the MELD era. Am J Gastroenterol. 2008;103:901–10. doi: 10.1111/j.1572-0241.2008.01809.x. [DOI] [PubMed] [Google Scholar]
- 7.Ostapowicz G, Fontana RJ, Schiodt FV, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med. 2002;137:947–54. doi: 10.7326/0003-4819-137-12-200212170-00007. [DOI] [PubMed] [Google Scholar]
- 8.Higgins PD, Fontana RJ. Liver transplantation in acute liver failure. Panminerva Med. 2003;45:85–94. [PubMed] [Google Scholar]
- 9.Hoofnagle JH, Carithers RL, Jr., Shapiro C, et al. Fulminant hepatic failure: summary of a workshop. Hepatology. 1995;21:240–52. [PubMed] [Google Scholar]
- 10.Lee WM, Squires RH, Jr., Nyberg SL, et al. Acute liver failure: Summary of a workshop. Hepatology. 2008;47:1401–15. doi: 10.1002/hep.22177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Grady JG, Alexander GJ, Hayllar KM, et al. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology. 1989;97:439–45. doi: 10.1016/0016-5085(89)90081-4. [DOI] [PubMed] [Google Scholar]
- 12.Wigg AJ, Gunson BK, Mutimer DJ. Outcomes following liver transplantation for seronegative acute liver failure: experience during a 12-year period with more than 100 patients. Liver Transpl. 2005;11:27–34. doi: 10.1002/lt.20289. [DOI] [PubMed] [Google Scholar]
- 13.Schiodt FV, Atillasoy E, Shakil AO, et al. Etiology and outcome for 295 patients with acute liver failure in the United States. Liver Transpl Surg. 1999;5:29–34. doi: 10.1002/lt.500050102. [DOI] [PubMed] [Google Scholar]
- 14.Trey C, Davidson CS. The management of fulminant hepatic failure. Prog Liver Dis. 1970;3:282–98. [PubMed] [Google Scholar]
- 15.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations’. Journal of the American Statistical Association. 1958;53:457–481. [Google Scholar]
- 16.Cox D. Regression models and life tables. J R Stat Soc B. 1972;34:187–220. [Google Scholar]
- 17.Eckhoff DE, McGuire BM, Young CJ, et al. Race: a critical factor in organ donation, patient referral and selection, and orthotopic liver transplantation? Liver Transpl Surg. 1998;4:499–505. doi: 10.1002/lt.500040606. [DOI] [PubMed] [Google Scholar]
- 18.Trooskin SB, Navarro VJ, Winn RJ, et al. Hepatitis C risk assessment, testing and referral for treatment in urban primary care: role of race and ethnicity. World J Gastroenterol. 2007;13:1074–8. doi: 10.3748/wjg.v13.i7.1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheung RC, Currie S, Shen H, et al. Chronic hepatitis C in Latinos: natural history, treatment eligibility, acceptance, and outcomes. Am J Gastroenterol. 2005;100:2186–93. doi: 10.1111/j.1572-0241.2005.00240.x. [DOI] [PubMed] [Google Scholar]
- 20.Nguyen GC, Thuluvath PJ. Racial disparity in liver disease: Biological, cultural, or socioeconomic factors. Hepatology. 2008;47:1058–66. doi: 10.1002/hep.22223. [DOI] [PubMed] [Google Scholar]
- 21.Larson AM, Polson J, Fontana RJ, et al. Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study. Hepatology. 2005;42:1364–72. doi: 10.1002/hep.20948. [DOI] [PubMed] [Google Scholar]
- 22.Weinick RM, Zuvekas SH, Cohen JW. Racial and ethnic differences in access to and use of health care services, 1977 to 1996. Med Care Res Rev. 2000;57(Suppl 1):36–54. doi: 10.1177/1077558700057001S03. [DOI] [PubMed] [Google Scholar]