Sir,
In recent years the use and the overuse of antibiotics to treat Upper Respiratory Tract Infections (URTIs) has resulted in the development of resistance patterns across widespread areas. Most URTIs are self-limiting viral infections due to rhinovirus, para-influenza virus, corona virus and adenovirus and resolve without prescription drugs. There is sufficient evidence to support the viral origin of most of these illnesses. However, even some of the bacterial illnesses are also self-limiting and antibiotic treatment is unnecessary. Acute bacterial sinusitis develops in 0.5-2% of cases of viral URTI. Recognizing viral or bacterial diseases (for which specific therapy is available) is important. Therapy addressing specific symptoms is the mainstay for most URTIs (viral). Antibiotics have no role in the management of common cold or any mild URTI except when it is due to bacterial infections like streptococcal pharyngitis, bacterial sinusitis, epiglottitis, pertussis or diphtheria.[1]
Resistance to antibiotics is a matter of great importance. Availability of antibiotics without prescription in our country has, by facilitating the development of resistance, already limited the therapeutic options in the treatment of life threatening infections and it needs to be discouraged. There is increasing evidence that directly associates antibiotic use with the emergence of resistant bacteria such as methicillin-resistant staphylococcus aurous (MRSA), vancomycin resistant enterococcus, resistant gram negative bacilli and clostridium difficile.[2]
The present study was conducted to study the non-prescription and irrational usage of antibiotics for URTI in the urban population. The study was conducted retrospectively in a north Indian city in 200 patients visiting a dental clinic, who could provide information about the medicines used, in the previous episodes of URTI. The data was collected on a questionnaire performed by the investigator, by interviewing the patients on antibiotic usage in URTI on a non-prescription basis, for a recall period of six months. Data on the source of information for the patient about the drug, awareness about the cost difference of generic or branded drugs, dose and duration of the drug for which it was taken and any adverse effect experienced with its use, were also collected.
The number of patients who had consumed antibiotics for URTI was 93 (46%). Out of which only 15 (7%) had taken prescription from the physician. Rest all were over the counter (OTC) purchases. Out of which 24 (12%) had taken the drug for relief from cold and 54 (27%) had taken antibiotics for cough and fever.
The most commonly used antibiotics included amoxicillin and co-amoxiclav (36%), roxithromycin (21%), azithromycin (16%), ciprofloxacin (12%), cefixime (9%) and levofloxacin (6%) [Figure 1]. Only 42 patients (21%) completed the full course of antibiotic treatment. 36 (18%) patients stopped taking them on getting relief from the symptoms and rest after experiencing diarrhoea as a side effect. The chemistۥs advice was the most common source of information, taken by patients for the OTC purchase of antibiotics (48%), followed by previous experience. Other sources of information were the relatives and the internet. Most (90%) of the drugs purchased were branded drugs, rest were generic.
Figure 1.
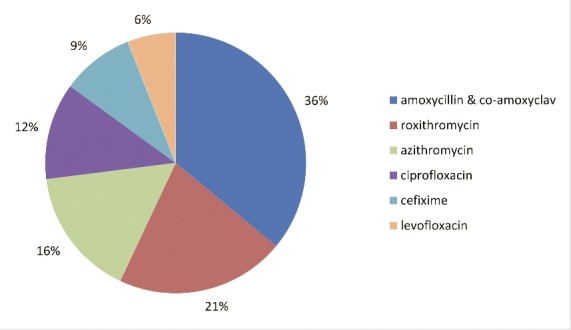
Chart showing non-prescription use of individual antibiotics for upper respiratory tract infections
The data shows a gross over-usage of non-prescription antibiotics, that too not taken for a full course, by most of the patients of URTI. Taking the drugs for inadequate duration worsens the scenario even more. The study shows the lack of awareness in the patients about the fact that it could increase the drug resistance problem. The study showed that awareness about the branded drugs being costlier than the generic drugs was also not there.
Most of the URTIs are self-limiting viral infections, not requiring the use of antibiotics. Patients need to take rest, adequate amount of fluids, antipyretic drugs and symptomatic treatment for cough and cold to recover from viral URTI.[1] Literature shows that nasal symptoms improve after treatment with α –adrenergic agonists and anti- histamines. Warm saline gargles and steam inhalation are inexpensive and relatively safe measures that provide temporary relief of throat symptoms. Non-steroidal anti-inflammatory drugs are useful for relieving fever, headache and malaise.[1]
The wide-spread use of antibiotics and that too broad spectrum ones results in emergence of many multi-resistant bacteria.[2,3] In order to preserve the activity of currently available antibiotics for as long as possible, care should be taken about the judicious use of these only in serious infections or the ones that are likely to respond significantly to treatment. The more judicious use of antibiotics can reduce resistance.[4]
Guidelines recommend that patients must visit the prescriber if there are symptoms indicating middle ear infection or acute bacterial sinusitis. These may be nasal discharge, hyposmia or anosmia, fever, cough, fatigue, maxillary dental pain, ear pressure or fullness. Antibiotics use by the physician should be reserved for moderate symptoms, not improving after 10 days or worsening after 5-7 days.[5,6]
This study highlights about the ignorance of even urban, educated patients about the problems associated with misuse of antibiotics. So, advice regarding judicious and rational use of antibiotics must be given by the healthcare professionals, whenever patient approaches them for some reason or through patient information brochures and newsletters.
Patients should be educated about the existence of bacterial and viral infections and also that the antibiotics would be of no use in a viral illness. The fact that these drugs could become ineffective, even for a bacterial infection, if misused or over-used, must be conveyed to them. Patient education can help in reducing the drug resistance problem to a great extent. Drug regulatory authorities must also take adequate steps to curb the OTC availability of antibiotics and empirical use of broad spectrum antibiotics should be curbed in URTIs in the larger interest of the patients.
REFERENCES
- 1.Dowell SF, Schwartz B, Phillips WR. the Pediatric URI Consensus Team. Appropriate use of antibiotics for URTIs in children. Part II. Cough pharyngitis and common cold. Am Fam Physician. 1998;58:1335–42,1345. [PubMed] [Google Scholar]
- 2.Nasrin D, Collignon PS, Roberts L, Wilson E, Pilotto LS, Douglas RM. Effect of beta-lactam antibiotic use in children on pneumococcal resistance to penicillin: Prospective cohort study. BMJ. 2002;324:28–30. doi: 10.1136/bmj.324.7328.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Angela C, Rafael P, Angela BB, Abdel E, Anthony H, Richard MW, et al. Effect of antibiotic prescribing on antibiotic resistance in individual children in primary care: Prospective cohort study. BMJ. 2007;335:429. doi: 10.1136/bmj.39274.647465.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Steinman MA, Gonzales R, Linder JA, Landefeld CS. Changing use of antibiotics in community-based outpatient practice, 1991–1999. Ann Intern Med. 2003;138:525–33. doi: 10.7326/0003-4819-138-7-200304010-00008. [DOI] [PubMed] [Google Scholar]
- 5.Wong DM, Blumberg DA, Lowe LG. Guidelines for the use of antibiotics in acute upper respiratory tract infections. Am Fam Physician. 2006;74:955–66. [PubMed] [Google Scholar]
- 6.Panagakou SG, Spyridis N, Papaevangelou V, Theodoridou KM, Goutziana GP, Theodoridou MN, et al. Antibiotic use for upper respiratory tract infections in children: A cross-sectional survey of knowledge, attitudes, and practices (KAP) of parents in Greece. BMC Pediatr. 2011;11:60. doi: 10.1186/1471-2431-11-60. [DOI] [PMC free article] [PubMed] [Google Scholar]


