Abstract
Eosinophilic cystitis (EC) is a rare disease. It is a transmural inflammation of the bladder, predominantly with eosinophils. High index of suspicion is needed for timely intervention. EC should be kept as a differential diagnosis in patients presenting with lower urinary tract symptoms due to small capacity bladder with a negative workup for urinary tuberculosis and in patients having hematuria and negative cytology, or incidentally found bladder lesions with known risk factors. Initial treatment is conservative with removal of risk factor, anti-histaminics and steroids. Augmentation cystoplasty should be considered in patients with a small capacity bladder. These patients need a strict and long term follow-up.
Keywords: Anti-histaminic, augmentation cystoplasty, eosinophilic cystitis, genitourinary tuberculosis, lower urinary tract symptoms, steroids
INTRODUCTION
First described by Edwin Brown in 1960, eosinophilic cystitis (EC) is a rare inflammatory bladder pathology and is still a pathological surprise.[1] It is a transmural inflammation of the bladder, predominantly with eosinophils, along with fibrosis of the bladder wall, with or without muscle necrosis. It has myriad presentations and remains a diagnostic dilemma. High index of suspicion is needed for timely intervention.
Eosinophilic cystitis is reported in patients of all age groups. It is equally distributed among both sexes in adults with a male preponderance in children.[2] The etiology of EC is unclear. Though it has been associated with allergy, asthma, atopy, peripheral eosinophilia, bladder trauma, open bladder surgery, transurethral resection of the bladder tumor, intravesical mitomycin-C, thiotepa, Bacillus-Calmette-Guerin (BCG), drugs (e.g., tranilast, sulfonamides, warfarin and penicillin), parasitic infections, eosinophilic enteritis, recurrent urinary tract infection, vesicoureteric reflux, ovarian teratoma, chronic granulomatous disease, sutures and food stuff, such as tomatoes, coffee and carrots, only a few of these associations have been verified so far.[3]
The immunological factors associated with EC have been postulated to be IgE mediated formation of antigen-antibody complexes which attracts eosinophils to the bladder wall. This leads to degranulation of mast cells and activation of eosinophils causing significant tissue damage and inflammation.[4] The manifestation of EC varies widely from mild bladder involvement, leading to some combination of storage and voiding lower urinary tract symptoms, hematuria and suprapubic pain with erythematous bladder lesions simulating interstitial cystitis or carcinoma in situ, to serious, painful, hemorrhagic and tumor like processes simulating infiltrative cancer with intractable upper urinary tract obstruction.
Urinalysis in EC commonly shows proteinuria and microscopic hematuria. Urine cultures are usually sterile.[2] Eosinophiluria is rarely seen and is not peculiar to EC.[3] Peripheral eosinophilia, defined as more than 5% of the total differential leukocyte count or 500 eosinophils per mm3 is seen in 50% of the patients. Imaging may be normal or may show irregular bladder wall thickening and tumor-like masses. In the later stages, the bladder may be small and contracted, and there may be resultant hydronephrosis.[3]
Cystoscopy shows erythematous, polypoid velvety red lesions and gross mucosal edema.[5] EC is primarily managed conservatively. In patients of EC with documented allergic reactions or use of agents like tranilast or mitomycin-C, removal of the causative factor can be curative. In idiopathic EC, non-steroidal anti-inflammatory drugs (NSAID) and anti-histamines have been used. Other treatments reported include intravesical dimethylsulfoxide, cyclosporin-A, silver nitrate and montelukast sodium. Transurethral resection of the bladder lesion has shown excellent outcome. Few patients with progressive EC not responding to medical therapy or transurethral resection may be considered for more radical procedures, such as partial/total cystectomy or augmentation cystoplasty.[6,7] We present here our institute's experience with eosinophilic cystitis.
CASE REPORT
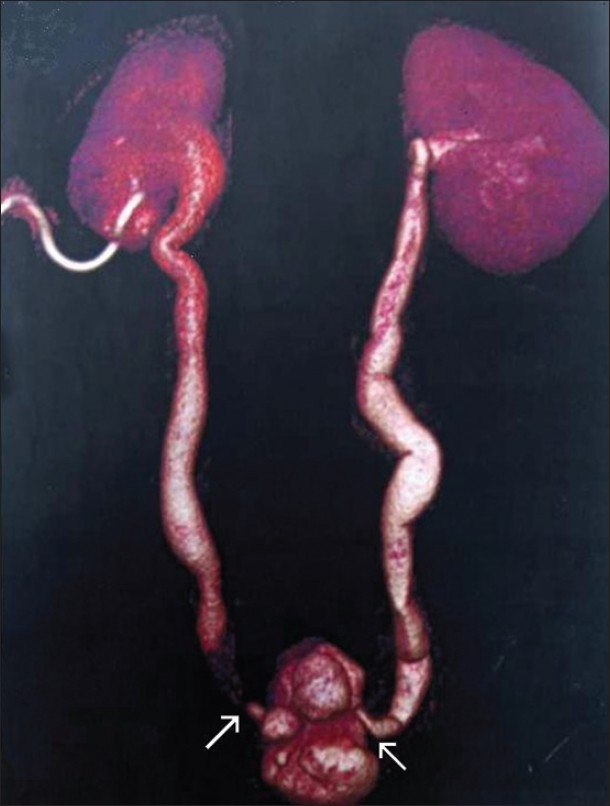
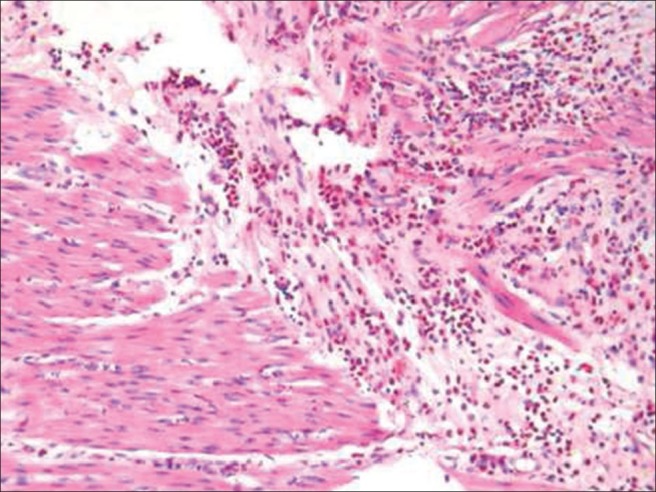
Clinical, radiological and pathological data of five patients diagnosed to have EC in our institute from July 2005 to December 2010 were retrieved and analyzed. There were four male patients and one female patient with age ranging from 40 to 80 years. Two of these patients presented with lower urinary tract symptoms and three were incidentally diagnosed but had underlying predisposing factors. The patient demographics, management and clinical outcome are given in Table 1. Our first patient was a 40-year-old male who had history of hematuria and severe frequency of urination for three years. He had been evaluated in an outside hospital. Though acid-fast bacilli smear, culture and Mycobacterium tuberculosis-polymerase chain reaction of urine had been negative, he had been started on anti-tubecular therapy (ATT) empirically based on clinical and radiological parameters. Since he did not have any benefit after completion of ATT, he was referred to our institute. His computerised tomography (CT) urography showed bilateral hydroureteronephrosis with narrowing at bilateral vesico-ureteric junctions with a small capacity bladder [Figure 1]. He underwent supratrigonal cystectomy with ileo-ceco-cystoplasty and bilateral ureteric reimplantation. Intraoperatively, there was a thick walled, small capacity urinary badder with inflamed and friable mucosa. Histopathology revealed eosinophilic cystitis showing transmural dense eosinophilic infiltrate and no evidence of tuberculosis [Figure 2]. At three years follow up, patient was doing well and voiding satisfactorily.
Table 1.
Demographics, treatment and clinical outcome of the patients in the case study report
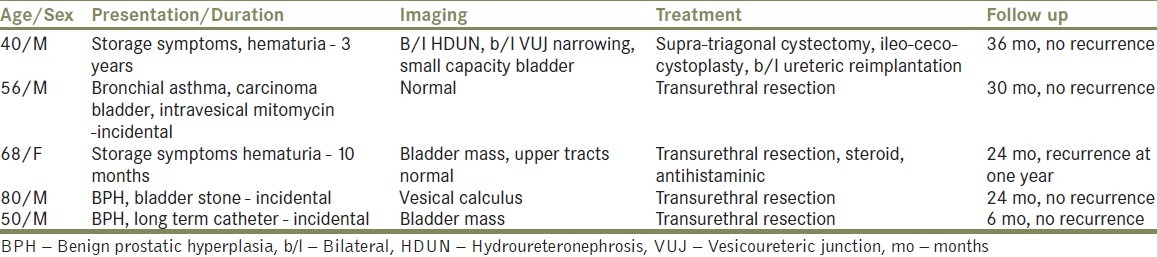
Figure 1.
Reconstructed computerised tomography urography image showing small contracted irregular bladder with bilateral hydroureteronephrosis and right percutaneous nephrostomy in situ. White arrows indicate the bilateral vesico-ureteric junction strictures
Figure 2.
Hematoxylin and eosin stain, ×280 microphotograph showing dense eosinophilic infiltration of the detrusor muscle and no evidence of tuberculosis in the case 1 of the series
The second patient was a 56 year- old- male, an asthmatic and a known case of superficial carcinoma urinary bladder. He had received weekly intravesical mitomycin-C therapy. At follow-up cystoscopy, he was found to have velvety lesions in urinary bladder which was resected transurethrally. Histopathology showed EC. This patient had peripheral eosinophilia also. He has been on regular cystoscopic follow-up for 2.5 years with no recurrence so far. The third patient was a 68 year-old-female with irritative voiding symptoms and hematuria. On cystoscopy, she was found to have a velvety lesion on posterior bladder wall which was resected and the histopathology revealed EC. This patient had peripheral eosinophilia. Patient was kept under follow up and had a similar lesion at the same site at one year which was resected and found to be EC. Patient was treated with steroids and anti-histaminics, and at one year follow-up there was no recurrence. The fourth patient was an 80 year-old-male, who had benign prostatic hyperplasia (BPH) with bladder stone. He was incidentally diagnosed to have a small supratrigonal lesion during trans-urethral resection of prostate. Biopsy of the resected specimen confirmed EC. Patient was free of recurrence at two years follow-up. The last patient was a 50 year-old-male with BPH on indwelling catheter, incidentally detected to have a two cm diameter bladder lesion on ultrasonography which was resected subsequently. Histopathology was reported as EC. He was free of recurrence at six months' follow up.
DISCUSSION
Eosinophilic cystitis is a rare condition. In our series, four patients had one of the predisposing factors mentioned previously. One of our patients had a presentation which typically mimicked features of urinary tuberculosis. Though peripheral eosinophilia is commonly reported, only one of our patients had peripheral eosinophilia. Sidh et al. reported a case of severe haematuria in EC needing salvage cystectomy.[8] In view of the variable natural history of the condition, chronicity and risk of recurrence, patients with EC need long-term follow-up with relevant blood tests, urine examination, appropriate imaging and cystoscopy.[8]
EC presenting as contracted small bladder is still rarer with only two cases reported so far.[6,7] There are no specific imaging and clinical features suggestive of EC, and it is very difficult to distinguish it from urinary tuberculosis. Our patient was initially managed with complete course of anti-tubercular therapy, but there was no clinical or radiological benefit, and subsequently he underwent augmentation ileo-cystoplasty which has been reported as surgical treatment of choice in such patients.[7] All patients with suspected urinary tuberculosis should undergo bladder biopsy if they are not responding to empirical anti-tubercular therapy. All the patients having initiated on anti-tubercular therapy should be followed up vigorously to avoid developing preventable complications.
In a patient presenting with lower urinary tract symptoms due to small bladder and features of urinary tuberculosis with negative workup, in patients having hematuria and negative cytology or incidentally found bladder lesions with known risk factors, EC should be suspected as a differential diagnosis. Most of the patients can be managed conservatively with removal of risk factor, anti-histaminics and steroids. Transurethral resection should be done in a patient presenting as bladder mass to rule out underlying malignancy. Augmentation cystoplasty is the solution when the patient has developed small capacity bladder. These patients need a strict and long term follow-up as recurrences are common and may mimic myriad bladder pathologies.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Brown EW. Eosinophilic granuloma of the bladder. J Urol. 1960;83:665–8. doi: 10.1016/S0022-5347(17)65773-2. [DOI] [PubMed] [Google Scholar]
- 2.Van den Ouden D. Diagnosis and management of eosinophilic cystitis: A pooled analysis of 135 cases. Eur Urol. 2000;37:386–94. doi: 10.1159/000020183. [DOI] [PubMed] [Google Scholar]
- 3.Itano NM, Malek RS. Eosinophilic cystitis in adults. J Urol. 2001;165:805–7. [PubMed] [Google Scholar]
- 4.Rubin L, Pincus MB. Eosinophilic cystitis: The relationship of allergy in the urinary tract toeosinophilic cystitis and the pathophysiology of eosinophilia. J Urol. 1974;112:457–60. doi: 10.1016/s0022-5347(17)59761-x. [DOI] [PubMed] [Google Scholar]
- 5.Cohen SM, Johansson SL. Lower Urinary tract. In: Damjanov I, Linder J, editors. Anderson's Pathology. 10th ed. St. Louis: Mosby; 1996. pp. 2150–1. [Google Scholar]
- 6.Cardini S, Smulewich E, Salvadori A, Lombardi M. Augmentation ileocystoplasty in a case of eosinophilic cystitis. Minerva Urol Nephrol. 1997;49:219–23. [PubMed] [Google Scholar]
- 7.Kayigil O, Ozbagi T, Cakar S, Metin A. Contracted bladder secondary to eosinophilic cystitis. Intl Urol Nephrol. 2001;33:341–2. doi: 10.1023/a:1015201410322. [DOI] [PubMed] [Google Scholar]
- 8.Teegavarapu PS, Sahai A, Chandra A, Dasgupta P, Khan MS. Eosinophilic cystitis and its management. Int J Clin Pract. 2005;59:356–60. doi: 10.1111/j.1742-1241.2004.00421.x. [DOI] [PubMed] [Google Scholar]


