Abstract
We describe a case-report of a chylous ascites after laparoscopic donor nephrectomy, summarize the current literature, and hypothesize on the etiology of this complication.
Keywords: Chylous ascites, hand-assisted, laparoscopic donor nephrectomy
INTRODUCTION
Living donor kidney transplantation is the treatment of choice for end-stage renal failure. Recipients of living donor kidneys have increased graft survival as compared with deceased donor kidneys. Laparoscopic hand-assisted donor nephrectomy (HALDN) is a procedure with low morbidity and mortality. Chylous ascites after donor nephrectomy is a rare complication. In this report, we present a case and we discuss the current literature and focus on the etiology of this complication.
CASE REPORT
A 34-year-old woman was subjected to an HALDN of the left kidney. The dissection and sealing of all tissues around the kidney and the renal hilar vessels were performed with the Ethicon® Ultracision harmonic scalpel. There were no intraoperative complications. The postoperative course of the donor was uneventful; she was discharged after 5 days. After one week, she presented with complaints of abdominal bloating and constipation. Physical examination showed a distended abdomen. An ultrasound revealed a significant amount of free fluid. Ultrasound-guided paracentesis aspirated a significant amount of creamy pink fluid. Laboratory tests of the fluid showed a creatinine of 69 μmol/l (the unit μmol/l is correct), triglyceride of 45.85 mmol/l, and 4.0 × 109 leucocytes and it was considered as chyle. A paracentesis drain was left in the abdomen. A total of 4.5 l chyle was aspirated by paracentesis. Patient was treated with octreotide three times, 0.1 mg a day subcutaneously, and was placed on medium-chain triglycerides (MCT) diet. The symptoms improved quickly and the drain was removed after 2 days. After 6 days, patient was discharged and maintained on an MCT diet for 6 weeks. There was no reoccurrence of the ascites. A repeated ultrasound showed absence of abdominal free fluid.
DISCUSSION
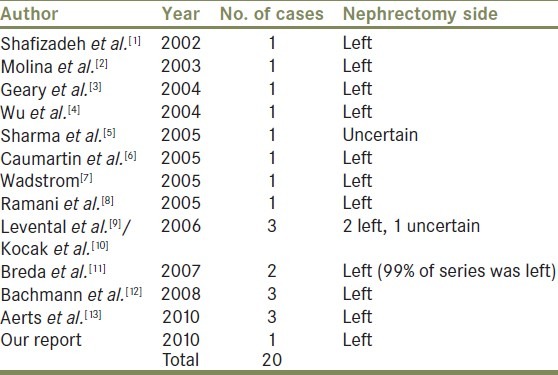
The cause of postoperative chylous ascites is leakage from damaged lymph vessels in the operative field. Lymph vessels do not contract and thrombose following interruption as blood vessels do. Leakage from transected lymph vessels is frequently identified during operations, especially abdominal aortic surgery. Abdominal aortic surgery is the most important cause of postoperative chylous ascites. Chylous ascites after laparoscopic donor nephrectomy is a rare complication. Previous reports are summarized in Table 1. To our knowledge, 20 cases have been reported in literature so far.
Table 1.
Reports on chylous ascites after laparoscopic donor nephrectomy
Kocak et al.[10] reported in their series 600 open and laparoscopic donor nephrectomies in which three chylous ascites (0.5%) occurred. In the first 500 donor nephrectomies (99% left-sided donor nephrectomies) of this series, two cases of chylous ascites occurred. Since they assumed that insufficient sealing during the procedure was the cause of this complication, they started to routinely use a fibrin sealant additional to the Ethicon® Ultracision device to seal the vessels. In the following 100 cases, they found another case of chylous ascites.
We report on our first and only case of chylous ascites following HALDN in our center. Between January 2000 and March 2011, we performed 198 left-sided and 171 right-sided HALDNs. All our procedures were performed with the use of the Ethicon® Ultracision without the use of fibrin sealing. In this series, only a single case of chylous ascites occurred.
It is remarkable that the majority of the reported cases of chylous ascites occurred after a left-sided laparoscopic donor nephrectomy. Does the local anatomy of the lymphatics surrounding the left kidney have a role in the cause of the chylous ascites or are there more left kidneys procured for living donor transplantation as compared with right donor kidneys? Some centers have a preference for the left kidney and others for the right kidney.
The paralumbar lymphatic trunks are the major lymphatic trunks in the retroperitoneum and transport the lymph from the lower limbs, genitalia, and pelvic organs. Proximally, the paralumbar trunks are joined with the intestinal trunk and form the cisterna chyli. The lymph vessels and lymph major trunks are concentrated along the para-aortic region. The length and the position of the left kidney make it necessary to perform a dissection close to the aorta to gain sufficient length of renal artery for the implantation procedure. In case of the right kidney, the renal artery is dissected right laterocaudal to the inferior caval vein. So, a para-aortal dissection is not performed during a right-sided donor nephrectomy. This anatomical difference in perioperative surgical strategy could be the reason why all chylous ascites complications are described after left-sided laparoscopic donor nephrectomies.
We did not find any report in the literature of chylous ascites after open donor nephrectomy. It might be that this complication is even more rare after open donor nephrectomy. In open aortic surgery, leakage from lymph vessels is frequently identified and subsequently selectively ligated or sealed during the operation. The pneumoperitoneum which is necessary for the laparoscopic donor nephrectomy and the presence of a high pressure state can in theory mask leakage from the low-pressure lymph vessels.
In conclusion, chylous ascites is a rare complication after laparoscopic donor nephrectomy. Due to anatomic and surgical technical aspects, it could possibly be a specific complication of the left-sided donor nephrectomy.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Shafizadeh SF, Daily PP, Baliga P, Rogers J, Baillie GM, Rajagopolan PR, et al. Chylous ascites secondary to laparoscopic donor nephrectomy. Urology. 2002;60:345xvi–345xix. doi: 10.1016/s0090-4295(02)01743-0. [DOI] [PubMed] [Google Scholar]
- 2.Molina W, Desai M, Gill I. Laparoscopic management of chylous ascites after donor nephrectomy. J Urol. 2003;170:1938. doi: 10.1097/01.ju.0000091660.15018.66. [DOI] [PubMed] [Google Scholar]
- 3.Geary B, Wade B, Wollmann W, El-Galley R. Laparoscopic repair of chylous ascites. J Urol. 2004;171:1231–2. doi: 10.1097/01.ju.0000110104.68489.70. [DOI] [PubMed] [Google Scholar]
- 4.Wu CT, Chiang YJ, Liu KL, Chu SH. Laparoscopic donor nephrectomy: New combination of hand-assisted and standard approaches. Transplant Proc. 2004;36:1909–11. doi: 10.1016/j.transproceed.2004.08.096. [DOI] [PubMed] [Google Scholar]
- 5.Sharma A, Heer M, Malladi S, Minz M. Chylous ascites after laparoscopic donor nephrectomy. J Endourol. 2005;19:839–40. doi: 10.1089/end.2005.19.839. [DOI] [PubMed] [Google Scholar]
- 6.Caumartin Y, Pouliot F, Sabbagh R, Dujardin T. Chylous ascites as a complication of laparoscopic donor nephrectomy. Transpl Int. 2005;18:1378–81. doi: 10.1111/j.1432-2277.2005.00219.x. [DOI] [PubMed] [Google Scholar]
- 7.Wadström J. Hand-assisted retroperitoneoscopic live donor nephrectomy: Experience from the first 75 consecutive cases. Transplantation. 2005;80:1060–6. doi: 10.1097/01.tp.0000176477.81591.6f. [DOI] [PubMed] [Google Scholar]
- 8.Ramani AP, Gill IS, Steinberg AP, Abreu SC, Kilciler M, Kaouk J, et al. Impact of intraoperative heparin on laparoscopic donor nephrectomy. J Urol. 2005;174:226–8. doi: 10.1097/01.ju.0000162048.15746.52. [DOI] [PubMed] [Google Scholar]
- 9.Leventhal JR, Kocak B, Salvalaggio PR, Koffron AJ, Baker TB, Kaufman DB, et al. Laparoscopic donor nephrectomy 1997 to 2003: lessons learned with 500 cases at a single institution. Surgery. 2004;136:881–90. doi: 10.1016/j.surg.2004.06.025. [DOI] [PubMed] [Google Scholar]
- 10.Kocak B, Koffron AJ, Baker TB, Salvalaggio PR, Kaufman DB, Fryer JP, et al. Proposed classification of complications after live donor nephrectomy. Urology. 2006;67:927–31. doi: 10.1016/j.urology.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 11.Breda A, Veale J, Liao J, Schulam P. Complications of laparoscopic living donor nephrectomy and their management: The UCLA experience. Urology. 2007;69:49–52. doi: 10.1016/j.urology.2006.09.030. [DOI] [PubMed] [Google Scholar]
- 12.Bachmann A, Wyler S, Wolff T, Gürke L, Steiger J, Kettelhack C, et al. Complications of retroperitoneoscopic living donor nephrectomy: Single center experience after 164 cases. World J Urol. 2008;26:549–54. doi: 10.1007/s00345-008-0296-6. [DOI] [PubMed] [Google Scholar]
- 13.Aerts J, Matas A, Sutherland D, Kandaswamy R. Chylous ascites requiring surgical intervention after donor nephrectomy: Case series and single center experience. Am J Transplant. 2010;10:124–8. doi: 10.1111/j.1600-6143.2009.02883.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


