Abstract
Background
The purpose of this study is to test the agreement between energy expenditure estimate of the SenseWear® Armband Pro3 (SWA) (BodyMedia, Pittsburgh, PA) and the Omron HJ-720 (Omron Healthcare, Kyoto, Japan) step counter with indirect calorimetry (IC) as a gold standard in older individuals with type 1 and type 2 diabetes mellitus while walking on a treadmill.
Subjects and Methods
In total, six men (60.3±3.1 years old) and 13 women (51.1±11.0 years old) with type 1 or type 2 diabetes mellitus were included in the study. Each subject performed three 15-min walking sessions with different combinations of speed and incline (3 km/h, 0%; 4 km/h, 0%; 5 km/h, 5%) on a treadmill. Energy expenditure (EE) was simultaneously measured by the SWA, Omron, and IC. Mean over-/underestimation and Pearson's correlation coefficients were used for statistical evaluation of the agreement between tested methods and IC.
Results
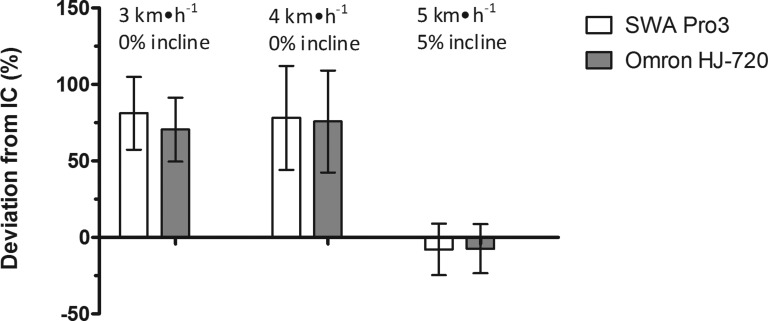
At the speed of 3 km/h with 0% incline, mean overestimation of +81.19±23.81% was found for SWA (r=0.79, P<0.001) and +70.51±20.91% for Omron (r=0.77, P<0.001). At the speed of 4 km/h and 0% incline, mean overestimation found for SWA was +78.18±33.96% (r=0.63, P<0.01) and +75.77±33.36% for Omron (r=0.52, P<0.05). At the level of high-intensity exercise at the speed of 5 km/h and 5% incline, mean underestimation was −7.88±16.86% for SWA (r=0.74, P<0.001) and −7.37±16.07% for Omron (r=0.75, P<0.001).
Conclusions
Both methods led to considerable overestimation of calculated EE in level walking and a relatively minor underestimation during fast uphill walking.
Background
All patients with diabetes should have the opportunity to benefit from the many valuable effects of physical activity.1 Monitoring physical activity and the prediction of energy expenditure (EE) continue to be difficult tasks to carry out outside the laboratory setting. Essentially, the most accurate methods are those working on metabolic principles.2 As a gold standard, indirect calorimetry (IC) performed by a mobile gas-exchange analyzer and the double-labeled water technique (DLW) are used.3 These methods are suitable for research purposes, where accurate data on EE are needed. Both, however, require technical equipment, and their use is limited in practical terms.4 We take the above-described methods as a benchmark for estimating EE outside the laboratory. For a more extensive use in population surveys, other methods, which are less expensive and require no or very little technical equipment, are more suitable. For an indicative estimate of EE in everyday activities, accelerometric devices are commonly used. These systems are often recommended for individuals with diabetes.
Older individuals with type 1 and type 2 diabetes usually display worse anthropometric parameters. Consequently, they prefer to exercise at lower speeds, which may influence the estimation of EE in accelerometric tools. Therefore, these devices must be validated specifically for this population. This study determined the accuracy of calculation of EE by the SenseWear® Armband Pro3 (SWA) (BodyMedia, Pittsburgh, PA) and the Omron HJ-720 (Omron Healthcare, Kyoto, Japan) step counter in individuals with diabetes during walking.
Accelerometric systems
Most instruments, inaccurately called “pedometers,” are no longer based on a purely mechanical principle, but rather on the principles of piezoelectric accelerometry. Usually, the instruments contain one, two, or three accelerometric sensors, working in an equal number of mutually perpendicular axes. Based on the number of sensors, the systems are one-dimensional (Caltrac™; Muscle Dynamics Fitness Network, Torrance, CA), two-dimensional (SWA Pro3), or three-dimensional (RT3®; StayHealthy, Monrovia, CA). Accelerometric tools are usually equipped with a software filter detecting “false steps” (caused, e.g., by shocks on a bus drive).5 In practical terms, these systems should be resistant to outer environments (be shock-proof and resistant to temperature oscillation, humidity, friction, or weather conditions).
SWA
The SWA is a two-axis device, fastened to the rear part of the right arm. The instrument contains a thermistor for measuring temperature, a sensor for galvanic skin response, and a system for measuring heat flux (i.e., the amount of heat dissipating from the body). The producer does not provide information on any other sensors.
When comparing results of validation studies, it needs to be pointed out that all models of SWA and especially the firmware are developing constantly. It is therefore important to compare only software for the same model range (in our center, we used firmware version 6.1, although now even version 7 is commercially available).
Subjects and Methods
In total, six men (60.3±3.1 years old) and 13 women (51.1±11.0 years old) with type 1 or type 2 diabetes mellitus were included in the study. The exclusion criteria were as follows: glycosylated hemoglobin (HbA1c) over 7.5%; serious retinopathy (proliferative), macular edema; serious nephropathy, in the proteinuria stage or renal failure; serious neuropathy of the lower limbs, diabetes leg syndrome; repeated unrecognized hypoglycemia, labile diabetes; another acute disease; or other diseases influencing or increasing risks of physical stress, such as decompensated hypertension or unstable angina pectoris.
The project has been approved by the ethics committee of the 2nd Faculty of Medicine, Charles University, Prague, Czech Republic.
Measurement of anthropometric parameters
Prior to the test itself, the following anthropometric parameters were measured: height, weight, step length (as an average of 10 steps), waist and hip girth, and sagittal abdominal diameter by abdominal caliper (Holtain-Kahn, Crymych, United Kingdom) in the standing and lying positions, as well as the body fat percentage, measured by the bioimpedance method (Quadscan 4000; Bodystat®, Douglas, Isle of Man, United Kingdom). Average anthropometric parameters are given in Table 1.
Table 1.
Values of Anthropometric Parameters
| Women | Men | Both | |
|---|---|---|---|
| Height (cm) | 163.7±5.3 | 184.2±5.0 | 170.2±10.7 |
| Weight (kg) | 85.9±8.7 | 102.9±19.4 | 91.3±14.5 |
| Step length (cm) | 65.6±5.1 | 79.2±3.7 | 69.9±7.70 |
| Waist girth (cm) | 105.6±9.3 | 110.8±11.3 | 107.3±9.7 |
| Hip girth (cm) | 114.2±7.0 | 112.0±8.0 | 113.3±7.0 |
| SAD (cm) | |||
| Standing | 30.5±3.6 | 31.8±4.0 | 31.0±3.6 |
| Lying | 25.9±3.4 | 26.6±3.9 | 26.1±3.4 |
| Body fat (%) | 40.3±5.4 | 25.8±4.0 | 35.7±8.3 |
| BMI (kg/m2) | 31.93±2.91 | 30.24±5.04 | 31.5±3.6 |
Data are mean±SD values.
BMI, body mass index; SAD, sagittal abdominal diameter.
Glycemia and blood pressure monitoring
Before the actual testing took place, current glycemia was checked by glucometer (Accu-chek® Performa; Roche Diagnostics, Indianapolis, IN). To undergo the testing, glycemia in the range of 90–270 mg/dL was required. Blood pressure was taken by a calibrated mercury sphygmomanometer (Chirana Injecta; Stará Turá, Slovakia). Maximum tolerated levels of casual blood pressure were 160/100 mm Hg. Glycemia and blood pressure checks as well as subjective feelings were also assessed after the testing.
Testing
The test itself consisted of walking on an electronic treadmill (Marquette T2000; Davis Medical Electronics, Vista, CA) in the laboratory. In order to find the most comfortable speeds (i.e., in our assumption, the speeds most likely to be used in everyday life), first a pilot test was carried out. After that, three different combinations of speed and incline were used to assess EE calculated by the Omron and SWA, respectively, with IC as a reference. Prior to the test, the subjects lacking previous experience with treadmill walking were asked to try it out. Subsequently, the Omron pedometer was fastened on the area of the right spina iliaca anterior superior with a clip. On the right arm, SWA was fastened by a rubber band, in the area above the triceps brachii muscle. Both instruments had been uploaded with the data required: step length and weight for Omron; sex, age, height, smoker/nonsmoker, and upper limb predominance for SWA. For SWA, software version 6.1 was used.
Prior to the test, the participants were introduced to the MedGraphics® VO2000™ breath gas-exchange analyzer (Medical Graphics, St. Paul, MN). Breath gases were collected by a mask connected to the analyzer by an umbilicus. In contrast to a mouthpiece, the mask slightly increases the dead space but is much better tolerated by the subjects (especially during a longer stress protocol) and allows prompt communication with the healthcare professional.
The walking stress protocol consisted of three sessions, each 15 min long, divided by two 3-min breaks. Each session was characterized by a different combination of speed and incline: Session 1, velocity=3 km/h, 0% incline; Session 2, velocity=4 km/h, 0% incline; and Session 3, velocity=5 km/h, 5% incline.
EE calculation
For every measurement, data on O2 consumption and CO2 production, averaged for every three breaths, were downloaded from the MedGraphics VO2000. EE was calculated by the equation of Weir,6 which takes into account varying EE equivalents for a given O2 consumption for various respiratory quotients (RQs): EE (kcal)=(1.1×RQ+3.9)×VO2 (L). For each session, the point of reaching the steady state (SS) was determined on the basis of constant consumption level of O2, most frequently at 2–5 min after the start of every stress test. EE was only calculated for the duration of the SS. The values for the remaining time at the start of each session (i.e., before SS was reached) were replaced by average values of the SS in the given session. For instance, if the interval before reaching SS was 3 min, the EE for the total of 15 min was determined as EE15=(EE12/12)×15, where EE15 stands for EE for the whole 15 min and EE12 stands for EE for the duration of the equilibrium (i.e., 12 min in this particular case).
As a complementary reference we applied an equation that calculates the total EE of walking as a sum of three components7:
basic component (the energy equivalent of consumption of 3.5 mL/kg/min of O2)
horizontal component, depending on the speed (the equivalent of consumption of 0.1 mL/kg/m/min of O2)
vertical component, depending on the speed and incline (the equivalent of consumption of 1.8 mL/kg/m/min of O2×incline in percentages).
For the total EE estimate, we summed up these three components, which made it possible to take into account the speed and the incline as well. This complementary reference is called “equation” in Table 2 and is not displayed in Figure 1.
Table 2.
Mean Deviations of the SenseWear Armband Pro 3 and the Omron HJ-720 from Energy Expenditure Determined by Indirect Calorimetry with 95% Limits of Agreement and Pearson's Correlation Coefficients in Individuals with Diabetes During Walking
| Conditions, device | Lower limit (%) | Mean (%) | Upper limit (%) | r |
|---|---|---|---|---|
| 3 km/h, 0% incline | ||||
| Equation | −22.54 | −0.68 | 21.17 | 0.79** |
| Omron+REE | 29.52 | 70.51 | 111.5 | 0.77** |
| SWA | 34.52 | 81.19 | 127.87 | 0.79** |
| 4 km/h, 0% incline | ||||
| Equation | −22.18 | 15.99 | 54.15 | 0.64* |
| Omron+REE | 10.39 | 75.77 | 141.15 | 0.52 |
| SWA | 11.61 | 78.18 | 144.75 | 0.63* |
| 5 km/h, 5% incline | ||||
| Equation | −16.25 | 11.02 | 38.28 | 0.88** |
| Omron+REE | −38.87 | −7.37 | 24.14 | 0.75** |
| SWA | 40.93 | −7.88 | 25.16 | 0.74** |
Equation data represent results calculated by the three-component mathematical equation.6
P<0.01, **P<0.001.
REE, resting energy expenditure; SWA, SenseWear Armband Pro3.
FIG. 1.
Deviations of SenseWear Armband (SWA) Pro3 and Omron HJ-720 from energy expenditure determined by indirect calorimetry (IC) in individuals with diabetes during walking. Data are expressed in percentages (error bars are±1 SD).
Statistical analysis
A statistical comparison of EE levels collected by the Omron accelerometer, by the SWA, and those provided by IC as a reference was performed in GraphPad® (San Diego, CA) software. We calculated the Pearson's correlation coefficients and 95% limits of agreement of the tested methods and IC.8
The significance of values is indicated in Results as ** for P<0.001 and * for P<0.01.
The manufacturer of the Omron, in fact, does not provide fundamental information on whether the EE given is a total EE, including resting period, or whether it only concerns the added energy expenditure (AEE). The fact that Omron does not add any values when it does not detect any counts would also suggest that the EE levels provided are more probably equivalent to AEE, excluding the resting energy expenditure (REE). As an estimate of the resting component we chose the energy equivalent of consumption of O2 of 5 mL/kg/min as appropriate for calm standing.9 Subsequently, we added this estimate to the net EE values calculated by the Omron.
Results
Percentage deviations of devices from EE determined by IC with 95% limits of agreement and Pearson's correlation coefficients are expressed in Table 2. Mean deviations are also graphically expressed in Figure 1. We found considerable mean overestimation of both tested methods in level walking at the speed of 3 km/h (+70.51±20.91%, r=0.77** for Omron;+81.19±23.81%, r=0.79** for SWA) and at the speed of 4 km/h (+75.77±33.36%, r=0.52 for Omron; +78.18±33.96%, r=0.63* for SWA). At the level of high-intensity exercise at the speed of 5 km/h and 5% incline, an underestimation of both devices was found (−7.37±16.07%, r=0.75** for Omron; −7.88±16.86%, r=0.74** for SWA). The above-mentioned equation7 as a complementary method was in very good agreement with IC at the speed of 3 km/h (−0.68±11.5%, r=0.79**) but worse agreement at the speed of 4 km/h (+15.99±19.47%, r=0.64*). At the speed of 5 km/h and 5% incline, the deviation of the equation was+11.02±13.9% (r=0.88**). High correlation coefficients were found between Omron and the mathematical equation (r=0.95**, r=0.94**, and r=0.91** for Sessions 1–3, respectively). Correlation coefficients between SWA and this equation were always lower (r=0.76**, r=0.88*, and r=0.86** for Sessions 1–3, respectively).
Discussion
The current study deals with the accuracy of the Omron HJ-720 accelerometer and the SWA Pro 3 of measuring EE in individuals with diabetes during walking under controlled conditions. We expected different results in these patients than in the young healthy group because of worse anthropometric parameters and lower walking speeds tested. Although people with obesity, metabolic syndrome, and diabetes are instructed to focus on physical activity as part of their disease management, only a few specific validation studies of the Omron and SWA for basic walking have been done.10,11 In level walking, we found higher overestimation than other studies have reported. A problem we had to solve was that the manufacturer of the Omron device does not report whether the calculated EE value should correspond with the net EE or with the total EE including the resting component. This was also confirmed by Crouter et al.12 in their validation study, where in six out of eight movement sensors assessed, this information was not provided. Because no value is being added by the device in the calm position of the Omron as a resting component, we consider the calculated value is just as an AEE. For comparison with IC, we added to Omron values the estimation of an REE while standing (the energy equivalent of consumption of 5 mL/kg/min of O2). After this correction, the overestimation of the Omron was still lower than the overestimation of the SWA. Nevertheless, the deviation of calculated EE during level walking was relatively similar in both devices.
Related studies
Tierney et al.11 found an overestimation of EE by the SWA particularly in activities at intensity levels of 2–5 METs (walking, stair climbing, cleaning, dressing, washing, etc.). Unfortunately, their results are not expressed in percentages of reference values and not specifically for each activity. Papazoglou et al.10 tested a similar SenseWear® Armband Pro 2 device in 20 obese subjects during walking at speed of 3 km/h on a treadmill. In this study, the IC found the EE to be 5.8±0.66 kcal/min, and the SWA Pro 2 calculated the EE to be 7.62±2.0 kcal/min, giving an overestimation of about 32%. In this study, the mean body mass index of all participants was 44.5±6.2 kg/m2, and the weight was not reported. Our participants had a lower body mass index (31.5±3.6 kg/m2) and were probably lighter. In the previously mentioned study,10 the walking session took only 5 min, which we consider as too short. According to our experience, the actual EE in the first minutes of walking on a treadmill is often higher as the individual is getting used to the pace, which is detected only with IC. This could explain the lower calculated overestimation in comparison with our study, where the sessions were 15 min long.
The above should be taken into account when analyzing the study of Swartz et al.,13 which has tested the Omron HJ-720 in three subgroups (normal, overweight, and obese) during level walking at six speeds of 2.4–6.5 km/h in 5-min sessions. Values for specific groups and speeds are expressed only in graphs: the highest overestimation of EE in the normal group (about 55%) and the obese group (about 42%) was found at a speed of 3.6 km/h, whereas the overestimation in the overweight group (about 90%!) was found at a speed of 4 km/h. The most accurate values in normal and overweight group were at a speed of 6.4 km/h (deviation of almost 0%), which is close to the transition speed between walking and running14 and is associated with an energetically ineffective pace, which is recognized only by IC. In our opinion, this is why an underestimation (about 28%) was found at this highest speed in the group of obese individuals in the mentioned study.
The principle of calculation
Algorithms used for computing EE values are traditionally part of the trade secret and cannot be manipulated with. The principle most frequently used to convert data gathered by the sensors to EE values expressed in kilocalories is linear regression,15–17 as in the Omron. On the other hand, the manufacturer of the SWA states that based on the data of individual modalities, the instrument should be able to detect the basic physical activities such as walking, running, bicycling, weight lifting, or resting. The company also states that for each of these activities, a specific algorithm for EE computation is available. What we consider as a serious drawback, however, is that it is not possible to verify retrospectively whether the individual activities have indeed been correctly recognized by the SWA.
Like our previous study, which focused on a healthy population,18 the present study has demonstrated that neither the Omron nor the SWA is able to sufficiently detect appropriate EE in different inclines of the surface, providing an overestimation in level walking and underestimation in incline walking. This is in agreement with other types of accelerometric devices.19 A high overestimation (up to 70–80%) of EE for level walking is evident, whereas values for uphill walking were underestimated. This is contrary to other studies that tested the Omron devices. For instance, Giannakidou et al.20 found the EE was underestimated as calculated by Omron pedometers by as much as 28% in a speed-dependent manner. It must be noted, however, that their study was performed in younger population (22.6±2.8 years) with different anthropometric parameters (body mass index, 23.2±2.6 kg/m2), and the AEE estimation was not added.
So far, however, we have not been able to measure the agreement of EE levels for walking downhill. Both instruments seem to follow the same strategy, when in everyday use the overestimation of level walking EE should roughly offset the underestimation of uphill walking (which, however, is much lower). Another important fact is that, compared with walking on a treadmill, walking in real conditions is more energy-intensive, up to 20%, depending on the type of path.21
Relationship between speed and EE
Based on results of IC, in eight of the 19 subjects tested, EE during level walking at the speed of 3 km/h was—paradoxically—higher than at the speed of 4 km/h. These eight subjects were on average younger (age, 52.50±8.2 vs. 55.18±11.38 years) and weighed less (88.56±11.17 vs. 93.23±16.2 kg) than those subjects, whose EE was increasing with speed. The percentage of body fat (35.78±7.28% vs. 35.63±8.94%) and other anthropometric parameters were comparable. Also, this smaller group was subjectively more comfortable with the speed of 4 km/h than 3 km/h. This apparent contradiction may be explained by the fact that the dependence of EE on speed is not linear,22,23 and a certain U-shape curve rendering the dependence of EE on speed can be envisaged, where the present group of eight subjects in question would be situated somewhere on the concavity of this shape at the speed of 4 km/h. It may also depend on the fact that many of the participants had only little experience with the treadmill and that not even a trial stage before the testing itself was sufficient for them to get used to the movement, to keep balance and walk naturally. These subjective difficulties may in fact have helped increase EE in Session 1. On the other hand, it is in contradiction with the characteristics of these subjects because their anthropometric parameters were comparable to those of the other participants. Also, the mean age of the group was lower, which would suggest that they would need less time to get used to the treadmill.
When evaluating the Omron accelerometer during walking on a level surface (treadmill walking), we found out that this instrument is based on an almost linear correlation between the number of steps and EE. However, it is an established fact that this actual relation is not a purely linear one22,23 and that, especially at speeds over 6 km/h, EE increases much more quickly than what would correspond to a simple linear increase. In our opinion, this is the main reason why in the above-mentioned studies13,20 the highest underestimation was found at the highest tested speed of 6.4 km/h.
Better results in long-term studies
The argument found in numerous articles that the SWA is validated for medical purposes must be assessed with caution because different types of the device and/or different software version may have been used in the relevant studies. Johannsen et al.24 published a study based on an assessment of the SWA for 14 consecutive days with DLW as a reference. They used the same device (SWA) and firmware version (6.1) as we did, but their probands were lighter, younger, and healthier than ours. SWA showed a measuring error rate of 8.1±6.8% with r=0.80 (95% confidence interval, 0.89–0.70). The use of SWA for longer periods has also been tested in another study focused on older population, providing good agreement.25 Participants wore the device for 12.5 (±1.1) days, including during sleep. For the total EE, the DLW method provided 2,040±472 kcal/day versus 2,012±497 kcal/day by the SWA with an r correlation of 0.89 (P<0.001). Unfortunately, this study does not mention which version of SWA was used. Because of the relatively easy estimation of REE, the agreement with a reference method could be improved by long-term monitoring because of the long time spent without physical activity. In our earlier study18 focused on a young healthy population, the protocol consisted of nine 4-min walking sessions (different combinations of speed and incline) and eight 2-min break sessions. The total EE value for 52 min was 249.65±40.6 kcal estimated by IC and 220.86±28.56 kcal estimated by SWA.
Correlation with the mathematical equation
A high correlation of the Omron with the mathematical equation in level walking apparently results from the fact that both the Omron and the equation probably work with a similar formula for EE calculation, which might differ solely in the parameter of speed, because Omron obtains this parameter indirectly (length multiplied by number of steps). As for the lowest degree of correlation with IC, we found it in Session 2 (i.e., a moderate-intensity session) (for the equation, r=0.64, P<0.01; Omron+REE, r=0.52, P<0.05; SWA, r=0.63, P<0.01), which is not very encouraging because the speed of 4 km/h was found as the most comfortable by the majority of the subjects, and it may be assumed that in their habitual physical activity, they will choose to walk closer to this speed more frequently than to the other two.
Conclusions
We found considerable overestimation of EE for level walking, whereas there was a relatively minor underestimation for the 5% incline. This discrepancy applied not only to the SWA, but also to the Omron, which is one of the widely used accelerometers. These findings should be interpreted in the light of the fact that the instruments are unable to recognize uphill walking, which requires more energy. The overall overestimation of EE during walking calculated by the tested instruments can in real-life conditions partially compensate for the fact that walking on most surfaces is more energy-demanding than walking on a treadmill in the laboratory. As concerns actual overestimation/underestimation, the less sophisticated Omron showed a comparable, but smaller, error than the multimodal SWA device. In the case of the Omron, it remains to be ascertained whether the values it produces actually correspond to the AEE without the REE. Neither of the devices tested is suitable for accurate EE monitoring. They could, nevertheless, be used for indicative (motivational) assessment of the physical activity of patients with diabetes. In general, it would be less confusing to use the number of steps instead of calculated EE in the everyday physical activity control by these devices.
Acknowledgments
This study was conducted with the support of METABO project Controlling Chronic Diseases Related to Metabolic Disorders (ICT-2007-1-216270). The study was also supported by the university research grant SVV 2013-267603.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Physical activity/exercise and diabetes. Diabetes Care. 2004;27(Suppl 1):S58–S62. doi: 10.2337/diacare.27.2007.s58. [DOI] [PubMed] [Google Scholar]
- 2.Kramer PA. Sylvester AD. The energetic cost of walking: a comparison of predictive methods. PLoS One. 2011;6:e21290. doi: 10.1371/journal.pone.0021290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schoeller DA. Racette SB. A review of field techniques for the assessment of energy expenditure. J Nutr. 1990;120(Suppl 11):1492–1495. doi: 10.1093/jn/120.suppl_11.1492. [DOI] [PubMed] [Google Scholar]
- 4.Berntsen S. Hageberg R. Aandstad A. Mowinckel P. Anderssen SA. Carlsen KH. Andersen LB. Validity of physical activity monitors in adults participating in free-living activities. Br J Sports Med. 2010;44:657–664. doi: 10.1136/bjsm.2008.048868. [DOI] [PubMed] [Google Scholar]
- 5.Slabý K. Bohdanová M. Procházka M. Radvanský J. Pedometer accuracy: motor vehicle travel artifacts—preliminary results [in Czech] Med Sport Boh Slov. 2010;19:244–247. [Google Scholar]
- 6.Weir JB. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949;109:1–9. doi: 10.1113/jphysiol.1949.sp004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McArdle WD, editor; Katch IF, editor; Katch LV, editor. Exercise Physiology: Nutrition, Energy, Human Performance. Philadelphia: Lippincott Williams & Wilkins; 2009. [Google Scholar]
- 8.Bland JM. Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 9.Ainsworth BE. Haskell WL. Herrmann SD. Meckes N. Bassett DR., Jr Tudor-Locke C. Greer JL. Vezina J. Whitt-Glover MC. Leon AS. 2011 compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 10.Papazoglou D. Augello G. Tagliaferri M. Savia G. Marzullo P. Maltezos E. Liuzzi A. Evaluation of a multisensor armband in estimating energy expenditure in obese individuals. Obesity (Silver Spring) 2006;14:2217–2223. doi: 10.1038/oby.2006.260. [DOI] [PubMed] [Google Scholar]
- 11.Tierney M. Fraser A. Purtill H. Kennedy N. A study to determine the criterion validity of the Sensewear armband as a measure of physical activity in people with rheumatoid arthritis. Arthritis Care Res (Hoboken) 2012 Dec 4; doi: 10.1002/acr.21914. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Crouter SE. Schneider PL. Karabulut M. Bassett DR., Jr Validity of 10 electronic pedometers for measuring steps, distance, and energy cost. Med Sci Sports Exerc. 2003;35:1455–1460. doi: 10.1249/01.MSS.0000078932.61440.A2. [DOI] [PubMed] [Google Scholar]
- 13.Swartz AM. Strath SJ. Miller NE. Grimm EK. Ewalt LA. Loy MS. Gennuso KP. Validity of physical activity monitors in assessing energy expenditure in normal, overweight, and obese adults. Open Sports Sci J. 2009;2:58–64. doi: 10.2174/1875399X00902010058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Farinatti PT. Monteiro WD. Walk-run transition in young and older adults: with special reference to the cardio-respiratory responses. Eur J Appl Physiol. 2010;109:379–388. doi: 10.1007/s00421-010-1366-1. [DOI] [PubMed] [Google Scholar]
- 15.Freedson PS. Melanson E. Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30:777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 16.Hendelman D. Miller K. Baggett C. Debold E. Freedson P. Validity of accelerometry for the assessment of moderate intensity physical activity in the field. Med Sci Sports Exerc. 2000;32(9 Suppl):S442–S449. doi: 10.1097/00005768-200009001-00002. [DOI] [PubMed] [Google Scholar]
- 17.Welk GJ, editor. Champaign, IL: Human Kinetics; 2002. Physical Activity Assessments for Health-Related Research. [Google Scholar]
- 18.Machač S. Monitoring of energy expenditure with the SenseWear Armband™ [in Czech] Med Sport Boh Slov. 2011;20:131–138. [Google Scholar]
- 19.Jakicic JM. Winters C. Lagally K. Ho J. Robertson RJ. Wing RR. The accuracy of the TriTrac-R3D accelerometer to estimate energy expenditure. Med Sci Sports Exerc. 1999;31:747–754. doi: 10.1097/00005768-199905000-00020. [DOI] [PubMed] [Google Scholar]
- 20.Giannakidou DM. Kambas A. Ageloussis N. Fatouros I. Christoforidis C. Venetsanou F. Douroudos I. Taxildaris K. The validity of two Omron pedometers during treadmill walking is speed dependent. Eur J Appl Physiol. 2012;112:49–57. doi: 10.1007/s00421-011-1951-y. [DOI] [PubMed] [Google Scholar]
- 21.Givoni B. Goldman RF. Predicting metabolic energy cost. J Appl Physiol. 1971;30:429–433. doi: 10.1152/jappl.1971.30.3.429. [DOI] [PubMed] [Google Scholar]
- 22.Atzler E. Herbst R. Arbeitsphysiologische Studien. Arch Ges Physiol. 1927:291–328. [Google Scholar]
- 23.Margaria R. Sulla fisiologia e specialmente sul consumo energetico della marcia e della corsa a varie velocità ed inclinazioni del terreno. Atti Accad Lincei Memorie. 1938:7299–368. [Google Scholar]
- 24.Johannsen DL. Calabro MA. Stewart J. Franke W. Rood JC. Welk GJ. Accuracy of armband monitors for measuring daily energy expenditure in healthy adults. Med Sci Sports Exerc. 2010;42:2134–2140. doi: 10.1249/MSS.0b013e3181e0b3ff. [DOI] [PubMed] [Google Scholar]
- 25.Mackey DC. Manini TM. Schoeller DA. Koster A. Glynn NW. Goodpaster BH. Satterfield S. Newman AB. Harris TB. Cummings SR. Validation of an armband to measure daily energy expenditure in older adults. J Gerontol A Biol Sci Med Sci. 2011;66:1108–1113. doi: 10.1093/gerona/glr101. [DOI] [PMC free article] [PubMed] [Google Scholar]