Abstract
Objective
Since the time of Kraeplin, schizophrenia has been thought of as a disorder with progressive deterioration in functioning. An important aspect of functioning is both physical and mental health-related quality of life (HRQoL). The objective of this study was to examine the relationship of age to both mental and physical aspects of HRQoL in individuals with schizophrenia as compared to normal comparison subjects (NCs).
Methods
Middle-aged and older Community-dwelling patients with schizophrenia (N=486) were compared to NCs (N=101). Health related quality of life was measured using the SF-36 Physical Health and Mental Health Component scores. The relationship between age and HRQoL was examined using linear regressions. In addition, we performed exploratory analyses to examine the effects of confounding variables on this relationship, and to examine the effects of age on SF-36 subscales.
Results
Patients with schizophrenia had lower SF-36 Physical and Mental Health Component scores than NCs, and these differences persisted after adjusting for the age difference between the two groups. The relationship between age and mental, but not physical, HRQoL was significantly different between the patients with schizophrenia and the NCs. Specifically, older age was associated with higher mental HRQoL among patients with schizophrenia, but not among the NCs. This difference remained significant after examining multiple potential confounding demographic and clinical variables.
Conclusions
This study found that older age was associated with greater mental health quality of life. Longitudinal studies are warranted to confirm our finding, and to examine potential mechanisms responsible for possible improvement in mental HRQoL with age.
Introduction
Schizophrenia, long considered one of the most serious mental illnesses, results in an annual cost to society exceeding $62 billion (Wu et al., 2005). The functional limitations caused by schizophrenia include impairments in neurocognition (Green, 2006; Savla et al., 2007) working (Lieberman, 2006; Palmer et al., 2002), self-care (Friedman et al., 2002), interpersonal relationships, and daily living skills (Siegel et al., 2006). Although, historically, the expected clinical course of a patient with schizophrenia was thought to be one of functional decline (e.g., Kraeplin's depiction of dementia praecox') (Feighner et al., 1972; Lieberman, 2006; Harvey et al., 1999; Spitzer et al., 1975), data from our group (Heaton et al., 2001; Nayak-Salva et al., 2006; Palmer et al., 2003) and others (Rund, 1998; Kurtz, 2005) have shown that, among non-institutionalized people with schizophrenia, the actual course of the disorder is remarkably stable across the life-span (Heaton et al., 2001; Savla et al., 2007; Palmer et al., 2003; Eyler-Zorrilla et al., 2000). Similarly, psychiatric symptoms tend to be less severe in older compared to younger persons with schizophrenia (Jeste et al., 2003; Huber et al., 1980; Harding et al., 1987).
Although cognition and psychiatric symptoms are important outcomes for patients with schizophrenia, quality of life may be the most meaningful outcome. Health-related quality of life (HRQoL), defined as a patient's self-reported perception of his or her physical, emotional, mental, and functional well-being (Gill and Feinstein, 1994), is a way of measuring the impact that a chronic disease has on a person's life and functioning (Guyatt et al., 1993). Prior studies have reported poor HRQoL in patients with schizophrenia, comparable to that of ambulatory patients with AIDS (Patterson et al., 1996). Factors contributing to poorer quality of life in these patients include depression (Reine et al., 2005) and younger age of onset (Sciolla et al., 2003; Patterson et al., 1997). The SF-36 is the most widely used measure of HRQoL, and has been used across a wide range of disease states (Meijer et al., 2002).
In the general population physical HRQoL declines with age, whereas mental HRQoL is stable (Ware et al., 1994), and chronically institutionalized persons with schizophrenia may be at increased risk of age-related functional decline (a key component of HRQoL) (Harvey et al., 2003). Among community dwelling persons, who make up the vast majority of older patients with schizophrenia, data on the relationship between age and HRQoL has been less clear (Reine et al., 2005).
In this study, we examine the relationship between age and physical and mental HRQoL in a sample of 101 normal comparison subjects (NCs) and 486 older adults with schizophrenia. We hypothesized that patients would have worse physical and mental HRQoL than NCs, and that within both groups, older age would be associated with worse physical and mental HRQoL. In addition, we planned to perform two sets of exploratory analyses. First, we explored the relationship between age and SF-36 subscales, to better understand which aspects of HRQoL were most highly correlated with age. In addition, we examined whether demographic and clinical factors that have been previously related to HRQoL (Patterson et al., 1997; Sciolla et al., 2003; Reine et al., 2005) confounded the relationship between age and SF-36 scores.
Methods
Study Sample
Patients were enrolled as part of clinical research at the University of California San Diego's Advanced Center for Innovation in Services and Intervention Research (ACISIR) between February 1994 and September 2006. The patients with schizophrenia were recruited from outpatient clinics of the San Diego County Adult Mental Health Services, UCSD Healthcare System, board-and-care homes, and the VA. None of the patients met the criteria for remission (Auslander and Jeste, 2004) at the time of study enrollment. Please see Jeste et al (Jeste et al., 2003) for NC recruitment details.
This study was approved by the UCSD IRB and all participants provided written informed consent. All clinical data was obtained by a trained research assistant.
For the current study, we included patients enrolled in the Center who met the following criteria: (a) DSM- IV diagnosis of schizophrenia or schizoaffective disorder, or for NCs absence of DSM-IV disorders; (b) age > 40 years; (c) and baseline SF-36 score. Our Center began using the SF-36 in 1994, but not all studies used this measure. Of the 1234 patients with schizophrenia enrolled in the Center since 1994, 486 had a baseline SF-36 score. Similarly 101 of 247 NCs had this measure. All additional clinical and demographic variables used in this report were baseline measures obtained on average within 7 days of the SF-36.
Health-related Quality of Life (HRQoL)
The SF-36 has two primary scales (Physical Health and Mental Health), each with 4 non-overlapping subscales. The Physical Health Component (PHC) assesses general physical health, bodily pain, physical functioning, and work limitations. The Mental Health Component (MHC) assesses an individual's energy/vitality, social functioning, general mental health, and the extent to which health problems interfere with social activities (i.e., Role Emotional). MCH scores have been found to correlate with other measures of psychopathology, such as depressive symptoms and psychotic symptoms. The MCH and PHC scores range from 0-100, higher scores indicate better HRQoL, and these scores are standardized with a population mean is 50 and a standard deviation of 10 (Ware, 2000). For patients with schizophrenia, the SF-36 has demonstrated adequate reliability and validity and has been described as a valuable measure of disease burden (Tunis et al., 1999).
Severity of Psychopathology
Severity of psychopathologic symptoms was evaluated with the Positive and Negative Syndrome Scale (PANSS) (Kay et al., 1988), and the 17-item Hamilton Rating Scale for Depression (HamD) (Hamilton, 1960).
Cognition
Neurocognitive deficits were evaluated with the total score from the Mattis Dementia Rating Scale (DRS) (Mattis, 1976).
Additional information
Other data collected contemporaneously with the SF-36 included demographics (age, education, ethnicity), medical conditions, and current psychotropic medications (type and dose).
Statistical Analyses
The demographic characteristics and psychopathology ratings among the patient and NC groups were compared with Analysis of Variance (for continuous variables) or Pearson's Chi-square (for categorical variables).
To test our first hypothesis, that patients would have worse physical and mental HRQoL than NCs, we used ANOVA.
To test our second hypothesis that the relationship between age and HRQoL would be different among patients with schizophrenia than it was for NCs, we used a previously described statistical approach (Baron and Kenny, 1986; Holmbeck, 1997) determine if diagnosis (schizophrenia or normal comparison) moderated the relationship between age and the two SF-36 component scores. A separate linear regression analysis was conducted for PHC and MHC. All two and three ways interactions were included in this model. In each analysis, a significant diagnosis-by-age interaction term would indicate that the relationship between age and HRQoL was different for patients with schizophrenia than it was for the NC participants. To evaluate the effect size of this interaction we used Cohen's q (small= 0.1, medium= 0.3, and large=0.5) (Cohen, 1992).
We also performed two sets of exploratory analyses within the schizophrenia group to: 1. evaluate the relationship between age and SF-36 MHC subscales, and 2. determine whether demographic or clinical factors confounded the relationship between age and HRQoL. The first exploratory analyses used Pearson correlations to examine the relationship between age and the subscales of SF-36 Mental Health Component. The second exploratory analysis used a series of regressions to examine whether a single demographic or clinical variable (e.g., PANSS score) significantly interacted with age, thereby modifying the association between age and mental HRQoL. To examine the effect of each potential confound on the age-SF-36 relationship we ran a separate linear regression for each potential confounding variable (Mausbach et al., 2004).
Results
Demographic characteristics and severity of psychopathology
As shown in Table 1, relative to NCs, patients with schizophrenia were younger, more likely to be male, less likely to be married, and had fewer years of education. The NCs also had a greater number of medical conditions than did the patients with schizophrenia, however after adjusting for the age differences between the two groups, this difference was not significant (F=1.15, p=.28). As expected, the patients with schizophrenia had greater severity of schizophrenia and depressive symptoms, and worse cognitive deficits than the NCs. Approximately 90% of the patients with schizophrenia were taking an antipsychotic medication, with similar proportions taking a first and second generation antipsychotic. Patients taking a second generation antipsychotic were more likely to have enrolled in the Center after 1999, and were younger than those taking a first generation antipsychotic (mean age 53.4 vs. 56.2, p=.003). In addition, just over one third of the patients with schizophrenia were also taking an antidepressant. There was no age difference between those patients with schizophrenia who did and did not take an antidepressant (F=.056, p=.81).
Table 1. Demographic and clinical characteristics of patients with schizophrenia and normal comparison participants (NCs).
| Variable | Normal Comparison participants (N=101) Mean (SD) or %(n) | Schizophrenia Patients (N=486) Mean (SD) or %(n) | Chi-square or F value | Degrees of freedom | p value |
|---|---|---|---|---|---|
| Age (sd) | 62.2 (11.3) | 54.7 (8.6) | 6.33 | 125 | <.001 |
| Gender | |||||
| Male | 36% (36) | 65% (317) | 30.53 | 1 | <.001 |
| Female | 64% (65) | 35% (169) | |||
| Ethnicity | |||||
| White | 61% (62) | 71% (347) | 14.99 | 3 | .003 |
| African American | 13% (13) | 14% (70) | |||
| Latino | 22% (22) | 9% (42) | |||
| Other | 4% (4) | 6% (27) | |||
| Ever Married | |||||
| Married | 70% (71) | 17% (84) | 120.93 | 1 | <.001 |
| Not-married | 30% (30) | 83% (402) | |||
| Living situation | |||||
| Alone | 28% (26) | 23% (104) | 94.77 | 3 | <.001 |
| With others | 72% (68) | 27% (125) | |||
| Board-and-care | 0% (0) | 47% (220) | |||
| Other | 0% (0) | 3% (14) | |||
| Years of Education (sd) | 13.3 (2.5) | 12.7 (2.5) | 2.10 | 144 | .038 |
| Mean number of Axis III conditions (sd) | 1.7 (1.6) | 0.9 (1.4) | 5.3 | 644 | <.001 |
| Age of onset of schizophrenia (sd) | N/A | 28.7(13.0) | |||
| Highest social position-Hollingshead | 3.2 (1.0) | 3.7 (.9) | 4.8 | 503 | <.001 |
| PANSS (sd) | 34.7 (4.6) | 57.5 (14.0) | 28.05 | 476 | <.001 |
| Hamilton (sd) | 2.8 (2.9) | 9.7 (6.2) | 16.51 | 316 | <.001 |
| DRS (sd) | 139.1 (4.5) | 129.6 (14.0) | 10.232 | 385 | <.001 |
| SF-36 PHC(sd) | 47.6 (10.1) | 44.0 (10.8) | 3.27 | 151 | .002 |
| SF-36 MHC (sd) | 55.3 (7.3) | 44.9 (12.2) | 11.372 | 236 | <.001 |
| Typical antipsychotic* | NA | 164 (42.3%) | |||
| Atypical antipsychotic* | NA | 198 (51.0%) | |||
| Mean CPZE dose of antipsychotic (sd) mg/day | NA | 536 (882) | |||
| Antidepressant* | 2 (2%) | 130 (33.5%) | |||
sd = standard deviation, SF36 PHC = SF-36 Physical Health Component score, SF36 MHC = SF=36 Mental Health Component score, NA = not applicable, DRS = Dementia Rating Scale total score, PANSS = positive and negative syndrome scale total score, Ham17 = Hamilton depression rating 17 item total score, CPZE= Chlorpromazine equivalents
124 patients with schizophrenia had no medication information recorded
Primary Analyses
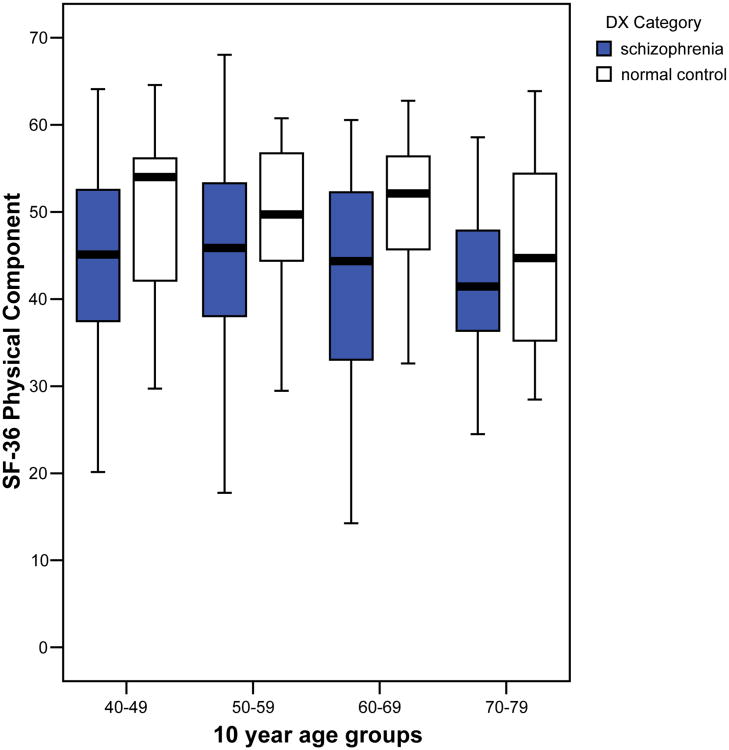
Physical Health Component: Compared to the NCs, the patients with schizophrenia had lower scores on the PHC of the SF-36 (Table 1). For patients with schizophrenia, older age was correlated with worse PHC scores (r =-.112, p=.013), whereas for NCs, the correlation between age and PHC scores was not significant (r = -.158, p= .115) (Figure 1). For the PHC, the age × diagnosis interaction was not significant (F=.57, p=.45), indicating that the relationship between age and PHC scores was similar for patients with schizophrenia and NCs. Other significant variables in the analysis predicting PHC included: age (F= 7.9, p=.005), gender (F=3.9, p=.047), diagnosis (F=16, p<.001), and the age × gender interaction (F=4.6, p=.03).
Figure 1. Relationship between age and SF-36 Physical Health Component score in older persons with schizophrenia (N=486) and normal comparison (N=101).
(Note: box plots are centered on median and extend to 75%ile, tails show 95%ile)
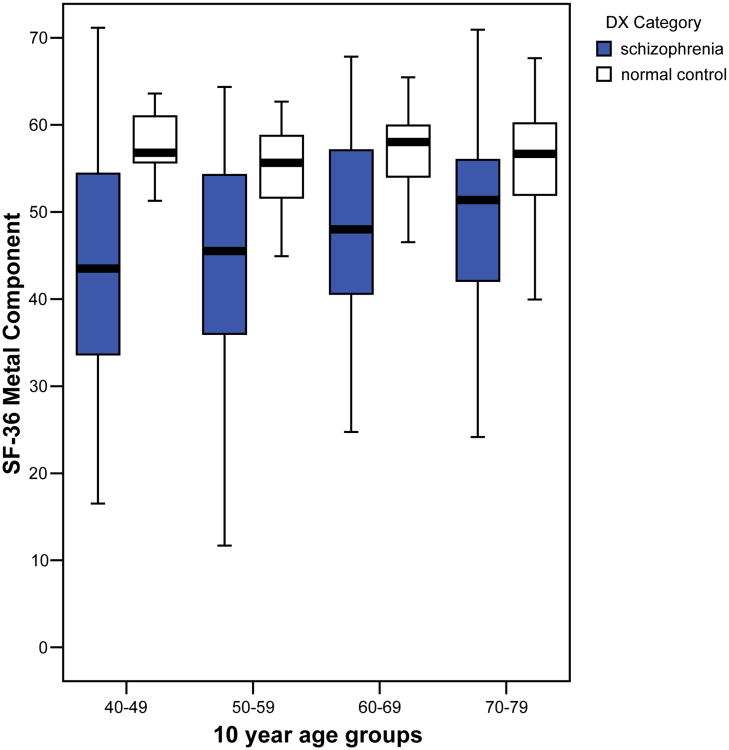
Mental Health Component: Compared to the NCs, the patients with schizophrenia had lower scores on the MHC of the SF-36 (Table 1). Age was positively correlated with SF-36 MHC score for patients with schizophrenia (r=.189, p<.001) but not for NCs (r= -.102, p= .31) (Figure 2). For the MHC, the age × diagnosis interaction was significant (F=6.4, p=.012), indicating that the relationship between age and SF-36 MHC was different for patients with schizophrenia than it was for NCs. The Cohen's q for this interaction was 0.3, indicating a small-to-medium effect size. The only other significant variable in the analysis predicting MHC was diagnosis (F=37, p<.001); gender, gender × diagnosis, age × gender, and age × gender × diagnosis were not significant.
Figure 2. Relationship between age and SF-36 Mental Health Component score in older persons with schizophrenia (N=486) and normal comparison (N=101).
(Note: box plots are centered on median and extend to 75%ile, tails show 95%ile)
Although not the focus of this study, we also examined the relationship between age and other clinical factors. For the NCs, age was correlated with the number of medical conditions (r=.41, p<.001); HamD scores and DRS scores were not associated with age. For the patients with schizophrenia, age was associated with the number of medical conditions (r=.31, p<.001), and DRS score (r=-.167, p=.003), but not PANSS score or HamD score.
Exploratory Analyses
Because the relationship between age and SF-36 MHC scores was significantly different between the patients with schizophrenia and the NCs, whereas the age-PHC relationship was similar between the two groups, we conducted our planned exploratory analyses only for the MHC scores. We first examined the relationship between age and SF-36 Mental Health Component subscales in patients with schizophrenia, and found that age was positively correlated with Social Functioning (r=.110, p=.015), Role-Emotional (r=.154, p=.001), and Mental Health (r=.133, p=.003), but not with Energy/Vitality (r=.015, p=.74).
Our second exploratory analysis examined whether any demographic or clinical variables confounded the observed relationship between older age and higher MHC score in persons with schizophrenia. Results of these analyses indicated that the association between age and MHC scores remained significant after accounting for each of the potential confounding demographic or clinical factors, and that none of the age-by-confound interactions was significant (Table 2). For example, older age was associated with a greater likelihood of living independently, rather than in a board-and-care home, but the age-by-living situation interaction was not significant. Although not the focus of this study, other factors that were associated with SF-36 MHC scores in these analyses were living situation (poorer MHC scores in patients living in board-and-care homes), PANSS scores (higher scores associated with poorer mental HRQoL), and HamD scores (higher scores associated with poorer mental HRQoL).
Table 2. Exploratory analysis of potential confounds that may modify the relationship between age and SF-36 Mental Health Component scores in older persons with schizophrenia (N=486).
| Confound | Age × confound interaction | |||
|---|---|---|---|---|
| Beta | p-value | Beta | p-value | |
| Gender | −.02 | .72 | −.03 | .70 |
| Ethnicity | −.04 | .38 | .06 | .24 |
| Living situation | .12 | .01 | −.06 | .18 |
| Marital status | .02 | .39 | −.05 | .27 |
| Education | −.07 | .13 | .03 | .53 |
| Age of onset | .02 | .71 | .12 | .90 |
| PANSS total | −.35 | <.001 | .01 | .84 |
| HamD | −.53 | <.001 | −.01 | .90 |
| DRS total | −.04 | .50 | .01 | .88 |
| SF-36 PHC | .00 | .93 | .03 | .58 |
note- Each row represents a different analysis predicting SF-36 MHC score. Each analysis included age, potential confounding variable, and age × confound interaction. The Beta value and p-value for age are not shown in this table, but the Beta values ranged from .17-.22, and all of the p values were significant.
PANSS= positive and negative syndrome scale total score
HamD= Hamilton depression rating 17 item total score
DRS= Dementia Rating Scale total score
SF36 PHC= SF-36 Physical Health Component score
Discussion
The principal findings of this study were: 1. Patients with schizophrenia had lower SF-36 PHC and MHC scores than NCs, and these differences persisted after adjusting for the age and gender difference between the two groups; 2. The relationship between age and mental health-related quality of life (HRQoL) was different between the patients with schizophrenia and the NCs. Specifically, older age was associated with higher mental HRQoL among patients with schizophrenia, but not among the NCs. Although the age effect was not large, it is worth noting that the direction of the relationship between mental HRQoL was different between the two groups and that the magnitude of this association corresponded to a small-to-medium effect size. These findings need to be replicated in a prospective study, but they raise the possibility that mental HRQoL may actually improve among older adults with schizophrenia, challenging the Kraeplinian view that the typical course for a patient with schizophrenia is one of progressive deterioration.
The finding of better mental HRQoL in older patients with schizophrenia was further supported by the exploratory analyses of MHC subscales; three of the four SF-36 MHC subscales were positively correlated with age. In addition, the one subscale not correlated with age, Energy/Vitality, would not be expected to improve with age. This observed association between older age and better mental HRQoL in patients with schizophrenia also persisted after examining multiple potential confounding demographic and clinical variables. In particular, although the severity of both schizophrenia and depressive symptoms were associated with SF-36 MHC scores, the relationship between age and mental HRQoL persisted after adjusting for the severity of these psychiatric symptoms.
Our finding of an association between older age and higher mental HRQoL conflicts with results from a prior study from our Center reported by Sciolla et al. (2003) In that study, focused on an examination of the utility of the SF-36 as a measure of HRQoL in older persons with schizophrenias, there was no significant association found between age and SF-36 MHC. However, the risk of type 2 error was higher in the Sciolla et al. study because of a smaller sample size (N=137), and the MHC score was examined only as one of 10 variables in a multivariate analysis. On the other hand, a recent report by Reine et. al. (2005) was consistent with the current findings in that older patients with schizophrenia had better SF-36 MHC than did their younger counterparts. Our current report expands on these prior investigations by studying a larger sample, focusing specifically on the association between age and HRQoL, examining the association between age and SF-36 MHC subscales, and considering whether other clinical and demographic factors confound this relationship. Two additional investigations from our Center have examined the relationship between the age and the Quality of Well Being (QWB) scale, in a subset of patients included in the current investigation, and found no association between age and QWB scores (Patterson et al., 1997; Jeste et al., 2003). However, the QWB combines both physical and mental health into a single summary score, potentially obscuring differences in the relationship between age and mental and physical HRQoL. In contrast, we are aware of one report that found higher SF-36 MHC scores in older patients with schizophrenia relative to their younger counterparts (Reine et al., 2005). Our current report expands on these prior investigations by studying a larger sample, focusing specifically on the association between age and HRQoL, examining the SF-36 MHC subscales, and considering whether other clinical and demographic factors confound this relationship.
There are at least three potential explanations by which older persons with schizophrenia could experience better mental health functioning than their younger counterparts. First, it is possible that our sample reflects a survival cohort, with only the highest functioning patients with schizophrenia survive into old age. Second, older patients may have developed better coping and self-management skills over the course of their illness, possibly including greater acceptance of the illness and greater participation in treatment. Finally, it is possible that the discrepancy between the life situation of people with schizophrenia and that of their peers without a mental illness may lessen as patients with this disorder get older.
Current data are insufficient to fully evaluate the relative role of the above three possible explanations for increased mental HRQoL in schizophrenia. However, one study of coping among persons with schizophrenia over time that the majority of patients demonstrated a stable or increased use of positive coping techniques (Ritsner and Ratner, 2006). Furthermore, increased use of positive coping techniques was associated with a number of mental health benefits, including elevated self-esteem and increased social support. Consistent with the third possibility, a qualitative study of older women with schizophrenia (Pentland et al., 2003), found a lessening of the impact of schizophrenia in their lives as they aged. This list of potential mechanisms is not exhaustive, and these potential mechanisms are not mutually exclusive. Enhanced self-management and reduced perceived impact of illness are two components of the definition of recovery from schizophrenia (Liberman et al., 2002; Bellack, 2006), and whether and how such recovery occurs naturally over the life span should be the subject of future prospective studies (Jeste and Nasrallah, 2003).
There are several limitations of this investigation. First, the data were cross sectional and we are not able to determine whether mental HRQoL changes with age. Future prospective studies should measure HRQoL and psychiatric symptoms over a reasonably lengthy portion of the lifespan to determine whether mental HRQoL improves age. Second, we are not able to determine whether the observed higher mental HRQoL translates into improved real-world functioning. Third, it is possible that only the highest functioning patients with schizophrenia survive to old age, and that the older patients in our sample are somehow healthier and represent a survival cohort. However, other variables including cognition and physical HRQoL were lower in the older patients, suggesting that our finding may be specific to mental HRQoL. Fourth, the patients in this investigation were primarily recruited from community-based settings. Although these patients may not represent chronically institutionalized patients, the vast majority of people with schizophrenia in California (and other states) live in the community (Cohen et al., 2003), and state psychiatric hospitals are almost exclusively for forensic patients (Lamb and Bachrach, 2001). Fifth, we did not measure patient's awareness of their mental illness, which could potentially be altered in older patients. Sixth, we examined current psychiatric symptoms and living situation, but did not have complete data on prior psychiatric hospitalizations, a measure of illness severity, for many participants in this study. It is possible that patients who have never been hospitalized and never had severe symptoms may be a different cohort those with prior hospitalizations and prior episodes of severe symptomatology. In addition, it is possible that some of the age-related interactions might be underpowered relative to the main effect. However the purpose of examining these age-related interactions was to confirm that the main effect of age on SF-36 MHC persisted after examining potential confounds. Future studies should examine the relationship between age and other factors in greater detail. Finally, there were demographic differences between NCs and patients with schizophrenia; the NCs were older and a greater proportion were female. Although our analyses accounted for the differences, future studies should include a comparison group that is more closely matched those with schizophrenia.
Despite the above caveats, the present results are important in suggesting that key aspects of quality of life among patients with schizophrenia may actually improve, rather than remain stable or even deteriorate with age. Although it has previously been reported that only a small proportion of patients with schizophrenia experience remission (Auslander and Jeste, 2004; Nasrallah and Lasser, 2006), these findings hold out the possibility that there may be improvements in mental health related quality of life as people with schizophrenia age. The mechanisms responsible for these potential improvements are as yet unknown, but merit future longitudinal research that may be relevant to the study of recovery over the lifespan.
Acknowledgments
This work was supported, in part, by the National Institute of Mental Health grants 067895, 066248, MH64722, by the Department of Veterans Affairs, and by the Veterans Affairs Center for Excellence on Stress and Mental Health (CESAMH).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Auslander LA, Jeste DV. Sustained remission of schizophrenia among community-dwelling older outpatients. Am J Psychiatry. 2004;161:1490–1493. doi: 10.1176/appi.ajp.161.8.1490. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bellack AS. Scientific and consumer models of recovery in schizophrenia: concordance, contrasts, and implications. Schizophr Bull. 2006;32:432–442. doi: 10.1093/schbul/sbj044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chafetz L, White MC, Collins-Bride G, Nickens J, Cooper BA. Predictors of physical functioning among adults with severe mental illness. Psychiatr Serv. 2006;57:225–231. doi: 10.1176/appi.ps.57.2.225. [DOI] [PubMed] [Google Scholar]
- Cohen CI, Ramirez PM, Kehn M, Magai C, Eimicke J, Brenner R. Assessing quality of life in older schizophrenic persons. Am J Geriatr Psychiatry. 2003;11:658–666. doi: 10.1176/appi.ajgp.11.6.658. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer: quantitative methods in psychiatry. Psychol Bull. 1992;112:115–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Eyler-Zorrilla LT, Heaton RK, McAdams LA, Zisook S, Harris JM, Jeste DV. Cross-sectional study of older outpatients with schizophrenia and healthy comparison subjects: No differences in age-related cognitive decline. Am J Psychiatry. 2000;157:1324–1326. doi: 10.1176/appi.ajp.157.8.1324. [DOI] [PubMed] [Google Scholar]
- Feighner JP, Robins E, Guze SB, Woodruff RA, Winokur G, Munoz R. Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry. 1972;26:57–63. doi: 10.1001/archpsyc.1972.01750190059011. [DOI] [PubMed] [Google Scholar]
- Friedman JI, Harvey PD, McGurk SR, White L, Parrella M, Raykov T, Coleman T, Adler DN, Davis KL. Correlates of change in functional status of institutionalized geriatric schizophrenic patients: focus on medical comorbidity. Am J Psychiatry. 2002;159:1388–1394. doi: 10.1176/appi.ajp.159.8.1388. [DOI] [PubMed] [Google Scholar]
- Gill TM, Feinstein AR. A critical appraisal of the quality of quality-of-life measurements. JAMA. 1994;272:619–626. [PubMed] [Google Scholar]
- Green MF. Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J Clin Psychiatry. 2006;67:e12. [PubMed] [Google Scholar]
- Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118:622–629. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harding CM, Brooks GW, Ashikaga T, Strauss JS, Breier A. The Vermont longitudinal study of persons with severe mental illness, I. Methodology, study sample and overall status 32 years later. Am J Psychiatry. 1987;144:718–726. doi: 10.1176/ajp.144.6.718. [DOI] [PubMed] [Google Scholar]
- Harvey PD, Bertisch H, Friedman JI, Marcus S, Parrella M, White L, Davis KL. The course of functional decline in geriatric patients with schizophrenia: Cognitive functional and clinical symptoms as determinants of change. Am J Geriatr Psychiatry. 2003;11:610–619. doi: 10.1176/appi.ajgp.11.6.610. [DOI] [PubMed] [Google Scholar]
- Harvey PD, Silverman JM, Mohs RC, Parrella M, White L, Powchik P, Davidson M, Davis KL. Cognitive decline in late-life schizophrenia: A longitudinal study of geriatric chronically hospitalized patients. Biol Psychiatry. 1999;45:32–40. doi: 10.1016/s0006-3223(98)00273-x. [DOI] [PubMed] [Google Scholar]
- Heaton RK, Gladsjo JA, Palmer BW, Kuck J, Marcotte TD, Jeste DV. Stability and course of neuropsychological deficits in schizophrenia. Arch Gen Psychiatry. 2001;58:24–32. doi: 10.1001/archpsyc.58.1.24. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: Examples from the child-clinical and pediatric psychology literatures. J Consult Clin Psychol. 1997;65:599–610. doi: 10.1037//0022-006x.65.4.599. [DOI] [PubMed] [Google Scholar]
- Huber G, Gross G, Schuttler R, Linz M. Longitudinal studies of schizophrenia patients. Schizophr Bull. 1980;6:592–605. doi: 10.1093/schbul/6.4.592. [DOI] [PubMed] [Google Scholar]
- Jeste DV, Nasrallah HA. Schizophrenia and aging: No more dearth of data? (Editorial) Am J Geriatr Psychiatry. 2003;11:584–587. doi: 10.1176/appi.ajgp.11.6.584. [DOI] [PubMed] [Google Scholar]
- Jeste DV, Twamley EW, Eyler Zorrilla LT, Golshan S, Patterson TL, Palmer BW. Aging and outcome in schizophrenia. Acta Psychiatr Scand. 2003;107:336–343. doi: 10.1034/j.1600-0447.2003.01434.x. [DOI] [PubMed] [Google Scholar]
- Kay SR, Opler LA, Lindenmayer JP. Reliability and validity of the positive and negative syndrome scale for schizophrenics. Psychiatry Res. 1988;23:99–110. doi: 10.1016/0165-1781(88)90038-8. [DOI] [PubMed] [Google Scholar]
- Kurtz MM. Neurocognitive impairment across the lifespan in schizophrenia: an update. Schizophr Res. 2005;74:15–26. doi: 10.1016/j.schres.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Lamb HR, Bachrach LL. Some perspectives on deinstitutionalization. Psychiatr Serv. 2001;52:1039–1045. doi: 10.1176/appi.ps.52.8.1039. [DOI] [PubMed] [Google Scholar]
- Liberman RP, Kopelowicz A, Ventura J, Gutkind D. Operational criteria and factors related to recovery from schizophrenia. International Review of Psychiatry. 2002;14:256–272. [Google Scholar]
- Lieberman JA. Neurobiology and the natural history of schizophrenia. J Clin Psychiatry. 2006;67:e14. [PubMed] [Google Scholar]
- Mattis S. Dementia Rating Scale. Psychological Assessment Resources, Inc.; Odessa, FL: 1976. [Google Scholar]
- Mausbach BT, Coon DW, Depp C, et al. Ethnicity and time to institutionalization of dementia patients: a comparison of Latina and Caucasian female family caregivers. J Am Geriatr Soc. 2004;52:1077–1084. doi: 10.1111/j.1532-5415.2004.52306.x. [DOI] [PubMed] [Google Scholar]
- Meijer CJ, Schene AH, Koeter WHJ. Quality of life in schizophrenia measured by the MOS SF-36 and the Lancashire Quality of Life Profile: A comparison. Acta Psychiatr Scand. 2002;105:293–300. doi: 10.1034/j.1600-0447.2002.1198.x. [DOI] [PubMed] [Google Scholar]
- Nasrallah HA, Lasser R. Improving patient outcomes in schizophrenia: achieving remission. J Psychopharmacol. 2006;20:57–61. doi: 10.1177/1359786806071248. [DOI] [PubMed] [Google Scholar]
- Nayak-Salva G, Moore DJ, Roesch SC, Heaton RK, Jeste DV, Palmer BW. An evaluation of longitudinal neurocognitive performance among middle-aged and older schizophrenia patients: Use of mixed-model analyses. Schizophr Res. 2006;83:215–223. doi: 10.1016/j.schres.2005.12.851. [DOI] [PubMed] [Google Scholar]
- Palmer BW, Bondi MW, Twamley EW, Thal L, Golshan S, Jeste DV. Are late-onset schizophrenia-spectrum disorders a neurodegenerative condition? Annual rates of change on two dementia measures. J Neuropsychiat Clin Neurosci. 2003;15:45–52. doi: 10.1176/jnp.15.1.45. [DOI] [PubMed] [Google Scholar]
- Palmer BW, Heaton RK, Gladsjo JA, Evan JD, Patterson TL, Golshan S, Jeste DV. Heterogeneity in functional status among older outpatients with schizophrenia: employment history, living situation, and driving. Schizophr Res. 2002;55:205–215. doi: 10.1016/s0920-9964(01)00218-3. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Kaplan RM, Grant I, Semple SJ, Moscona S, Koch W, Harris MJ, Jeste DV. Quality of well-being in late life psychosis. Psychiatry Res. 1996;63:169–181. doi: 10.1016/0165-1781(96)02797-7. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Semple SJ, Shaw WS, Halpain M, Moscona S, Grant I, Jeste DV. Self-reported social functioning among older patients with schizophrenia. Schizophr Res. 1997;27:199–210. doi: 10.1016/S0920-9964(97)00078-9. [DOI] [PubMed] [Google Scholar]
- Pentland W, Miscio G, Eastabrook S, Krupa T. Aging women with schizophrenia. Psychiatr Rehabil J. 2003;26:290–302. doi: 10.2975/26.2003.290.302. [DOI] [PubMed] [Google Scholar]
- Reine G, Simeoni MC, Auquier P, Loundou A, Aghababian V, Lancon C. Assessing health-related quality of life in patients suffering from schizophrenia: a comparison of instruments. Eur Psychiatry. 2005;20:510–519. doi: 10.1016/j.eurpsy.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Ritsner MS, Ratner Y. The long-term changes in coping strategies in schizophrenia: temporal coping types. J Nerv Ment Dis. 2006;194:261–267. doi: 10.1097/01.nmd.0000207361.81947.52. [DOI] [PubMed] [Google Scholar]
- Rund BR. A review of longitudinal studies of cognitive functions in schizophrenia patients. Schizophr Bull. 1998;24:425–435. doi: 10.1093/oxfordjournals.schbul.a033337. [DOI] [PubMed] [Google Scholar]
- Savla GN, Moore DJ, Palmer BW. Cognitive functioning in schizophrenia. In: Mueser KT, Jeste DV, editors. Clinical Handbook of Schizophrenia. Guilford Press; New York: 2007. [Google Scholar]
- Sciolla A, Patterson TL, Wetherell J, McAdams LA, Jeste DV. Functioning and well-being of middle-aged and older patients with schizophrenia; Measurement with the 36-item short-form (SF-36) health survey. Am J Geriatr Psychiatry. 2003;11:629–637. doi: 10.1176/appi.ajgp.11.6.629. [DOI] [PubMed] [Google Scholar]
- Siegel SJ, Irani F, Brensinger CM, Kohler CG, Bilker WB, Ragland JD, Kanes SJ, Gur RC, Gur RE. Prognostic variables at intake and long-term level of function in schizophrenia. Am J Psychiatry. 2006;163:433–441. doi: 10.1176/appi.ajp.163.3.433. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J, Robins E. Research Diagnostic Criteria (RDC) for a Selected Group of Functional Disorders. New York State Psychiatric Institute; New York: 1975. [Google Scholar]
- Tunis SL, Croghan TW, Heilman DK, Johnstone BM, Obenchain RL. Reliability, validity, and application of the medical outcomes study 36-item short-form health survey (SF-36) in schizophrenic patients treated with olanzapine versus haloperidol. Med Care. 1999;37:478–691. doi: 10.1097/00005650-199907000-00008. [DOI] [PubMed] [Google Scholar]
- Ware JE. [Accessed 10-24-06];2000 http://www.sf-36.org/tools/SF36.shtml.
- Ware JE, Kosinski M, Keller SD. SF-36 Physical and Mental Health Summary Scales: A User's Manual. The Health Institute, New England Medical Center; Boston: 1994. [Google Scholar]
- Wu EQ, Birnbaum HG, Shi L, Ball DE, Kessler RC, Moulis M, Aggarwal J. The economic burden of schizophrenia in the United States in 2002. J Clin Psychiatry. 2005;66:1122–1129. doi: 10.4088/jcp.v66n0906. [DOI] [PubMed] [Google Scholar]