Abstract
With advancement in technology, improvement in endoscope and ancillary equipment, more complex procedures can be performed using flexible ureterorenoscopy. In this review article we provide a summary of flexible ureterorenoscopic procedures with “tips and tricks” for success for each type of procedure. It looks at the disposables used with flexible ureterorenoscopic procedures, set up and patient positioning for gaining access, insertion and handling of scope and the use of urethral access sheath. We also provide techniques for various flexible ureterorenoscopic procedures including management of renal stones, calyceal diverticula and upper tract urothelial tumours.
Keywords: Calculi, flexible ureterorenoscopy, holmium laser, lithotripsy, laser vaporization
INTRODUCTION
The fibreoptic technology used in modern medicine was first demonstrated 150 years ago by John Tyndall in 1854. Young and McKay described the first ureteroscopy in 1929.[1] These Ureteroscopes were without any active deflection or working channel and were for diagnostic use only. It was not until 1978 before the first distal ureteroscopy was reported by Lyon and colleagues.[1,2] In association with Karl Storz, the first working Ureteroscope was developed in 1980 by Perez-Castro, a rigid ureteroscope with a separate optic and working channel. This was soon followed by the first electrohydraulic and ultrasonic lithotripsy a year later. The same year ureteroscopy and stone basketing under direct vision was reported by Das. The first flexible tip ureteroscope was introduced by Bagley and colleagues in 1983.[1,2]
Last two decades have witnessed a huge improvement in flexible ureterorenoscope (F-URS) technology with smaller outer diameter, larger working channel, active deflection and better fibre optics.[2,3] With digital imaging and high definition television, the image quality has improved and the digital chip is now incorporated in the tip of the newer F-URS. In addition to the improvements in the endoscope, ancillary equipment such as graspers, baskets and laser technology have also progressed allowing more complex procedures. As the technology has improved, there has been a huge surge in the number of ureterorenoscopic procedures being performed.[4] The indications for F-URS procedures include management of calculus disease, diagnostic procedures, endoscopic management of upper tract tumors and endoureterotomy or endopyelotomy.[5–9] The aim of this paper is to provide a summary of flexible ureterorenoscopic procedures with “tips and tricks” for success for each type of procedure.
Disposables used with the flexible ureterorenoscopic (F-URS) procedure
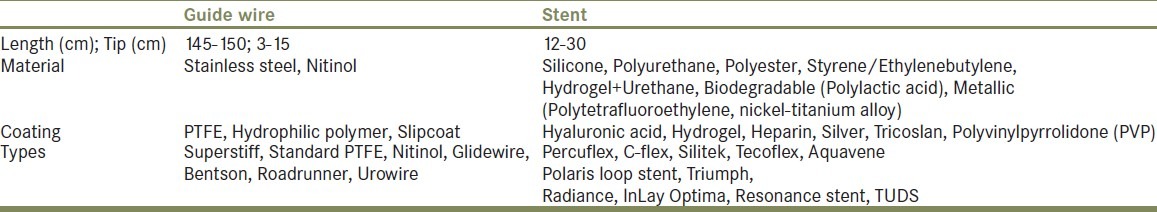
Guide wires
Guide wires are used to gain access to renal collecting system and to allow passage of stents and catheters. The three important characteristics are tip flexibility, low friction and shaft rigidity, the later more useful as a coaxial system for passage of catheters or stents. Two 150-cm-long and 0.035 or 0.038 inch diameter guide wires (one ‘safety’ and one ‘working’ wire) should be used. The distal tip end must be flexible and atraumatic and its length varies from 3 to 15 cm [Table 1]. To reduce friction, guide wires are coated with polytetrafluroethylene (PTFE) or hydrophilic polymer. The latter is useful for negotiating difficult ureter; however these hydrophilic wires must be kept moist prior to its use. The working wire should be hydrophilic to protect the working channel of the scope. For difficult guide wire passage the following tricks can be helpful – advancing it via ureteral catheter, using a hydrophilic guide wire or Ureteroscopically passing it under vision and treating the underlying pathology such as stone fragmentation or balloon dilatation of stricture to allow access.[10] Difficult ureteral access can be negotiated (at times) with a 0.025 or 0.028 hydrophilic wire. Occasionally, for impacted ureteral stones direct disintegration is the only way to avoid false passage by guide wire, whatever the type or material of guide wire used. If a glide wire is used, once it is passed proximal to the stone, a 5Fr open ended catheter can be passed and the wire exchanged for a stiff wire.
Table 1.
Examples of material, coating and types of guide wires and stents available
Ureteral catheter
A 5-6F open tip ureteral catheter is used for retrograde pyelogram (RPG) or for positioning the guide wire in the ureter or to obtain urine sample from pelvicalyceal system for cytology/culture.
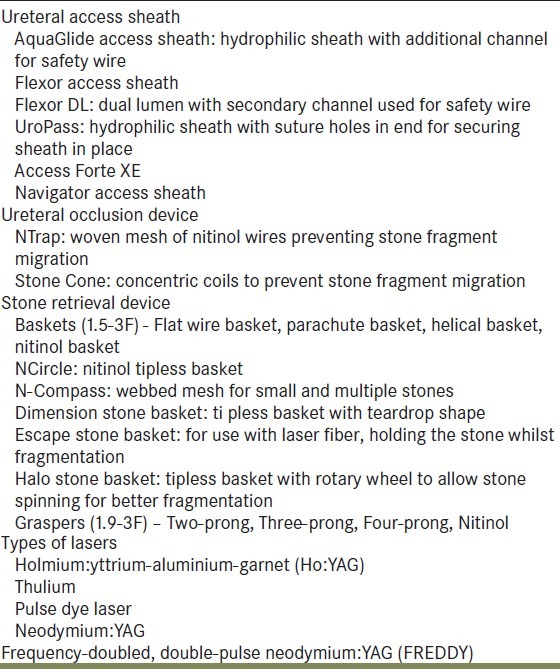
Ureteral access sheath
With expanding indication of F-URS, the use of access sheath is now becoming more common. It can facilitate ureterorenoscopy and retrieval of stone fragments (multiple withdrawals and reinsertions), whilst reducing the intrarenal pressure, improving irrigant flow, better visibility, decreasing operative time and costs.[11,12]
The access sheath is a 2-piece hydrophilic device: the sheath and the internal dilator [Table 2]. It is inserted over the working wire under fluoroscopic control and the internal dilator can be removed once the sheath is in place. Care should be taken while inserting it and forceful insertion should be avoided. It comes in various diameters (9.5-14 F internal diameter and 11.5-17.5 F external diameter) and lengths (20-55 cm).[13]
Table 2.
Different accessories used with flexible ureteroscopic procedures
Port seal
The seal is fixed on the working channel of the F-URS. The seal consists of an O-ring which allows the operator to conserve irrigant and preserve leaks whilst gripping the instrument (such as laser fiber).
Stone extraction devices
The extraction devices include stone-graspers, baskets and forceps [Table 2]. Most modern devices are made of nitinol, which have memory, resist kinking and cause minimal loss of deflection. To minimize complications it is important to carefully select the extraction device for the size and location of the stone, having a safety wire at all times, maintaining a good view at all times and avoiding forceful or blind manipulation. All extraction devices should be introduced in a straight scope (undeflected).
Baskets – Nitinol baskets are now standard device for stone retrieval.[2,13] The range from 1.5-2.2F and are flexible, designed not to damage the scope or intra-renal system. The smallest possible basket for the purpose should be used. Basket opening and closing are controlled by a proximal handle.
Graspers – These have 3 or 4 prongs that allow the impacted stone (in renal papilla or urothelial mucosa) to be extracted. They are also effective in removing stone from the kidney with the main advantage of being able to release the stone at any time.
Biopsy forceps – Allows taking biopsy sample from tumors or urothelial mucosa.
Irrigation
Saline is the standard irrigation used for F-URS. To improve the irrigant flow with an instrument in the working channel, it can be pressurized to get adequate flow at the distal tip of the ureteroscope. This can be done either by a manual pressure pump or pressure irrigation bag or a mechanical irrigator.[14,15]
Ureteral drainage
At the end of the procedure ureteral drainage may be required. This is done by leaving a ureteral catheter for up to 24 hours or a double J stent for several days. Stents are placed to prevent or relieve intrinsic or extrinsic ureteral obstruction. Various etiologies include ureteric calculi or stricture, retroperitoneal disease, trauma or iatrogenic injury and drainage post urinary diversion. A guide wire is positioned fluoroscopically or endoscopically prior to stenting. Care should be taken whilst cannulating the ureteric orifice so that it is atraumatic without creating a false passage, avoiding over distension and coiling of guide wire in the bladder. While the stent is being placed, the guide wire should be held taut and the stent position checked fluoroscopically and cystoscopically.
There is a wide variation in the size, shape and material of ureteric stents [Table 1]. The first generation polymeric stents were made of silicone which has now been replaced by polyurethane and newer polymers. To reduce bacterial adherence, biofilm formation and encrustation the newer stents are either made of modified polyurethane or other such polymers and some of them have additional coating. The coatings are either antibacterial agents (hydrogel, silver, PVP, heparin) or they are surface property enhancers (hyaluronic acid, heparin).[16]
Laser
Various different types of laser fibers have been used for ureteroscopic procedures [Table 2]. The Holmium-YAG laser is now the gold standard for use with the F-URS and delivers pulsatile energy.[2] It allows intra-corporeal lithotripsy, management of ureteral strictures and urothelial tumors.[2,17] The laser fiber must be placed right against the target (stone or tumor) for it to work. They can be single use or reusable and come in different sizes. The smaller diameter fiber (150-200 μm) deliver less energy but allow scope deflection, whilst the larger diameter fiber (350-400 μm) restrict scope deflection giving more power. There is a red aiming beam (green in some lasers) which shows where the fiber is in relation to the target.
Set-up and patient positioning and gaining access
Flexible ureteroscopy is usually performed under general anesthesia. Ensure that a urinalysis has been done preoperatively to rule out a urinary tract infection. Prophylactic antibiotics should be administered as per protocol. The patient is typically in dorsal lithotomy position.
Ensure that pressure points are protected. Fluoroscopy should be available and radiation symbol should be placed outside operating theatre. A cystoscopy is then performed to assess the position and size of ureteric orifice and to help insert a guide wire into the renal pelvis under fluoroscopic guidance. A RPG is then performed via a ureteric access catheter under fluoroscopy to visualize the ureteric and intra-renal anatomy and/or pathology. For all ureteroscopic procedures a ‘safety wire’, which provides access to the renal pelvis should be placed and kept secure at all times.[12,13,15] In males, the penis is held straight to straighten the urethra. Under fluoroscopy, F-URS (or the access sheath if it is being used) is then passed over a second ‘working’ wire.
Insertion, holding and handling of flexible ureterorenoscope
The handle of the ureterorenoscope is always held with dominant hand with the deflection control worked with the thumb, whilst the non-dominant hand controls the advancement/withdrawal of the scope. The scope should be kept straight without any distal tip deflection and inserted into the intra-renal collecting system over the working guide wire.[15] The working wire is then withdrawn and cold-light cable, the camera and irrigation system is attached. Recently wireless ureteroscopy has been described, but this is not standard practice and may be operator skill dependent.[15]
Ureteral dilatation and insertion of ureteral access sheath
After cystoscopy a safety guide wire is placed. Routine ureteric dilatation is not necessary.
For ureteral dilatation a ureteral balloon catheter is inserted over the working guide wire under fluoroscopic control.[13] Ureteral dilatation is then performed with inflation of balloon with contrast agent.
Ureteral access sheath is inserted over the working guide wire under fluoroscopic guidance.
The appropriate sheath based on its diameter and length should be selected on the anticipated use and ureteric anatomy.[13,15]
Management of kidney stones (other than lower-pole calculi)
Several options are available for managing kidney stones including percutaneous nephrolithotomy (PCNL), shock wave lithotripsy (SWL) and flexible ureteroscopy and lasertripsy (FURSL). We describe FURSL for managing renal stones. After the ‘safety wire’ and UAS is placed and secured, the F-URS is inserted over the working guide wire. Once the scope is in the pelvis, the working guide wire is withdrawn. The intra-renal collecting system is explored and the stone is located. The laser fiber (200 or 365 μm) is introduced into the working channel of the F-URS.[18] The fiber is advanced a few millimeters beyond the end of the working channel, the aiming beam is switched on and the laser is ready. The initial laser settings are of a frequency of 5-10 Hz and the power of 1-1.5 J (corresponding to 5-9 W).[19] The fiber is placed against the stone and fragmentation is commenced. Once fragmented, the fragments are captured with a grasper and withdrawn with the scope. If a UAS is not being used, the ureteroscope is withdrawn and must be repositioned over a working guide wire. If the fragment will not go through the UAS, the ureteroscope should be grasped against the distal end of the sheath and the entire unit (scope, grasper holding the stone and the access sheath) is removed in ‘one piece’, provided the fragment can be accommodated by the ureter. At the end of the procedure, the intra-renal system is re-inspected for any fragments. If the ureter needs to be drained, a ureteric catheter or an internal stent may be left in place, overnight or for a few days respectively.
Management of lower-pole calculi
Once the F-URS is in place, the lower pole calculus is located. A nitinol basket (1.5-2.4F) is inserted and the stone is captured and displaced to the upper pole calyx or renal pelvis. The stone is released and laser fiber is used to fragment the stone. If the stone cannot be displaced from lower pole calyx, it is fragmented in situ using a smaller laser fiber (150-200 μm).[5,20] For the introduction of the laser fiber, the scope must always be kept straight (undeflected) and scope deflection is only started after the fiber is at the tip of the endoscope.[21] The fragments are removed, the intra-renal system is re-inspected and ureter drained as described above.
Prevention of stone fragment accumulation in the lower calyx
If at the end of flexible ureterorenoscopy and lasertripsy (FURSL), many small stone fragments are left in the collecting system, there will be a risk of these fragments re-accumulating in the lower-pole calices. To prevent this, the lower pole calices can be sealed with an autologous blood clot. The ureteroscope is positioned in the lower group of calices.
Saline is then injected into the working channel of the scope, to flush the fragments towards the upper calices and the renal pelvis, and to clear any remaining contrast. Through the working channel of the scope, 5-10 ml of autologous blood (taken from peripheral venous line) is then injected.[22] The scope position in the lower caliceal group needs to be checked under fluoroscopy as the blood completely obscures the endoscopic vision. Once injected, the scope is withdrawn, and the surgeon waits 5-10 minutes for blood seal to form. RPG is then performed to check that the lower calyx is no longer visualized ensuring that the clot is providing a seal.
Management of calyceal diverticula
The decision to perform F-URS versus PCNL can be very difficult and the choice depends on the position, size and length of calyceal infundibulum. We describe the management of calyceal diverticula using F-URS. The F-URS is introduced into the intra-renal collecting system, as described above. A mixture of contrast and methylene blue or indigo carmine is injected through the working channel of the scope. Opacification of the diverticulum under fluoroscopy means that the neck of the diverticulum is patent.[23]
Saline is used to flush the intra-renal collecting system. The diverticulum is then observed for leakage of dye, with a delayed emptying of the diverticulum suggesting a narrow neck. A laser fiber (350-400 μm) is then passed through the working channel of the scope to incise the neck of the diverticulum. The scope is then inserted into the diverticulum and the stone can either be fragmented in situ or extracted intact with nitinol grasper.[24] Following treatment of the stone(s), the neck of the diverticulum is then generously incised with the laser, to allow the diverticulum to be marsupialised into the collecting system. A check for any residual fragments is made and a ureteral drainage with an internal stent is done with the pigtail of the stent in the marsupialised cavity (if possible).
Retrograde endopyelotomy
A RPG is performed and Uretero-pelvic junction (UPJ) obstruction is confirmed.[9] The extrinsic obstructing cause should be identified if the obstruction is from outside. A safety wire is secured and if required a short UAS is inserted under fluoroscopy. The F-URS is then inserted over the working guide wire. The position of the scope is then checked whether it is in the renal pelvis (if the UPJ is passable) or distal to UPJ (if it is not passable). The working wire is withdrawn and with the ureteroscope kept straight (distal tip undeflected), a 365 μm laser fiber is advanced a few millimeters beyond the end of the working channel. With the aiming beam switched on the laser is set at a frequency of 12-15 Hz and a power of 1-1.5J (15-22 W).[19] If the scope is in the renal pelvis the UPJ is incised as the scope is being withdrawn towards the ureter, where as if the scope is below the UPJ the incision is made as the scope is being advanced towards the renal pelvis. Repeated passes are then made with the laser fiber, until the preiureteral fat appears. The F-URS is removed and a high-pressure ureteral balloon catheter is inserted over the safety wire. Under fluoroscopic guidance, the balloon is inflated with contrast agent to dilate the incised area.[6] The ureteral balloon catheter is removed and a RPG is performed, which would show extravasation of contrast for a correctly performed endopyelotomy. At the end of the procedure, a ureteral stent (8F or 12/8F) should be inserted and left in place for 4-6 weeks with a urethral catheter for 24 hours.
Retrograde endoureterotomy
A RPG is performed and the ureteric stricture identified. A safety wire is secured and if required and safe, a short UAS is inserted under fluoroscopy. The F-URS is then inserted over the working guide wire. The position of scope is checked, whether it is in the renal pelvis (ureteric stricture is passable) or distal to the stricture (not passable). The laser endoureterotomy is then done in the same was as retrograde endopyelotomy. Balloon dilatation is then done with contrast agent to dilate the incised area. For a correctly done endoureterotomy, a subsequent RPG will show extravasation of contrast from the ureter. An internal stent (12F) should be inserted and left in place for 6 weeks with a urethral catheter for 24 hours.
Antegrade flexible ureteroscopy
Although not frequently indicated, it can be useful in difficult retrograde access or in cases of urinary diversion.[25] Antegrade F-URS places mechanical stress on the scope and weakens it. In a prone position, the intra-renal collecting system is punctured under ultrasound or fluoroscopic guidance. A middle or upper calyceal system should be preferred as it helps scope alignment with the ureter. Contrast is injected through the puncture needle, to opacify the intra-renal collecting system and the ureter. The working guide wire is then inserted into the ureter under fluoroscopic guidance. The puncture needle is withdrawn and a dual-lumen catheter is inserted over the working guide wire. The safety guide-wire is then inserted through the second channel of the dual lumen catheter and is secured to the patient's body. Dual-lumen catheter is withdrawn and a high-pressure ureteral balloon catheter is inserted over the working guide wire. Under fluoroscopy, the balloon is inflated with contrast to dilate the tract. The ureteric balloon catheter is then withdrawn and UAS is inserted over the working guide wire. The F-URS is then inserted through the UAS over the working guide wire under fluoroscopic guidance. The working wire is removed and antegrade ureterorenoscopic procedure is carried out as indicated. At the end of the procedure the UAS is removed and a percutaneous nephrostomy tube is inserted under fluoroscopic guidance and secured to skin.
Management of urothelial tumors
Standard treatment of ureteric or renal pelvic tumors is nephroureterectomy. However, for patients with solitary kidney, chronic renal insufficiency or bilateral disease endoscopic management is an alternative option. Once the F-URS is in position, a saline wash of the intra-renal system may be obtained for cytology.[8,26] A RPG may be indicated to assist in localization of the lesion. However, it must not be done prior to cytological sampling as it interferes with the cytopathological examination. Trauma to the urothelium by advancement of guide wire should be avoided as it may cause mucosal trauma and can be confused as a lesion. Once the tumor is localized the choice of ablation techniques includes – 1) Debulking of tumor by cold-cutting it with a tipless nitinol basket for pathology, followed by laser vaporization of tumor base, or 2) Biopsy with forceps and vaporizing the entire tumor with a laser.[10,27] Vaporization is done with holmium: YAG laser (365 μm) with a frequency of 10Hz and a power of 1-1.2J (10-12 W).[19] For lower pole lesions, a smaller diameter fiber (200 μm) is used. Once the lesion is treated, inspect the rest of the intra-renal and ureteric surface. At the end, drainage is established either by a ureteral catheter left for 24 hours or a ureteric stent left for a few days. Adjuvant chemotherapy with instillation of topical agents may be given as appropriate.
Durability of the scope
With broadening indications of F-URS and high cost of purchase and maintenance, durability of scopes is extremely important.[28] The problems arise from loss of tip deflection, perforation of inner lining of the scope and loss of fibreoptic bundles. The newer generation of scopes seem to require fewer repairs especially in experienced hands.[29] The most common damage is to the working channel. This is done by working devices, especially laser fibers with the distal tip of F-URS deflected or if the laser is fired within the scope.[30] Hence, the damage can be avoided by keeping the scope straight before inserting the laser fiber and ensuring that it is not fired within the scope. Damage has also been reported during handling and sterilization of the scopes and hence adequate training to staff should be provided to minimize this.[31]
CONCLUSIONS
Flexible ureteroscopy with Holmium-YAG laser is an effective, reproducible and minimally traumatic diagnostic and therapeutic technique perfectly adapted to disease of the upper urinary tract. With digital technology, the new F-URS provide better image quality and hence, greater precision for diagnostic and therapeutic procedures. Time and technology will continue to help with ‘miniaturization’ of the scope. Improvement in optics and ancillary equipment will allow access and treatment in all cases even those with anomalous or reconstructed urinary tract anatomy.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Johnston WK, 3rd, Low RK, Das S. The evolution and progress of ureteroscopy. Urol Clin North Am. 2004;31:5–13. doi: 10.1016/S0094-0143(03)00100-9. [DOI] [PubMed] [Google Scholar]
- 2.Beiko DT, Denstedt JD. Advances in ureterorenoscopy. Urol Clin North Am. 2007;34:397–408. doi: 10.1016/j.ucl.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Monga M, Anderson KJ, Durfee W. Physical properties of flexible ureteroscopes: implications for clinical practice. J Endourol. 2004;18:462–5. doi: 10.1089/0892779041271454. [DOI] [PubMed] [Google Scholar]
- 4.Bratslavsky G, Moran ME. Current trends in ureteroscopy. Urol Clin North Am. 2004;31:181–7. doi: 10.1016/S0094-0143(03)00096-X. xi. [DOI] [PubMed] [Google Scholar]
- 5.Grasso M, Ficazzola M. Retrograde ureteropyeloscopy for lower pole caliceal calculi. J Urol. 1999;162:1904–8. doi: 10.1016/S0022-5347(05)68065-2. [DOI] [PubMed] [Google Scholar]
- 6.Razdan S, Silberstein IK, Bagley DH. Ureteroscopic endoureterotomy. BJU int. 2005;95(Suppl 2):94–101. doi: 10.1111/j.1464-410X.2005.05207.x. [DOI] [PubMed] [Google Scholar]
- 7.Traxer O. Flexible ureterorenoscopic management of lower-pole stone: Does the scope make the difference? J Endourol. 2008;22:1847–50. doi: 10.1089/end.2008.9792. discussion 1855. [DOI] [PubMed] [Google Scholar]
- 8.Grasso M, Fraiman M, Levine M. Ureteropyeloscopic diagnosis and treatment of upper urinary tract urothelial malignancies. Urology. 1999;54:240–6. doi: 10.1016/s0090-4295(99)00121-1. [DOI] [PubMed] [Google Scholar]
- 9.Conlin MJ, Bagley DH. Ureteroscopic endopyelotomy at a single setting. J Urol. 1998;159:727–31. [PubMed] [Google Scholar]
- 10.Lam JS, Gupta M. Ureteroscopic management of upper tract transitional cell carcinoma. Urol Clin North Am. 2004;31:115–28. doi: 10.1016/S0094-0143(03)00099-5. [DOI] [PubMed] [Google Scholar]
- 11.Auge BK, Pietrow PK, Lallas CD, Raj GV, Santa-Cruz RW, Preminger GM. Ureteral access sheath provides protection against elevated renal pressures during routine flexible ureteroscopic stone manipulation. J Endourol. 2004;18:33–6. doi: 10.1089/089277904322836631. [DOI] [PubMed] [Google Scholar]
- 12.Monga M, Bodie J, Ercole B. Is there a role for small-diameter ureteral access sheaths? Impact on irrigant flow and intrapelvic pressures. Urology. 2004;64:439–41. doi: 10.1016/j.urology.2004.04.060. discussion 441-2. [DOI] [PubMed] [Google Scholar]
- 13.Holden T, Pedro RN, Hendlin K, Durfee W, Monga M. Evidence-based instrumentation for flexible ureteroscopy: A review. J Endourol. 2008;22:1423–6. doi: 10.1089/end.2007.0327. [DOI] [PubMed] [Google Scholar]
- 14.Parkin J, Keeley FX, Jr, Timoney AG. Flexible ureteroscopes: A user's guide. BJU Int. 2002;90:640–3. doi: 10.1046/j.1464-410x.2002.03017.x. [DOI] [PubMed] [Google Scholar]
- 15.Sprunger JK, Herrell SD., 3rd Techniques of ureteroscopy. Urol Clin North Am. 2004;31:61–9. doi: 10.1016/S0094-0143(03)00093-4. [DOI] [PubMed] [Google Scholar]
- 16.Molimard B, Al-Qahtani S, Lakmichi A, Sejiny M, Gil-Diez de Medina S, Carpentier X, et al. Flexible ureterorenoscopy with Holmium laser in horseshoe kidneys. Urology. 2010;76:1334–7. doi: 10.1016/j.urology.2010.02.072. [DOI] [PubMed] [Google Scholar]
- 17.Stilling NM, Jung H, Nørby B, Osther SS, Osther PJ. Retrograde ureteroscopic holmium laser endopyelotomy in a selected population of patients with ureteropelvic junction obstruction. Scand J Urol Nephrol. 2009;43:68–72. doi: 10.1080/00365590802473164. [DOI] [PubMed] [Google Scholar]
- 18.Breda A, Ogunyemi O, Leppert JT, Schulam PG. Flexible ureteroscopy and laser lithotripsy for multiple unilateral intra-renal stones. Eur Urol. 2009;55:1190–6. doi: 10.1016/j.eururo.2008.06.019. [DOI] [PubMed] [Google Scholar]
- 19.Traxer O, Lechevallier E, Saussine C. Flexible ureteroscopy with Holmium laser: Technical aspects. Prog Urol. 2008;18:929–37. doi: 10.1016/j.purol.2008.09.034. [DOI] [PubMed] [Google Scholar]
- 20.Auge BK, Dahm P, Wu NZ, Preminger GM. Ureteroscopic management of lower-pole renal calculi: technique of calculus displacement. J Endourol. 2001;15:835–8. doi: 10.1089/089277901753205852. [DOI] [PubMed] [Google Scholar]
- 21.Monga M, Dretler SP, Landman J, Slaton JW, Conradie MC, Clayman RV. Maximizing ureteroscope deflection: “play it straight”. Urology. 2002;60:902–5. doi: 10.1016/s0090-4295(02)01891-5. [DOI] [PubMed] [Google Scholar]
- 22.Traxer O, Dubosq F, Chambade D, Sèbe P, Sylvestre S, Haab F, et al. How to avoid accumulation of stone fragments in the lower calix during flexible ureterorenoscopy. Prog Urol. 2005;15:540–3. [PubMed] [Google Scholar]
- 23.Traxer O, Sèbe P, Chambade D, Sylvestre S, Haab F, Gattegno B, et al. How to identify the neck of a caliceal diverticulum in flexible ureterorenoscopy. Prog Urol. 2005;15:100–2. [PubMed] [Google Scholar]
- 24.Sejiny M, Al-Qahtani S, Elhaous A, Molimard B, Traxer O. Efficacy of flexible ureterorenoscopy with holmium laser in the management of stone-bearing caliceal diverticula. J Endourol. 2010;24:961–7. doi: 10.1089/end.2009.0437. [DOI] [PubMed] [Google Scholar]
- 25.el-Nahas AR, Eraky I, el-Assmy AM, Shoma AM, el-Kenawy MR, Abdel-Latif M, et al. Percutaneous treatment of large upper tract stones after urinary diversion. Urology. 2006;68:500–4. doi: 10.1016/j.urology.2006.03.065. [DOI] [PubMed] [Google Scholar]
- 26.Chen GL, El-Gabry EA, Bagley DH. Surveillance of upper urinary tract transitional cell carcinoma: The role of ureteroscopy, retrograde pyelography, cytology and urinalysis. J Urol. 2000;164:1901–4. doi: 10.1016/s0022-5347(05)66913-3. [DOI] [PubMed] [Google Scholar]
- 27.Cornu JN, Rouprêt M, Carpentier X, Geavlete B, de Medina SG, Cussenot O, et al. Oncologic control obtained after exclusive flexible ureteroscopic management of upper urinary tract urothelial cell carcinoma. World J Urol. 2010;28:151–6. doi: 10.1007/s00345-009-0494-x. [DOI] [PubMed] [Google Scholar]
- 28.Pasqui F, Dubosq F, Tchala K, Tligui M, Gattegno B, Thibault P, et al. Impact on active scope deflection and irrigation flow of all endoscopic working tools during flexible ureteroscopy. Eur Urol. 2004;45:58–64. doi: 10.1016/j.eururo.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 29.Traxer O, Dubosq F, Jamali K, Gattegno B, Thibault P, et al. New-generation flexible ureterorenoscopes are more durable than previous ones. Urology. 2006;68:276–9. doi: 10.1016/j.urology.2006.02.043. discussion 280-1. [DOI] [PubMed] [Google Scholar]
- 30.Carey RI, Gomez CS, Maurici G, Lynne CM, Leveillee RJ, Bird VG. Frequency of ureteroscope damage seen at a tertiary care center. J Urol. 2006;176:607–10. doi: 10.1016/j.juro.2006.03.059. discussion 610. [DOI] [PubMed] [Google Scholar]
- 31.Sooriakumaran P, Kaba R, Andrews HO, et al. Evaluation of the mechanisms of damage to flexible ureteroscopes and suggestions for ureteroscope preservation. Asian J Androl. 2005;7:433–8. doi: 10.1111/j.1745-7262.2005.00077.x. [DOI] [PubMed] [Google Scholar]


