Abstract
Introduction:
Patients with threatened miscarriage associated with adverse pregnancy outcomes because of associated pregnancy and labor complications.
Objectives:
To evaluate the effect of threatened miscarriage on early and late pregnancy outcome.
Methods:
A retrospective case–controlled study was performed on 89 women with threatened miscarriage (study group) at Maternity and Children Hospital Buraidah, KSA from January 2010 to December 2010. They were matched for age and parity to 45 cases (control group) attending route antenatal clinic at the same time. Data recorded included, demographic characteristics and detailed pregnancy outcome and ultrasound finding including gestational age, cardiac activity and subchorionic hematoma.
Results:
The overall adverse pregnancy outcome was significantly higher in the studied cases compared to the control group (p=015).The miscarriage rate was significantly higher in study group compared to the controls group, (16.9%vs 2.2%, p=0000). Preterm delivery, babies with low birth weight and premature rupture of membranes were significantly higher in the miscarriage group compared to the controls group, (15.7% vs 2.2%, p=0.001), (15.7% vs 2.2%), p=0.001) and (6.7%) vs 4.45), p=0.016). There were no significant differences in other pregnancy outcomes.
Conclusion:
threatened miscarriage is associated with increased incidence of adverse pregnancy outcome. The risk is specially increased in premature rupture of the membranes, preterm delivery and neonatal birth weight.
Key words: adverse pregnancy, threatened miscarriage, preterm delivery, neonatal birth weight.
1. INTRODUCTION
Threatened abortion is defined as “pregnancy termination before turning 20 weeks of gestation or with a fetus born weighing less than 500gm” (1). It is the most common complication of pregnancy, occurring in 15-20% of ongoing pregnancy (2). The clinical diagnosis of threatened miscarriage is presumed when a bloody vaginal discharge or bleeding appears through a closed cervical os during the first half of pregnancy (3). About, 90-96% pregnancies with both fetal cardiac activity and vaginal bleeding at 7-11 weeks do not miscarry. The higher success rate is associated with bleeding at the later end of the gestational age range (4). In practice, once the bleeding has settled, these pregnancies are not considered high risk and do not required follow up. Ultrasound has modified the diagnosis and the approach to the management of miscarriage. Any woman with bleeding in early pregnancy is offered ultrasound to ascertain the viability, location of the placenta and furthermore, the presence or absence of subchorionic hematoma which is associated with 4-33% rate of miscarriage (5).
Early pregnancy bleeding is associated with adverse pregnancy outcome. Threatened abortion has associated with preterm labor and low birth weight (6), pre-eclampsia, preterm prelabour rupture of membranes (PPROM), placental abruption and intrauterine growth restriction (IUGR) (7). In this study we have examined cases of threatened miscarriage retrospectively from early in the first trimester till the ultimate outcome; we aimed to evacuate maternal and perinatal outcomes in this high risk group.
2. MATERIALS AND METHODS
This study was conducted in the department of Obstetrics and Gynecology, Maternity and Children’s Hospital Buraidah Al Qassim, KSA, from January 2010 to December 2010. Total of 89 cases were included in the study and had ultrasound after presenting with symptoms of threatened abortion at or below 20 weeks of gestation. The diagnostic criteria for threatened miscarriage was based on documented fetal cardiac activity on ultrasound with a history of vaginal bleeding in the presence of a closed cervix and gestational age at 20 weeks or less (Saraswat Let, al. 2009) (8). Patients with threatened miscarriage were admitted to hospital for bed rest, they received Dydrogesterone (duphaston) 10mg twice/per day. They were matched for age and parity to 45 cases control group had attended antenatal clinic during the same period. Control cases were excluded if they had developed bleeding in early pregnancy or gave a history of bleeding in early pregnancy. All ultrasound examinations were performed by the same operator using GE logic 200, in a frequency of 3.5 and 6.5 MHZ for transabdominal and transvaginal scan respectively. Patients were revaluated and followed up as needed till ultimate outcome. The following sonographic factors were evaluated, size of the gestational sac, and fetal cardiac activity, patients notes were revised for antenatal complications and maternal and perinatal outcomes.
Statistical analysis was performed using SPSS 15 for windows. Pregnancy outcomes were compared using x2 test, and the gestational ages and birth weights were compared using t test.
3. RESULTS
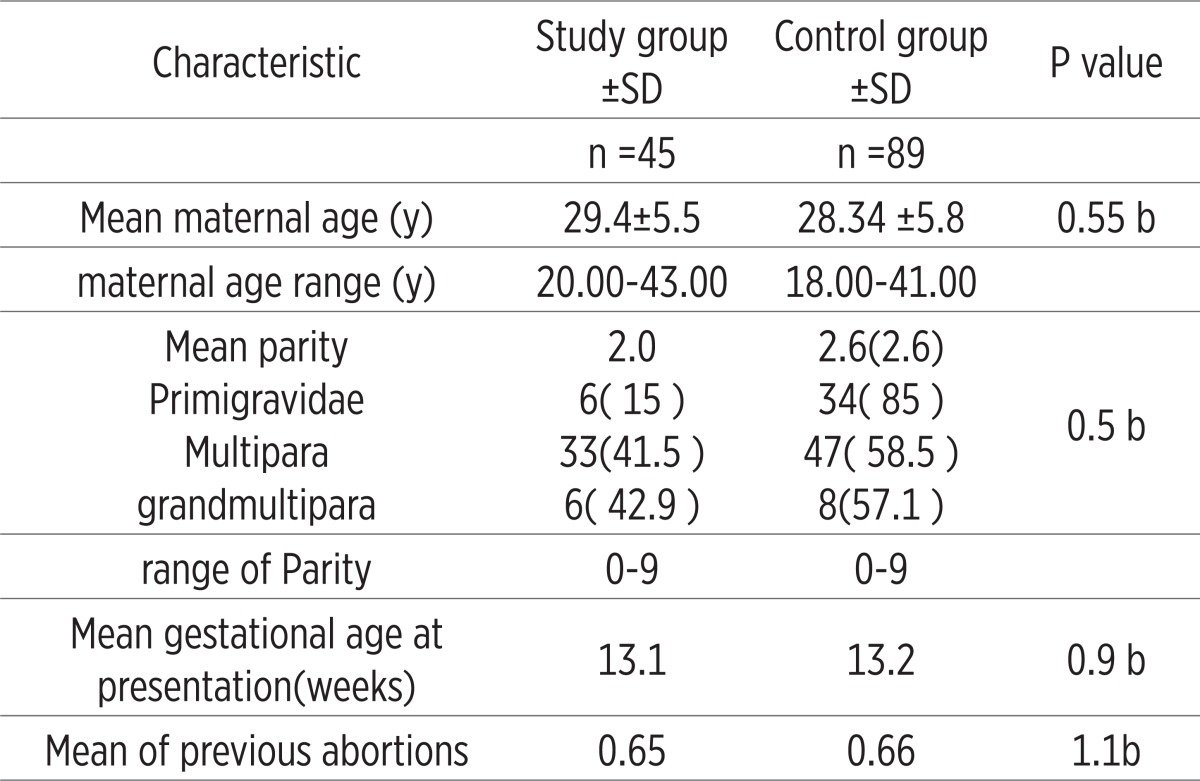
A total of 134 women were included in this study, 89 women with threatened miscarriage and 45 controls. The demographic factors and pregnancy loss for the two groups are presented in Table 1. The mean maternal ages for the threatened miscarriage and the control groups were 29.4±5.5 and 28.34 ±5.8, ranged (20 to 43) years respectively. There was no significant difference within age distribution of the groups (p=0.55). The mean parity for the study and the control groups were 2.0 and 2.6 deliveries respectively (p=0.5). In the study group, 57.5% were multiparous, compared to 51.7% in the control group, both groups ranged 0 to 9. The mean gestational age at presentation for the threatened miscarriage group was 13.1weeks compared to 13.2 in the controlled group.
Table 1.
Maternal Characteristics in 89 Women With Threatened Miscarriage Compared With 45 Asymptomatic Controls. SD, standard deviation, P value a significant, b insignificant, Values are mean±SD
 |
The overall adverse pregnancy outcomes was significantly higher in women with threatened miscarriage than the control group (p=015). Pregnancy outcomes between the two groups are shown in Table 2. The overall miscarriage rate was significantly higher in the threatened miscarriage group compared to controls group15 (16.9%) vs 1(2.2%) respectively (p=0.000). Our investigations showed that women with threatened miscarriage had a significantly increased risk of preterm labor (less 37 weeks of gestation) compared with the control group (15.7% vs 2.2%, p=0.016). Women with threatened miscarriage had significantly small babies weighing less than 2.5 kg compared with the control group (15.7% compared to 2.2% respectively), with a mean birth weight(2.4 ±1.13851 vs 3.1±0.36709, p=000).
Table 2.
Adverse Pregnancy Outcome in 89 Women with Threatened Miscarriage Compared to 45 in the Control Group.
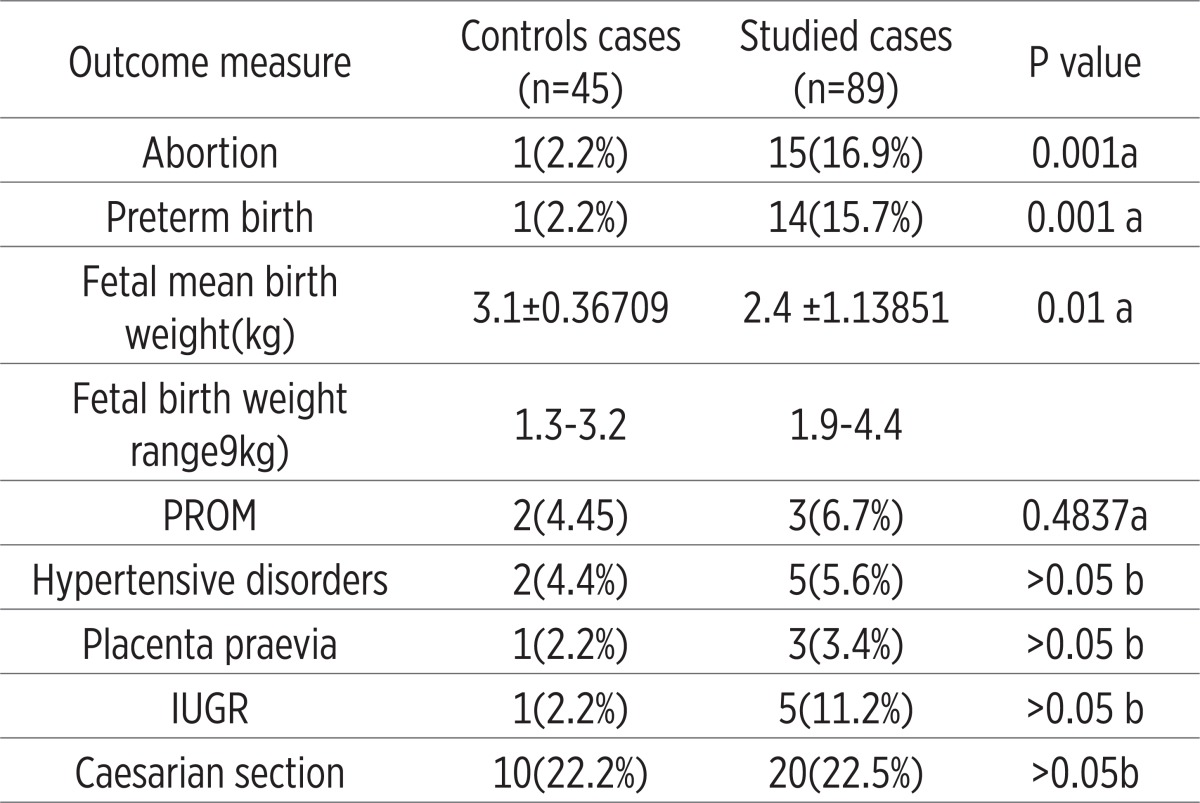 |
There were no significant differences in the incidence of PROM, IUGR, preeclampsia, placenta praevia and the rate of cesarean section between the two groups Table 2.
4. DISCUSSION
Bleeding in early pregnancy is a common gynecological complaint. These data showed that patients having threatened miscarriage had a significantly increased risk of complete abortion, preterm labor and low birth weight infants. Other pregnancy complications such as placenta praevia, IUGR, PIH, PROM and cesarean section rates were relatively increased, but not at significant levels. These data showed that the prediction of positive outcome in threatened abortion after confirmation of positive cardiac action on sonography was 83.1%. Similar previous evidences were reported by Goldstein et al. (1983), Batzofin et al. (1996 and 1984) and Ball RH et al. (1996) (6, 9, 10). There was no change in survival rate this constant value can be explained by the frequently offered unrewarding treatment by porgestagens and bed rest, which is supported by poor quality data.
The literature reports on the association between bleeding in early pregnancy and pregnancy outcome is a conflicting one. Many investigators reported increase incidence of preterm birth and low birth weight following threatened miscarriage (4, 11). On the contrary, there are fewer literature reports that find normal development following threatened miscarriage (12, 13). Similarly it was reported that the incidence of placental abruption and placenta praevia (14) and premature rupture of the membranes (15) were higher among patients with threatened miscarriage as compared to non threatened group, other evidence showed that such a relation is not yet established (16, 17). Lack of consistencies between these different studies, was observed in definition of the upper limits of abortion used, size of the study population, gestational age at presentation and to a lesser extent the statistical test used. It appeared that the definitive relationship between threatened miscarriages at adverse pregnancy outcome is not yet established. The positive value of this assumption raises the awareness of practitioners of the possible complications that may follow.
In the present study, significantly suboptimal outcome was greater for preterm birth (before 37 weeks of gestation) and low birth weight. Preterm labor and premature rupture of membranes may be considered as one phenomenon, because both conditions are intermingling. The low birth weight and lower Apgar score observed in the study cases is a logic sequence of preterm birth and possibly a lower level of antenatal care given. It seems that all of the above adverse pregnancy outcomes are consequences of PROM. There is evidence that later pregnancy complications such as preterm labor and premature rupture of the membranes may be due to impaired placentation (18) and more recently reactive oxygen species (19)as a result of early pregnancy insult. This assumption is probably a risk rather than etiological factor, because it will not explain cases of premature rupture of the membranes and preterm labor seen in patients with non threatened miscarriage. Therefore, it is still conceivable that other factors are responsible for late pregnancy complication seen in threatened miscarriage group.
In conclusion the exact cause of miscarriage is debatable, despite that several factors have been correlated with higher miscarriage rates. In preterm labor, despite intensive researches, rates have not changed over the past 40 years. It is possible that more than one process is involved in the pathogenesis of these two conditions. One of the shortcomings on previous researches is that the majority were retrospectives. More prospective researches should be encouraged.
REFERENCES
- 1.F. gray Cunningham, Kenneth J. Leveno, Steven L. Bloom, John C. Hauth, Lary C. Gilsstrap, and Katharine D. Wenstrom. 23th. 2010. William’s obstetrics; pp. 215–224. [Google Scholar]
- 2.Farrell T, Owen P. The significance of extrachorionic membrane separation in threatened miscarriage. Br J Obstet Gynecol. 1996;103:926–8. doi: 10.1111/j.1471-0528.1996.tb09915.x. doi: 10.1111/j.1471 0528. [DOI] [PubMed] [Google Scholar]
- 3.F. gray Cunningham, Kenneth J. Leveno, Steven L. Bloom, John C. Hauth, Lary C. Gilsstrap, and Katharine D. Wenstrom. Williams’s obstetrics. 23th. 2010. Clinical diagnosis of threatened miscarriage; pp. 215–224. [Google Scholar]
- 4.Tongsong T, Srisomboon J, Wanapirak C, et al. Pregnancy outcome with threatened abortion with demonstrable fetal cardiac activity: A cohort study. J obstet Gynecol (Tokyo 1995) 1995;21:331–5. doi: 10.1111/j.1447-0756.1995.tb01019.x. PMID8775901. [DOI] [PubMed] [Google Scholar]
- 5.Pearlstone M, Baxi L. Subchorionic haematoma: A review. Obstet Gynecol Surv. 1993;48:65–8. PMID: 8437776. [PubMed] [Google Scholar]
- 6.Baztofin JH, Fielding WL, Friedman EA. Effect of vaginal bleeding in early pregnancy outcome. Obstet Gynecol. 1984;63:515–8. PMID: 6700898. [PubMed] [Google Scholar]
- 7.Weiss JL, Malone FD, Vidaver J, Ball RH, Nyberg DA, Comstock CH, et al. Threatened abortion: a risk factor for poor pregnancy outcome, a population-based screening study. Am J Obstet Gynecol. 2004;190:745–50. doi: 10.1016/j.ajog.2003.09.023. PMID: 15042008. [DOI] [PubMed] [Google Scholar]
- 8.Saraswat L, Bhattacharya S, Maheshwari A, Bhattacharya S. Maternal and perinatal outcome in women with threatened miscarriage in the first trimester: a systematic review. BJOG. 2010 Feb;117(3):245–57. doi: 10.1111/j.1471-0528.2009.02427.x. Epub 2009 Nov 26. [DOI] [PubMed] [Google Scholar]
- 9.Goldstien SR, Subramanyam BR, Raghavendra BN, Horii SC, Hilton S. Subchrionic bleeding in threatened abortion: sonographic finding and significance. AJR. 1983;141:975–978. doi: 10.2214/ajr.141.5.975. PMID: 6605073. [DOI] [PubMed] [Google Scholar]
- 10.Ball RH, Ade CM, Schoenborn JA, Crane JP. The clinical significance of ultrasonographically detected subchorionichemorrhages. Am J Obstet Gynecol. 1996;174:996–1002. doi: 10.1016/s0002-9378(96)70339-3. PMID: 8633682. [DOI] [PubMed] [Google Scholar]
- 11.Dickey RP, Olar TT, Curole DN, Taylor SN, Matulich EM. Relationship of first trimester subchorionic bleeding detected by color Doppler ultrasound to subchorionic fluid, clinical bleeding and pregnancy outcome. Obstet Gynecol. 1992;80:415–20. PMID: 1365697. [PubMed] [Google Scholar]
- 12.Buck C, Gregg R, Stavarky K, et al. The effect of single prenatal and natal complications upon the development of children of mature birth weight. Pediatrics. 1969;43:942. PMID: 5786218. [PubMed] [Google Scholar]
- 13.Barker DJ, Edward JH. Obstetrics complications and school performance. Br Med J. 1967;3:695. doi: 10.1136/bmj.3.5567.695. PMID: 5786218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sheiner E, Levy A, Katz M, Mazor M. Pregnancy outcome following recurrent spontaneous abortions. Eur J Obstet Gynecol Reprod. Biol. 2005;118:61–65. doi: 10.1016/j.ejogrb.2004.06.015. PMID: 15596274. [DOI] [PubMed] [Google Scholar]
- 15.Buchmayer SM, Spare´n P, Cnattingius S. Previous pregnancy loss: risks related to severity of preterm delivery. Am J Obstet Gynecol. 2004;191:1225–1231. doi: 10.1016/j.ajog.2004.02.066. PMID: 15507945. [DOI] [PubMed] [Google Scholar]
- 16.Pearlstone M, Baxi L. Subchorionic haematoma: A review. Obstet Gynecol Surv. 1993;48:65–8. PMID:8437776. [PubMed] [Google Scholar]
- 17.Mantoni M, Fog Pedersen J. Intrauterine haematoma - Anultrasonic study of threatened abortion. Br J Obstet Gynaecol. 1981;88:47–51. doi: 10.1111/j.1471-0528.1981.tb00936.x. PMID: 7459291. [DOI] [PubMed] [Google Scholar]
- 18.Khong TY, De Wolf F, Robertson WB, Brosens I. Inadequate maternal vascular response in pregnancies complicated by pre-eclampsia and by small for gestational age infants. Br J Obstet Gynaecol. 1986;93:1049–59. doi: 10.1111/j.1471-0528.1986.tb07830.x. PMID: 3790464. [DOI] [PubMed] [Google Scholar]
- 19.Plessinger MA, Woods JR, Miller R. Pretreatment of human amnion-chorion with vitamins C and E preventshypochlorous acid-induced damage. Am J Obstet Gynecol. 2000;183:979–85. doi: 10.1067/mob.2000.106676. PMID: 11035350. [DOI] [PubMed] [Google Scholar]


