Abstract
Miliary mottling on chest radiography is seen in miliary tuberculosis, certain fungal infections, sarcoidosis, coal miner’s pneumoconiosis, silicosis, hemosiderosis, fibrosing alveolitis, acute extrinsic allergic alveolitis, pulmonary eosinophilic syndrome, pulmonary alveolar proteinosis, and rarely in hematogenous metastases from the primary cancers of the thyroid, kidney, trophoblasts, and some sarcomas. Although very infrequent, miliary mottling can be seen in primary lung cancers. Herein, we report the case of a 28-year-old female with chest X-ray showing miliary mottling. Thoracic computed tomography (CT) features were suggestive of tuberculoma with miliary tuberculosis. CT-guided fine needle aspiration cytology confirmed the diagnosis as lower-lobe, left lung non-small cell carcinoma (adenocarcinoma). It is rare for the non-small cell carcinoma of the lung to present as miliary mottling. The rarity of our case lies in the fact that a young, non-smoking female with miliary mottling was diagnosed with non-small cell carcinoma of the lung.
Key Words: Non-small cell lung carcinoma, Adenocarcinoma lung, Miliary
Introduction
Miliary mottling consists of opacities, between 0.5 to 2 mm in size, in chest radiography. In Indian settings, although miliary mottling is more commonly associated with miliary tuberculosis, it can be seen in other conditions such as fungal infections (histoplasmosis, coccidioidomycosis, cryptococcosis, and blastomycosis), sarcoidosis, Coal miner’s pneumoconiosis, silicosis, hemosiderosis, fibrosing alveolitis, acute extrinsic allergic alveolitis, pulmonary eosinophilic syndrome, and pulmonary alveolar proteinosis.1
Miliary mottling can be seen rarely in the secondary malignancies of the lung.2,3 The incidence of lung cancer is higher in males and peaks between age 55 and 65 years. The miliary pattern in chest radiography is very rare in patients with primary lung cancer.4,5
Here is a rare case of a young, female patient with non-small cell carcinoma of the lung presenting as miliary mottling.
Case Description
A 28-year-old housewife presented with a history of fever, cough, and chest pain of 15 days duration.
The patient was apparently normal 15 days prior to admission, when she developed a fever that was gradually progressive, moderate to high grade, and associated with chills. She had cough associated with mucoid expectoration, which was non-blood tinged. She also had a pricking type of chest pain, which was central and non-radiating.
The patient was not a diabetic or a hypertensive, and nor was she a known case of ischemic heart disease or tuberculosis. Also, she was not a smoker or an alcoholic. There was no family history of tuberculosis or close contact with tuberculosis.
On examination, the patient was afebrile with a pulse of 90 beats per minute and blood pressure of 130/80 mmHg. General physical examination did not reveal pallor, icterus, clubbing, cyanosis, edema, or lymphadenopathy. Thyroid examination was within normal limits, and respiratory, cardiovascular, abdominal, and central nervous systems were clinically normal.
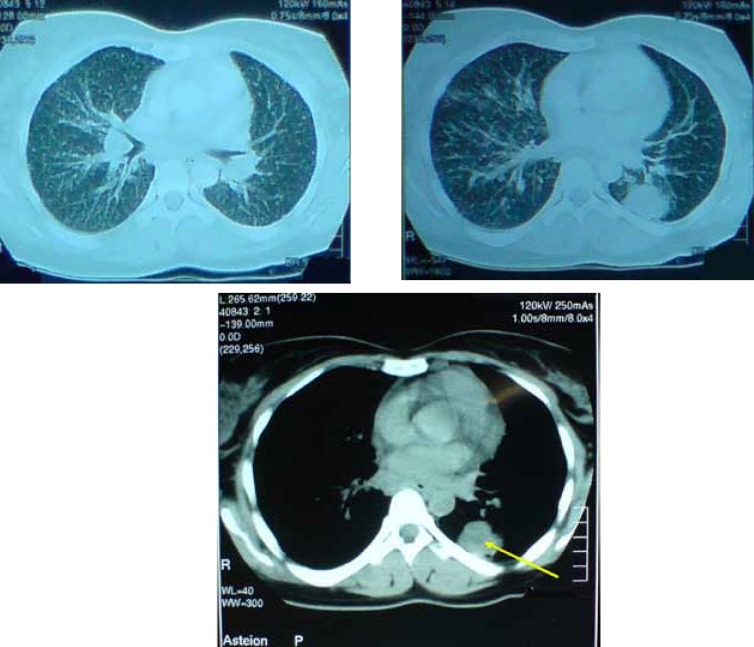
Hemogram revealed a total count of 11,900 /mm3. Additionally, the differential count was within normal limits and the erythrocyte sedimentation rate (ESR) was 35 mm/h. Sputum acid fast bacilli (AFB) (3 samples) were negative. A Gram stain showed plenty of epithelial cells, pus cells, Gram-positive cocci, and gram-negative bacilli. Human immunodeficiency virus (HIV) was non-reactive. Liver function and renal function tests were within normal limits. The Mantoux test was negative. Chest X-ray showed miliary mottling (figure 1). Thoracic computed tomography (CT) revealed a small, mildly enhancing, nodular lesion containing central density involving the posterior basal segment of the left lower lobe with a few enlarged pretracheal, retrocaval, aortopulmonary, and right hilar lymph nodes. In addition, numerous tiny nodular lesions were scattered in both lung fields and there was no pleural effusion. The CT features were suggestive of tuberculoma with miliary tuberculosis (figure 2).
Figure 1.
Chest radiograph, showing miliary mottling
Figure 2.
Thoracic computed tomography, demonstrating a small, mildly enhancing, nodular lesion containing central density (arrow) with a few enlarged pretracheal, retrocaval, aortopulmonary and right hilar lymph nodes. Additionally, numerous tiny nodular lesions are scattered in both lung fields, suggestive of tuberculoma with miliary tuberculosis
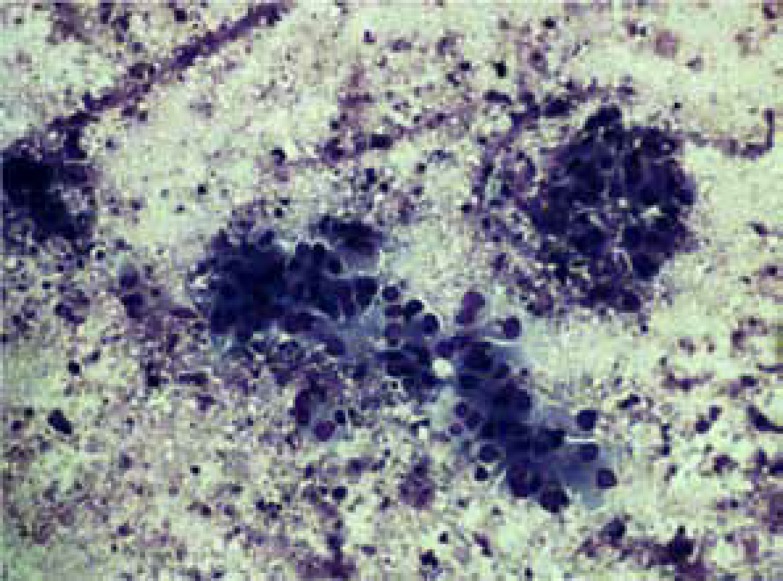
CT-guided fine needle aspiration cytology (FNAC) was performed to confirm the diagnosis of tuberculosis. However, FNAC sprang a surprise by revealing tumor cells arranged in an acinar pattern with a hyperchromatic nucleus with a background of hemorrhage and necrosis, suggestive of a lower-lobe, left lung non-small cell carcinoma (adenocarcinoma) (figure 3).
Figure 3:
Computed tomography-guided fine needle aspiration cytology smear, showing pleomorphic tumor cells arranged in an acinar pattern, with a hyperchromatic nucleus with a background of hemorrhage and necrosis, suggestive of non-small cell carcinoma (adenocarcinoma).
Discussion
The word “lung cancer” is applied to tumors that arise from the respiratory epithelium (bronchi, bronchioles, and alveoli), whereas mesotheliomas, lymphomas, and stromal tumors are different from epithelial lung cancer. The incidence of lung cancer is at its highest between ages of 55 and 65 years. Active smoking increases the relative risk of developing lung cancer by about thirteenfold, and long-term passive exposure to cigarette smoke increases it by 1.5 fold. According to the World Health Organization (WHO) classification, four major cell types constitute 88% of all primary lung neoplasms: squamous carcinomas; small-cell carcinomas; adenocarcinomas; and large cell carcinomas. Individual cell types have distinct natural histories and responses to therapy, and treatment decisions are chiefly made on the basis of whether a tumor is classified as a small cell carcinoma or as one of non-small cell subtypes. Squamous and small cell carcinomas commonly present as a central mass with endobronchial growth, while adenocarcinomas and large cell carcinomas present as peripheral nodules or masses often with pleural involvement. A subtype of adenocarcinomas called bronchioloalveolar carcinomas grow along the alveoli without invasion and they can present radiologically as a single mass or a diffuse, multi-nodular lesion or even as fluffy infiltrate.6
Our patient was a young, non-smoking female (28 years old). She presented with cough, fever, and chest pain. Her chest radiograph demonstrated miliary mottling. Consequently, miliary tuberculosis was considered as an initial diagnosis. When three samples of sputum for AFB and the Mantoux test proved negative and thoracic CT showed a nodular lesion suggestive of tuberculoma, the patient was subjected to CT-guided FNAC, which completely changed the diagnosis to a non-small cell carcinoma of the lung. For further management, the patient was referred to a higher oncology center, where she received chemotherapy. She survived for 8 weeks, but finally succumbed to her illness.
The literature contains a small number of similar cases reported as miliary never-smoking adenocarcinoma of the lung.7 Our patient also showed striking similarities to the 5 patients reported by Umeki8 in 1993 inasmuch as they also had non-small cell carcinoma (adenocarcinoma) of the lung with miliary metastases to the lung. The author identified these 5 cases in a consecutive cohort of 630 patients and suggested that the prevalence of miliary phenotype might be approximately 1% in Japanese patients. Moreover, he reported a short survival time after the appearance of the miliary lung metastases.
Almost all histological types of lung cancer are secondary to smoking. Be that as it may, lung cancer can be seen in individuals who have never smoked. The most common type of lung cancer occurring in lifetime non-smokers, in females, and in patients belonging to younger age groups is non-small cell carcinoma.6,9
Conclusion
The differential diagnoses of miliary mottling on chest radiography comprise miliary tuberculosis fungal infections (histoplasmosis, coccidioidomycosis, cryptococcosis, and blastomycosis), sarcoidosis, coal miner’s pneumoconiosis, silicosis, hemosiderosis, fibrosing alveolitis, acute extrinsic allergic alveolitis, pulmonary eosinophilic syndrome, pulmonary alveolar proteinosis, and hematogenous metastases from the primary cancers of the thyroid, kidney, trophoblasts, and some sarcomas.
Primary lung cancer with a hematogenous spread may cause miliary shadows. Although nonspecific, this radiographic finding may be helpful in certain cases. However, tissue diagnosis continues to play an important role in establishing the definitive diagnosis.
Acknowledgment
We would like to thank our colleagues in the Pathology Department of JSS Medical College Mysore, Dr. Sunila, Dr. Vijaya B, and Dr. Nandini N M, for their assistance in diagnosis and provision of photographs of slides.
Conflict of interest: None declared
References
- 1.Chandrasekhar HR, Shashikala P, Murthy BN, Vidyasagar B, Rao HL. Bronchioloalveolar carcinoma mimicking miliary tuberculosis. J Assoc Physicians India. 2001;49:281–2. PubMed PMID: 11225147. [PubMed] [Google Scholar]
- 2.Scott JX, Gnananayagam JE, Sundaravalli EK, Thomas G, Shanthly N, Kirubakaran C. Unusual cause for miliary lung mottling in a child. Indian J Chest Dis Allied Sci. 2004;46:291–3. PubMed PMID: 15515831. [PubMed] [Google Scholar]
- 3.Reddy B, Senthil N, Valarmathi , Raju S. Medullary Carcinoma of Thyroid Presenting as Miliary Mottling of the Lung. SRJM. 2010;3:26–9. [Google Scholar]
- 4.Koutsopoulos AV, Mitrouska I, Dambaki KI, Voloudaki A, Vardaki E, Haniotis V, et al. Is a miliary chest pattern always indicative of tuberculosis or malignancy؟. Respiration. 2006;73:379–81. doi: 10.1159/000091191. doi: 10.1159/000091191. PubMed PMID: 16446532. [DOI] [PubMed] [Google Scholar]
- 5.Furqan M, Butler J. Miliary pattern on chest radiography: TB or not TB؟. Mayo Clin Proc. 2010;85:108. doi: 10.4065/mcp.2009.0523. PubMed Central PMCID: PMC2813816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, editors. Harrison’s Principles of Internal Medicine. 7th ed. New York: McGraw-Hill; 2008. pp. 551–2. [Google Scholar]
- 7.Laack E, Simon R, Regier M, Andritzky B, Tennstedt P, Habermann C, et al. Miliary never-smoking adenocarcinoma of the lung: strong association with epidermal growth factor receptor exon 19 deletion. J Thorac Oncol. 2011;6:199–202. doi: 10.1097/JTO.0b013e3181fb7cf1. doi: 10.1097/JTO.0b013e3181fb7cf1. PubMed PMID: 21178715. [DOI] [PubMed] [Google Scholar]
- 8.Umeki S. Association of miliary lung metastases and bone metastases in bronchogenic carcinoma. Chest. 1993;104:948–50. doi: 10.1378/chest.104.3.948. doi: 10.1378/chest.104.3.948. PubMed PMID: 8365317. [DOI] [PubMed] [Google Scholar]
- 9.Subramanian J, Govindan R. Lung cancer in never smokers: a review. J Clin Oncol. 2007;25:561–70. doi: 10.1200/JCO.2006.06.8015. doi: 10.1200/JCO.2006.06.8015. PubMed PMID: 17290066. [DOI] [PubMed] [Google Scholar]