Abstract
Quantification of the degree of pulmonary edema in organ donors is useful for assessing the clinical severity of pulmonary edema, determining response to therapy, and as an endpoint for therapeutic trials. Currently, there is no accurate non-invasive method for assessing the degree of pulmonary edema. We tested the performance of a four quadrant chest radiographic scoring system compared to quantification of pulmonary edema by excised lung weight in 84 donors whose lungs were not used for transplantation. Chest radiographs were taken 3.6 ± 3.0 hours prior to organ procurement and were scored by two of the authors. Lungs were excised without perfusion and individually weighed. The chest radiographic scoring system had good performance: correlation between total radiographic score and total lung weight of 0.61, p <0.001. Performance of the scoring system was improved when chest radiographs with atelectasis were excluded (r = 0.79, p < 0.001). The area under the receiver operator characteristic curve for detection of moderate pulmonary edema (total lung weight > 1000g) was 0.80. This chest radiographic scoring system may potentially be used to assess the clinical severity of pulmonary edema and may be useful as part of the evaluation of donors for suitability for lung transplantation.
Keywords: pulmonary edema, organ donor, lung transplantation, chest radiograph
INTRODUCTION
Acute pulmonary edema is common in brain dead organ donors and may be due to either elevations in lung vascular pressure (usually cardiogenic) or an increase in lung vascular permeability (acute lung injury) (1). Quantification of the degree of pulmonary edema in organ donors is useful for assessing the clinical severity of pulmonary edema, determining response to therapy, and as an endpoint for therapeutic trials designed to either prevent or minimize lung edema or accelerate the resolution of pulmonary edema. A variety of invasive measures for quantifying the extent of pulmonary edema have been assessed in clinical studies (2, 3). Quantification of pulmonary edema by measurement of extravascular lung water using a single or double indicator technique can provide an estimation of the degree of pulmonary edema. Such measurements of extravascular lung water have been shown to be associated with severity of illness and clinical outcomes (4) in patients with acute respiratory failure and have been used a clinical endpoint in clinical trials (5).
However, the measurement of extravascular lung water using a single or double indicator method requires the insertion of venous and arterial catheters into large blood vessels with attendant risks. A non-invasive method for quantifying the degree of acute pulmonary edema could have broad application in both clinical and research settings including assessment of organ donors. We hypothesized that a chest radiograph scoring system based on scoring of the degree of pulmonary edema in each of the four quadrants of the lung fields would provide an accurate assessment of the degree of pulmonary edema as assessed by the total excised lung weight. To test this hypothesis, we developed and applied a chest radiographic scoring system to chest radiographs taken immediately prior to organ procurement in organ donors whose lungs were not used for transplantation. Chest radiographic scores were compared to lung weights determined after lung resection at the time of organ procurement. We selected this population for the study because pulmonary edema is common complication of neurologic injury and brain death (6), and because of the unique availability of resected lungs from the subjects for quantitative assessment of the degree of pulmonary edema.
METHODS
Donors
The study was done using chest radiograph and lung physiologic data obtained as part of the Beta-Agonist for Oxygenation in Lung Donors (BOLD) study, a randomized, blinded, placebo-controlled trial of nebulized albuterol versus placebo to enhance the resolution of pulmonary edema in 500 brain dead organ donors (NCT00310401). As part of the BOLD study protocol, when a surgical team is available, lungs that are not used for transplantation are resected at the time of organ procurement without perfusion and transported to the laboratory of an investigator (MAM) for physiological, biochemical and molecular biology studies. All decisions about acceptability of lungs for transplantation were made by the donor management and surgical transplantation teams and the investigators were not involved in these decisions. Consecutive brain dead organ donors enrolled from April 2007 through April 2009 in the BOLD study were eligible for inclusion in the current study if they completed the organ donation process, had one or more lungs that were not used for transplantation and a surgical team was available to resect the lungs at the time of organ procurement for transport to our laboratory. Consent for research was obtained from the next of kin, and the study was approved by the Medical Board of the California Transplant Donor Network.
Chest radiographic scoring
Chest radiographs that were obtained within 24 hours of organ procurement were scored for each donor. All chest radiographs were taken in the anterior-posterior plane in the supine position. If more than one chest radiograph was available within this time frame, the radiograph closest to organ procurement was utilized. All chest radiographs were scored by consensus of two of the investigators (LBW and HRO) using a scoring system that was modified from the Murray Lung Injury Score (7) without knowledge of the clinical data or lung physiological data. Each lung on the radiograph was divided into two quadrants by a horizontal line through the center of the hilum. For each quadrant, a score between 0 and 4 was assigned with 0 representing no edema, 1 representing edema in 0–25% of the quadrant, 2 representing edema in 25–50% of the quadrant, 3 representing edema in 50–75% of the quadrant and 4 representing edema in > 75% of the quadrant. In addition to the edema scoring, the presence or absence of atelectasis (defined as hazy opacity with volume loss) in each lung field was noted.
Lung fluid balance measurements
Lungs were resected en bloc from donors without perfusion and transported at 4°C to the laboratory. The total weight of each lung was recorded as a quantitative index of pulmonary edema (8).
Statistical Analysis
All statistical analysis was done using PASW Statistics 18.0 (SPSS Inc., Chicago, IL). For comparison of lung weights to chest radiographic scoring, the total chest radiograph scores for left and right lungs were compared to the left and right lung weights and Pearson correlation coefficients were calculated. For all analyses, a P value ≤ 0.05 was considered statistically significant. To assess the ability of the chest radiograph score to detect moderate pulmonary edema (total lung weight > 1000 g) the area under the receiver operator characteristic (ROC) curve, was calculated. The ROC curve is a plot of sensitivity against 1 – specificity and the area under the ROC curve can be used to assess the performance of a diagnostic test (9).
RESULTS
Donor Characteristics
Between April 2007 and April 2009, 280 donors were enrolled in the BOLD study. Of these, 247 donors (494 lungs) completed the organ donation process and 149 lungs were transplanted. Of the remaining 345 non-transplanted lungs, 238 lungs were resected from 120 donors for research and were potentially available for the study. Resection occurred if a surgical team was available. Two lungs were not resected due to trauma to the organ. From these 120 donors with lungs resected for research, portable supine anteroposterior chest radiographs taken within 24 hours of organ procurement were available in 84 of the 120 donors and these radiographs were matched with the corresponding resected lungs for analysis (162 lungs, 79 left lungs, 83 right lungs). Weight measurement was missing for 6 lungs. Clinical characteristics of the 84 organ donors are in Table 1. The mean time between final chest radiograph and operative aortic cross clamping for organ procurement was 3.6 ± 3.0 hours. Because the BOLD study is a blinded randomized clinical trial that is still accruing subjects, information about study arm assignment (placebo versus albuterol) is not available and is not relevant to the objectives of this study.
Table 1.
Clinical characteristics of 84 brain dead organ donors
| Clinical characteristic | Mean (SD) or n (%) |
|---|---|
| Age (years) | 48 ± 13 |
| Male gender | 47 (56%) |
| Caucasian | 56 (67%) |
| Body mass index (kg/m2) | 28.7 ± 6.5 |
| Cause of brain death | |
| CNS hemorrhage/infarct | 39 (46%) |
| Head trauma | 27 (32%) |
| Anoxic brain injury | 15 (18%) |
| Other | 3 (4%) |
| Current smoker | 32 (38%) |
| Primary reason ruled out for lung donation | |
| Lung function/blood gases | 54 (65%) |
| Medical history/imaging findings | 15 (18%) |
| Social history/positive serologies | 2 (2%) |
| Other (age, no match etc.) | 12 (15%) |
| Not recorded | 1 (1%) |
Chest Radiographic Scoring
Chest radiographic scores are summarized in Table 2. Mean scores for pulmonary edema were higher in the lower quadrants than the upper quadrants which may, in part, reflect the high percentage of films that had evidence of atelectasis (75%) or pleural effusions (45%), both of which tended to be more prominent in the bases. Patients who were obese [body mass index (BMI) > 30] tended to have higher chest radiographic scores (6.5 ± 3.5 vs. 5.2 ± 3.4, p = 0.08).
Table 2.
Summary of chest radiographic scoring in 84 donors
| Criterion | Mean (SD) or N(%) |
|---|---|
| Chest radiographic scoring | |
| Right upper quadrant score | 0.9 ± 1.0 |
| Right lower quadrant score | 1.9 ± 1.2 |
| Right lung total score | 2.7 ± 1.8 |
| Left upper quadrant score | 0.9 ± 1.0 |
| Left lower quadrant score | 2.0 ± 1.1 |
| Left lung total score | 2.9 ± 1.9 |
| Other radiographic findings | |
| Right atelectasis | 38 (45%) |
| Left atelectasis | 54 (64%) |
| Right pleural effusion | 17 (20%) |
| Left pleural effusion | 35 (42%) |
Lung Fluid Balance Analysis
Mean lung weights (400 ± 130 g on the left, 444 ± 148 g on the right) were higher than normal lung weight (approximately 250 g)(10), indicating the presence of pulmonary edema.
Comparison of Chest Radiographic Scoring to Lung Weights
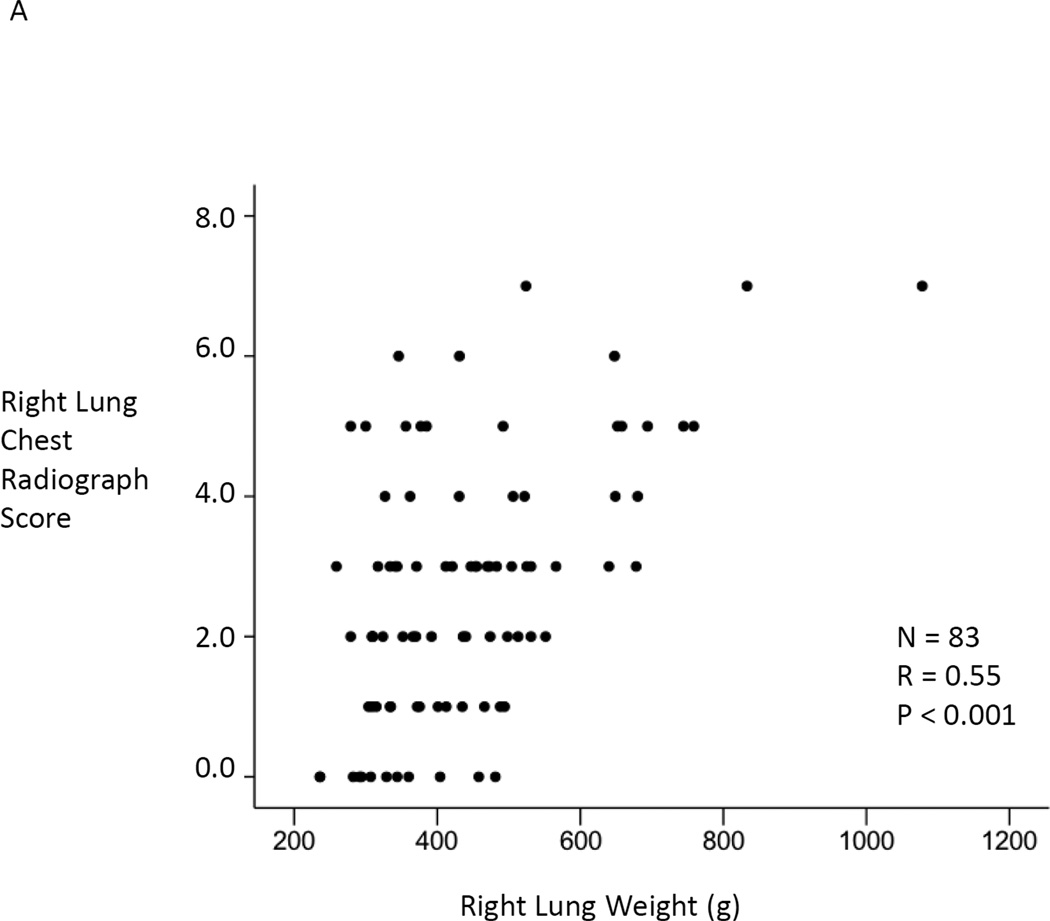
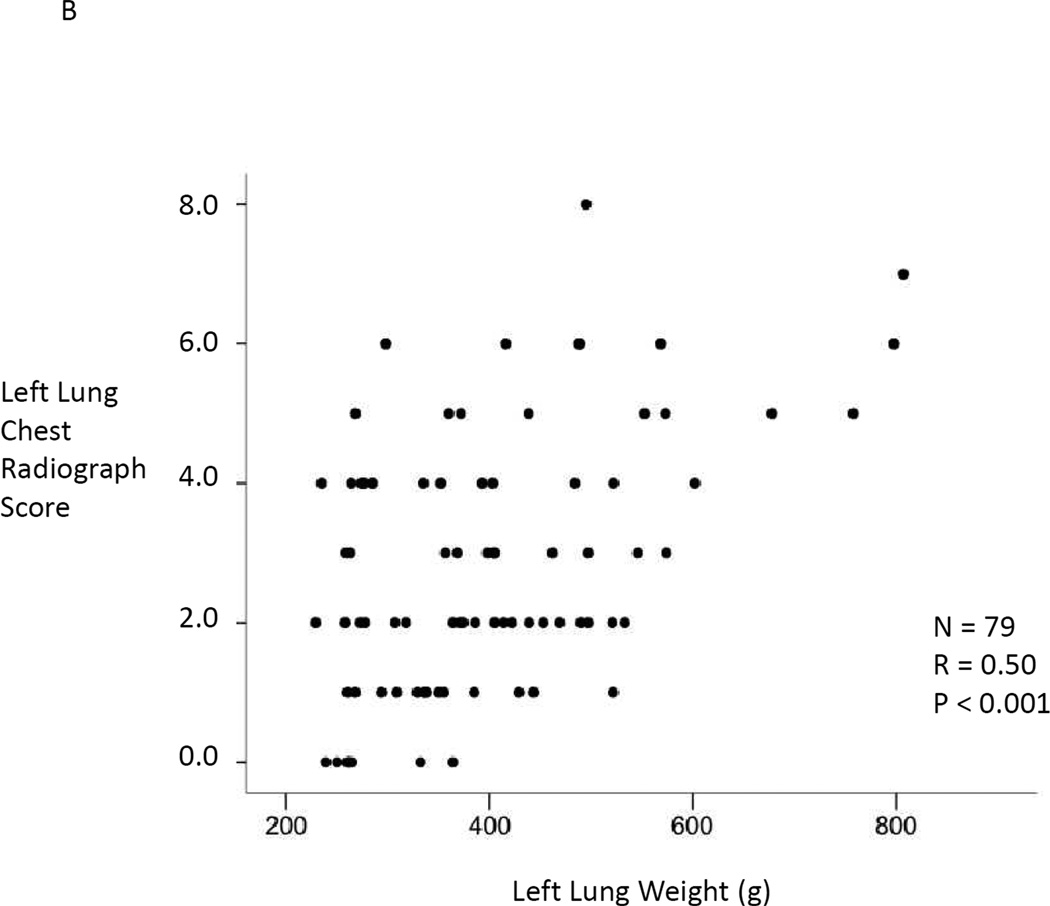
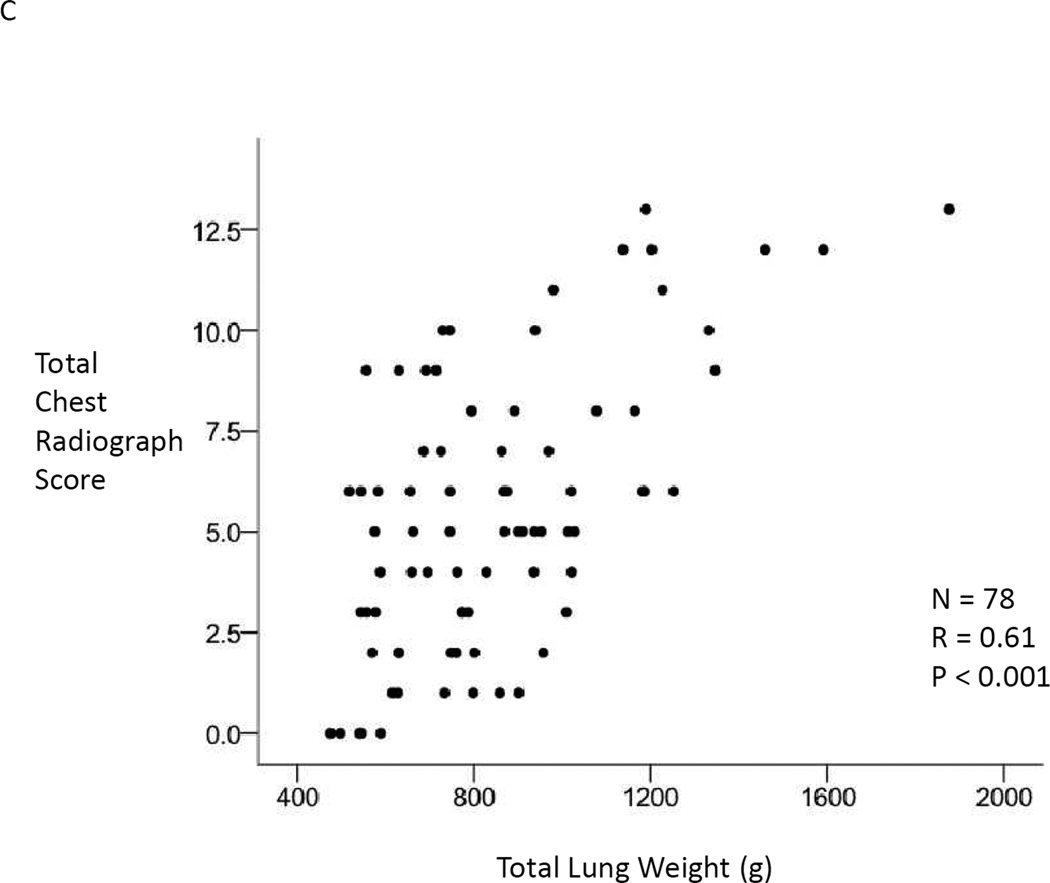
Right lung weight was significantly correlated with the total right chest radiographic score (r = 0.55, p < 0.001, Figure 1A). Left lung weight was significantly correlated with the total left chest radiographic score (r = 0.50, p < 0.001, Figure 1B). When the total combined weight of both lungs was compared to the total combined chest radiographic score for all quadrants, the correlation coefficient improved to r = 0.61 (p < 0.001, Figure 1C). To insure that differences in normal lung weight based on body size did not impact the results, we analyzed the lung weights adjusting for height or predicted body weight. Adjusting lung weights for patient height or predicted body weight had a minimal effect on the correlation coefficient for the comparison between total lung weight and total chest radiographic score ( r = 0.65 and r = 0.67 respectively). When obese patients with a body mass index greater than 30 (n = 33) were excluded, correlations between lung weight and chest radiographic scores improved (Right: r = 0.65, p < 0.001; Left: r = 0.63, p < 0.001; Total: r = 0.70, p < 0.001).
Figure 1.
Panel A, comparison of total right lung chest radiographic score to right lung weight. N = 83. Pearson’s correlation coefficient r = 0.55, p < 0.001. Panel B, comparison of total left lung chest radiographic score to left lung weight. N = 79. Pearson’s correlation coefficient r = 0.50, p < 0.001. Panel C, comparison of total right and left lung chest radiographic score to total right and left lung weight. Only donors who had both lungs resected for weight were included, N = 78. Pearson’s correlation coefficient r = 0.61, p < 0.001.
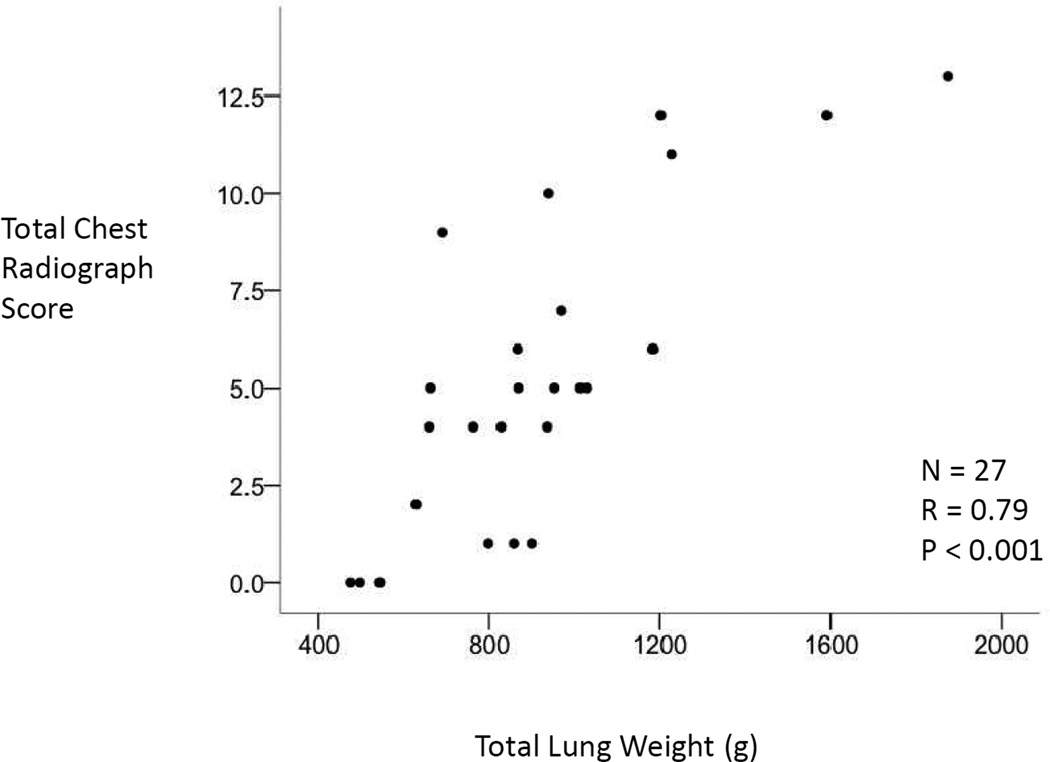
Because the presence of atelectasis can mimic pulmonary edema or consolidation, we also repeated the analysis excluding chest radiographs with atelectasis (n = 27). Correlations between chest radiographic scores and the right and left lung weights (Right: r = 0.58, p < 0.001, Left r = 0.73, p < 0.001) as well as the total lung weights (r = 0.79, p < 0.001, Figure 2) were stronger in the subset of chest radiographs without atelectasis. This effect was more prominent for the left lung, likely because atelectasis was more common on the left side.
Figure 2.
Comparison of total right and left lung chest radiographic score to total right and left lung weight. Only donors who had no evidence of atelectasis were included, N = 27. Pearson’s correlation coefficient r = 0.79, p < 0.001.
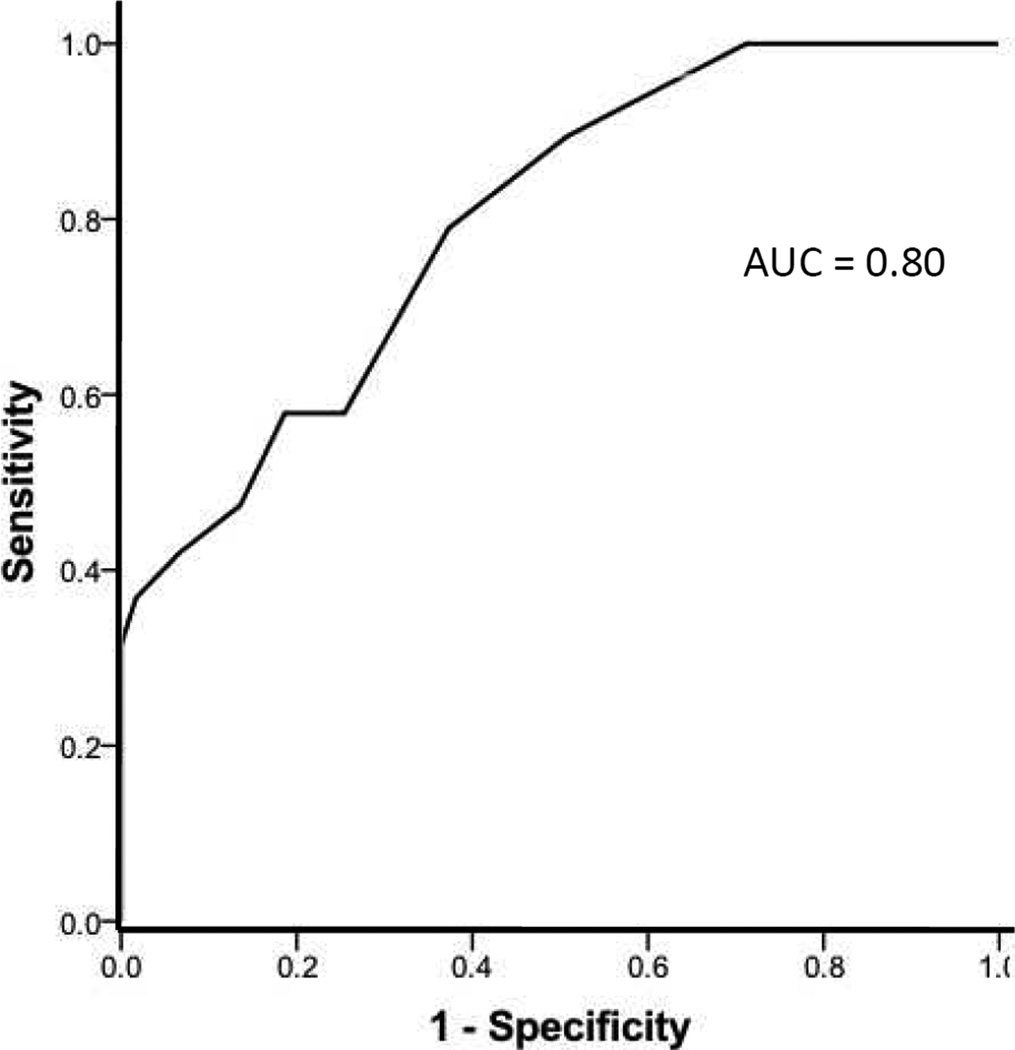
To assess the performance of the chest radiograph score for detection of moderate pulmonary edema with alveolar flooding (total lung weight > 1000 g) the area under the receiver operator characteristic (ROC) curve was calculated. The area under the curve was 0.80 (Figure 3).
Figure 3.
Receiver operator characteristic curve for the use of the chest radiographic scoring system to detect moderate pulmonary edema with a total lung weight of greater than 1000g. Area under the curve (AUC) is 0.80.
DISCUSSION
In order to test a non-invasive method for quantifying the degree of acute pulmonary edema in organ donors, we compared a chest radiograph scoring system to excised lung weight, a quantitative assessment of the degree of pulmonary edema, in 84 brain dead organ donors. Pre lung-procurement chest radiographic scores were strongly and significantly correlated with total excised lung weight; the best performance was achieved when the total scores for all four quadrants of the chest radiograph were added together for a total radiographic score and compared to the combined weight of the two excised lungs. Association of the radiographic score with the lung weight improved further when obese patients (BMI > 30) were excluded or when chest radiographs with evidence of atelectasis were excluded. Obesity and atelectasis may both interfere with the accurate interpretation of the chest radiograph. Our findings suggest that a simple chest radiographic scoring system can be used to non-invasively estimate the degree of pulmonary edema in organ donors. Potential applications of the chest radiographic scoring system include assessment of clinical severity of pulmonary edema, determining response to therapy, and as an endpoint for therapeutic trials aimed at preventing the formation of or accelerating the resolution of pulmonary edema. In addition, use of this chest radiograph scoring system to estimate the extent of pulmonary edema may have value in the evaluation of donors for suitability for lung transplantation, an important issue that we (11) and others have addressed (12) (13).
To our knowledge, this is the first study in humans to systematically compare chest radiographic scoring of pulmonary edema to quantitative assessment of pulmonary edema by lung weight in excised lungs. Snashall and colleagues (14) induced pulmonary edema experimentally in dogs and compared chest densitometry and chest radiographic scoring to postmortem measures of extravascular lung water. They found a correlation between densitometric assessment of chest radiographs and lung water that was highest in the lower lung zones (r = 0.71) and lower in the upper lung zones (r = 0.45). Chest radiographic scoring was sensitive to changes in lung water of greater than 35% (14). In humans, chest radiographic scoring has been compared to measurement of pulmonary edema by the double indicator techniques (15, 16). Halperin and colleagues (15) compared serial chest radiographs to serial measurements of extravascular lung water in a small study of 12 patients with acute respiratory failure. They divided the lungs into six regions and scored the degree of alveolar edema in each region on a 0 to 65 scale resulting in a total score between 0 and 390. Radiographic scores correlated with the extravascular lung water measurements (r = 0.51), but the change in extravascular lung water over time did not correlate with change in radiographic score. Sivak and colleagues (16) measured pulmonary edema using the double indicator technique compared to radiographic quantitation of pulmonary edema in 14 critically ill patients. Chest radiographs were graded from 1 to 5 depending on the overall amount of edema detected. Chest radiographs were 64% accurate for detecting increased extravascular lung water as measured by the double indicator technique. Neither of these human studies were able to directly quantify the degree of pulmonary edema in excised lungs and thus were limited by the inherent limitations of the double indicator technique for measuring the extent of pulmonary edema (17).
Our study has several strengths. The study was done prospectively in the context of a large randomized clinical trial, and thus we were able to prospectively evaluate a large number (84) of well characterized donors. As such, to our knowledge this is the largest study to date to validate a clinical chest radiographic scoring system against direct measurements of pulmonary edema. Chest radiographs were obtained under typical clinical circumstances in the intensive care unit suggesting that the results should be generalizable to other critically ill patients. Unlike prior clinical studies that compared chest radiographs to estimates of lung water made using double indicator techniques, we were able to directly quantify the extent of pulmonary edema in the patients by weighing the excised lungs after procurement, avoiding many of the potential pitfalls of the double indicator technique.
The study also has some limitations. Only a subset of donors enrolled in the clinical trial had both pre-procurement chest radiographs and excised lung weights available. Although it would be preferable to have measurements on every donor enrolled in the clinical trial, practical concerns limited availability of both chest radiographs and excised lungs. Donors were enrolled at dozens of hospitals across Northern California and at some hospitals the chest radiograph could not be obtained within the required timeframe. At the time of organ procurement, a qualified surgeon to procure lungs for research was not always available. Coroner restrictions limited the availability of both chest radiographs and lungs from some donors. In addition, approximately 25% of the donor lungs were used for transplantation and thus were not available for gravimetric measurement of lung water. Nevertheless, the study still represents a large number of donors and is larger than any prior study evaluating the chest radiographic as a method to estimate the quantity of pulmonary edema. The chest radiographs in the study were not evaluated by radiologists. The fact that the chest radiographs were read by two of the authors (both pulmonary and critical care physicians) and not by radiologists could be viewed as a limitation. However, we wanted to develop a radiographic scoring system that could be readily applied by clinicians, and the use of physician readers rather than radiologists increases the generalizabity of the findings. A third limitation is the variable timeframe between the chest radiograph and the lung procurement with an average interval of 3.6 ± 3.0 hours. It is possible that the chest radiographic scoring system would have even better correlation with the lung weights if all the chest radiographs had been taken immediately prior to organ procurement. Unfortunately, due to the practical limitations of obtaining chest radiographs during the organ procurement process, it was not possible to obtain radiographs in the operating room immediately prior to lung resection.
In summary, a simple four quadrant chest radiographic score performed well to estimate the extent of pulmonary edema in brain dead organ donors when compared to quantification of pulmonary edema in the excised human lung. This chest radiographic scoring system can be used to assess the clinical severity of pulmonary edema, determine response to therapy for acute pulmonary edema, and as an endpoint for therapeutic trials aimed at preventing the formation of or accelerating the resolution of pulmonary edema. In addition, use of this chest radiograph scoring system to estimate the extent of pulmonary edema may have value in the evaluation of donors for suitability for lung transplantation.
ACKNOWLEDGMENTS
We thank the transplant coordinators, advanced practice coordinators, surgical coordinators and staff of the California Transplant Donor Network for their invaluable assistance in enrolling patients in this study. This study was supported by NIH HL081332 (LBW), HL103836 (LBW) and HL51856 (MAM).
Footnotes
Author contributions: Dr. Ware participated in research design, performance of the research, data analysis and writing of the paper. Dr. Neyrinck participated in research design, performance of the research, data analysis and writing of the paper. Dr. O’Neal participated in performance of the research, and writing of the paper. Dr. Lee participated in performance of the research, and writing of the paper. Ms. Landeck participated in research design and performance of the research. Ms. Johnson participated in research design, performance of the research and writing of the paper. Dr. Calfee participated in research design, data analysis and writing of the paper. Dr. Matthay participated in research design, data analysis and writing of the paper. The California Transplant Donor Network participated in performance of the research.
References
- 1.Ware LB, Matthay MA. Clinical practice. Acute pulmonary edema. N Engl J Med. 2005;353(26):2788. doi: 10.1056/NEJMcp052699. [DOI] [PubMed] [Google Scholar]
- 2.Isakow W, Schuster DP. Extravascular lung water measurements and hemodynamic monitoring in the critically ill: bedside alternatives to the pulmonary artery catheter. Am J Physiol Lung Cell Mol Physiol. 2006;291:L1118. doi: 10.1152/ajplung.00277.2006. [DOI] [PubMed] [Google Scholar]
- 3.Brown LM, Liu KD, Matthay MA. Measurement of extravascular lung water using the single indicator method in patients: research and potential clinical value. Am J Physiol Lung Cell Mol Physiol. 2009;297(4):L547. doi: 10.1152/ajplung.00127.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Craig TR, Duffy MJ, Shyamsundar M, McDowell C, McLaughlin B, Elborn JS, et al. Extravascular lung water indexed to predicted body weight is a novel predictor of intensive care unit mortality in patients with acute lung injury. Crit Care Med. 2010;38(1):114. doi: 10.1097/CCM.0b013e3181b43050. [DOI] [PubMed] [Google Scholar]
- 5.Perkins GD, McAuley DF, Thickett DR, Gao F. The beta-agonist lung injury trial (BALTI): a randomized placebo-controlled clinical trial. Am J Respir Crit Care Med. 2006;173(3):281. doi: 10.1164/rccm.200508-1302OC. [DOI] [PubMed] [Google Scholar]
- 6.Avlonitis VS, Fisher AJ, Kirby JA, Dark JH. Pulmonary transplantation: the role of brain death in donor lung injury. Transplantation. 2003;27:1928. doi: 10.1097/01.TP.0000066351.87480.9E. [DOI] [PubMed] [Google Scholar]
- 7.Murray JF, Matthay MA, Luce JM, Flick MR. An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis. 1988;138:720. doi: 10.1164/ajrccm/138.3.720. [DOI] [PubMed] [Google Scholar]
- 8.Staub NC. Pulmonary edema. Physiol Reviews. 1974;54:678. doi: 10.1152/physrev.1974.54.3.678. [DOI] [PubMed] [Google Scholar]
- 9.Bewick V, Cheek L, Ball J. Statistics review 13: Receiver operating characteristic curves. Crit Care. 2004;8:508. doi: 10.1186/cc3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joachim H, Riede UN, Mittermayer C. The weight of human lungs as a diagnostic criterium (distinction of normal lungs from shock lungs by histologic, morphometric and biochemical investigations) Pathol Res Pract. 1978;162(1):24. doi: 10.1016/S0344-0338(78)80129-0. [DOI] [PubMed] [Google Scholar]
- 11.Ware LB, Wang Y, Fang X, Warnock M, Sakuma T, Hall TS, et al. Assessment of lungs rejected for transplantation and implications for donor selection. Lancet. 2002;360:619. doi: 10.1016/s0140-6736(02)09774-x. [DOI] [PubMed] [Google Scholar]
- 12.Yeung JC, Cypel M, Waddell TK, van Raemdonck D, Keshavjee S. Update on donor assessment, resuscitation, and acceptance criteria, including novel techniques--non-heart-beating donor lung retrieval and ex vivo donor lung perfusion. Thorac Surg Clin. 2009;19(2):261. doi: 10.1016/j.thorsurg.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Aigner C, Seebacher G, Klepetko W. Lung transplantation. Donor selection. Chest Surg Clin N Am. 2003;13(3):429. doi: 10.1016/s1052-3359(03)00051-6. [DOI] [PubMed] [Google Scholar]
- 14.Snashall PD, Keyes SJ, Morgan BM, McAnulty RJ, Mitchell-Heggs PF, Mclvor JM, et al. The radiographic detection of acute pulmonary oedema: a comparison of radiographic appearances, densitometry, and lung water in dogs. Br J Radiol. 1981;54:277. doi: 10.1259/0007-1285-54-640-277. [DOI] [PubMed] [Google Scholar]
- 15.Halperin BD, Feeley TW, Mihm FG, Chiles C, Guthaner DF, Blank NE. Evaluation of the portable chest roentgenogram for quantitating extravascular lung water in critically ill adults. Chest. 1985;88(5):649. doi: 10.1378/chest.88.5.649. [DOI] [PubMed] [Google Scholar]
- 16.Sivak ED, Richmond BJ, O'Donavan PB, Borkowski GP. Value of extravascular lung water measurement vs portable chest x-ray in the management of pulmonary edema. Crit Care Med. 1983;11(7):498. doi: 10.1097/00003246-198307000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Effros RM, Pornsuriyasak P, Porszasz J, Casaburi R. Indicator dilution measurements of extravascular lung water: basic assumptions and observations. Am J Physiol Lung Cell Mol Physiol. 2008;294(6):L1023. doi: 10.1152/ajplung.00533.2007. [DOI] [PubMed] [Google Scholar]