Abstract
The testicular plasmocytoma represents only 5% of the non-germinative cell testicular tumors, and accounts for only 2% of all plasma cell neoplasms. Approximately, 50 cases of testicular plasmocytoma have been reported in medical literature; however, only 9 of these are isolated tumors without previous history or progression to multiple myeloma. A 47-year-old patient, presenting progressive and painless growth of the right testicle in the last four years, underwent surgical treatment in another hospital two years ago, to correct a hydrocele in the same testicle with no improvement at all. Sonography showed a tumor with the following measurements for the right testicle: 84 × 59 × 80 mm. The tumor marker values were all normal. An abdominal computed tomography found no evidence of retroperitoneal lymph nodes invasion. The patient underwent a right radical orchiectomy. Pathologic analysis revealed a malignant neoplasia described as a plasmocytoma (solitary myeloma) that produces immunoglobulin's kappa light chain. After five years of follow-up, there were no signs of metastasis or local recurrence in the exams. Case report and review of literature have been presented here.
Keywords: Plasmocytoma, solitary myeloma, testicle
INTRODUCTION
The plasmocytoma is a plasma cell tumor with low rate of growth and its most common location is the bone. When this tumor occurs in others tissues, it is called as extra-medullary plasmocytoma and is considered a rare disorder. The upper air-way (nasal cavity, nasopharynx, paranasal sinuses and larynx) accounts for 90% of the extra-medullary plasmocytomas. Less common sites are the gastrointestinal tract, central nervous system, bladder, thyroid, breast, parotid glands and lymph nodes.[1] The testicular plasmocytoma represents only 5% of the non-germinative cell testicular tumors, and accounts for only 2% of all plasma cell neoplasms. It is usually an autopsy finding causing no clinical signs; however, may sometimes is seen as a manifestation of a multiple myeloma and, more exceptionally, the testicle may be its only location.[2] Approximately 50 cases of testicular plasmocytoma have been reported in medical literature, however only 9 of these were isolated tumors without any previous history or progression to multiple myeloma.[3]
The diagnosis of this tumor is based on histologic confirmation of monoclonal plasma cell infiltration of a single disease site and on the exclusion of systemic myeloma. The treatment of these tumors may be done with surgery, or radiotherapy associated or not associated with chemotherapy. The orchiectomy is the preferred treatment in cases of testicular tumors.[1] Using radiotherapy with a total dose of at least 4000 cGy, the risk for local recurrence is less than 5%.[4]
CASE REPORT
A 47-year-old patient, presenting with progressive and painless growth of the right testicle in the last four years, underwent surgical treatment in other hospital two years before to correct a hydrocele in the same testicle with no improvement. Sonography revealed a solid heterogeneous tumor in the right testicle with the following measurements: 84 × 59 × 80 mm (still with residual hydrocele). The tumor markers (alpha-fetoprotein, beta-Human chorionic gonadotropin [HCG] and lactate dehydrogenase [LDH]) values were all normal. An abdominal computed tomography found no evidence of retroperitoneal lymphnodes invasion. The patient underwent a right radical orchiectomy then [Figure 1]. Pathologic analysis revealed a malignant neoplasia described as a plasmocytoma (solitary myeloma) that produces immunoglobulin's kappa light chain [Figure 2]. After the surgery, the patient recovered well. After five years of follow-up there were no signs of metastasis or local recurrence in the examination.
Figure 1.
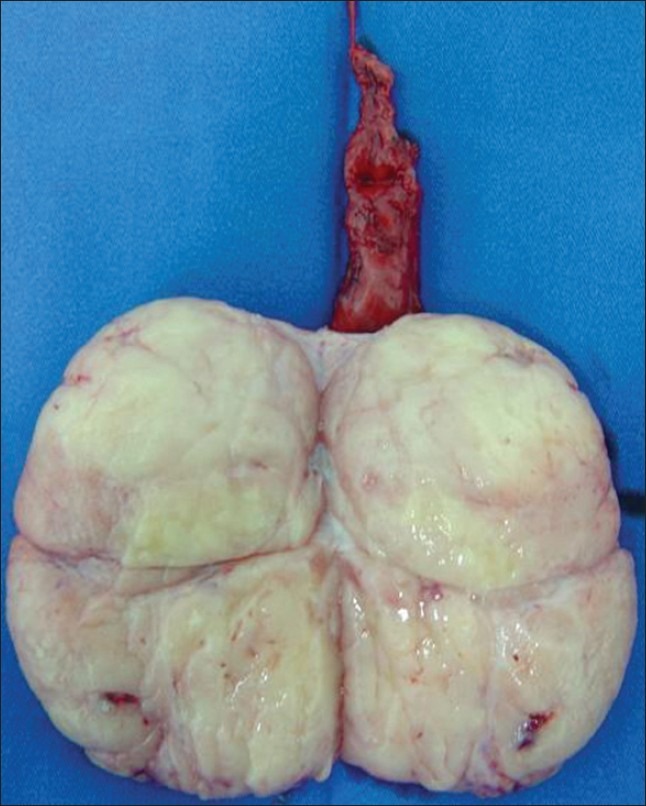
Testicle aspect after orchiectomy of the patient in the case report
Figure 2.
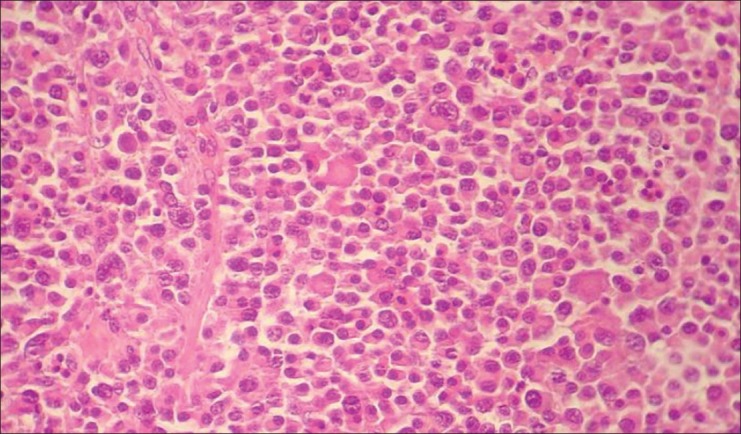
Microscopic aspect of the tumor of the patient in the case report
DISCUSSION
The main concern about the testicular plasmocytoma is that its low rate of growth makes it different from other testicular tumors and may delay its diagnosis by confusing its presentation with other benign diseases, and sometimes is even associated with them.[5] Although in other sites of extra-medullary plasmocytomas, the fine-needle aspiration or the biopsy could be considered as helpful procedures to establish preoperative diagnosis, it is considered unsafe to do so in the testicular masses due to the risk of tumor dissemination to the scrotum.[1]
The pathological diagnosis of plasmocytoma is also a challenge, and only microscopic examination could not be enough. Confirmation of the diagnosis is facilitated by ancillary studies. Plasmocytomas show positive immunostaining for CD138, CD79a and monoclonal antibody VS38, and monotypic cytoplasmic immunoglobulin staining. Light chain restriction in tumor cells can also be confirmed by in situ hybridization. Lesions that are sometimes difficult to distinguish from testicular plasmocytoma include seminoma (classic and spermatocytic), lymphoma and metastatic melanoma.[6]
Cytogenetic studies of plasmocytomas show recurrent losses in chromosome 13, chromosome arm 1p and chromosome arm 14q as well as gains in chromosome arms 19p, 9q and 1q.[6] The monomer deletion or escalation of chromosome 13 is found in 15% to 48% of the patients.[7]
Even though the most accepted treatment for extra-medullary plamocytomas is the radiotherapy,[1,4] orchiectomy was the chosen treatment in almost all case reports of testicular tumors probably due to lack of previous diagnosis suspicion. Only one author reports the use of radiotherapy to treat a testicular plasmocytoma with a good local outcome, but with a systemic recurrence after chemotherapy.[8]
The presented case is unique in literature due to its time of follow-up. The longest follow-up in case reports is 14 months.[9] This lack of long term follow-up creates doubt about the progression of the tumor to multiple myeloma, since the plasmocytomas are considered by some as an initial presentation of a multiple myeloma instead of an isolated tumor.[10]
Approximately 30% of patients with solitary bone plasmocytoma remain disease-free for several years; and, some of these patients may be cured. The prognosis of patients with solitary extra-medullary plasmocytoma appears to be better than for patients with solitary bone plasmocytoma, because approximately 70% of patients with solitary extra-medullary plasmocytoma remain disease-free at 10 years.[4]
Another concern about the plasmocytoma is the use of adjuvant therapy, which is also a controversy among authors. Favorable outcome of patients with testicular plasmocytoma that underwent surgical treatment suggests that there is no need for complementary treatment in these cases, however close follow-up to help in early detection of eventual progression to multiple myeloma must be kept.
Adjuvant chemotherapy should be considered in patients with tumors greater than five centimeters and those with high-grade tumors.[1]
This particular natural behavior presented by the testicular plasmocytoma may lead to a diagnostic challenge, because the clinical differential diagnosis with other benign diseases in not precise and other malignancies cannot be safely excluded without pathological examination. Surgical treatment is the treatment of choice in almost all cases thanks to the doubt in diagnosis, thus overcoming radiotherapy as the main option of treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Soutar R, Lucraft H, Jackson G, Reece A, Bird J, Low E, et al. Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma. Clin Oncol (R Coll Radiol) 2004;16:405–13. doi: 10.1016/j.clon.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 2.Alvarez-Mugica M, Monzon Jalon A, Vazquez Bulnes V, Andrea Aguilar C, Gomez Fernandez JM, Alvarez Gonzalez RC, et al. Secondary testicular plasmocytoma. Arch Esp Urol. 2007;60:99–102. [PubMed] [Google Scholar]
- 3.Chelly I, Mekni A, Bellil K, Salah Belhadj M, Bellil S, Haouet S, et al. Testicular plasmocytoma: A case report. Tunis Med. 2007;85:702–3. [PubMed] [Google Scholar]
- 4.Dimopoulos MA, Hamilos G. Solitary bone plasmacytoma and extramedullary plasmacytoma. Curr Treat Options Oncol. 2002;3:255–9. doi: 10.1007/s11864-002-0015-2. [DOI] [PubMed] [Google Scholar]
- 5.Suzuki K, Shioji Y, Morita T, Tokue A. Primary testicular plasmacytoma with hydrocele of the testis. Int J Urol. 2001;8:139–40. doi: 10.1046/j.1442-2042.2001.00269.x. [DOI] [PubMed] [Google Scholar]
- 6.Tanagho Y, Stovsky M, Maclennan GT. Testicular plasmacytoma. J Urol. 2010;184:1161–2. doi: 10.1016/j.juro.2010.06.031. [DOI] [PubMed] [Google Scholar]
- 7.Wang YM, Li FY, Luo JD, Li J, Xie LP, Yang GS. Testicular plasmacytoma: A case report and review of the literature. Chin Med J (Engl) 2008;121:956–8. [PubMed] [Google Scholar]
- 8.Pisoni Brambilla G, Assi A, Ballarati E, Turri E, Zaroli A, Montalbetti L, et al. Plasmocytoma of the testis. Description of a clinical case and review of the literature. Minerva Med. 1993;84:211–5. [PubMed] [Google Scholar]
- 9.Iizumi T, Shinohara S, Amemiya H, Tomomasa H, Yazaki T, Umeda T, et al. Plasmacytoma of the testis. Urol Int. 1995;55:218–21. doi: 10.1159/000282791. [DOI] [PubMed] [Google Scholar]
- 10.Pham TH, Shetty SD, Stone CH, De Peralta-Venturina M, Menon M. Bilateral synchronous testicular plasmacytoma. J Urol. 2000;164:781. doi: 10.1097/00005392-200009010-00042. [DOI] [PubMed] [Google Scholar]


