Abstract
Objective
To investigate the influence of performance feedback and motivation during two tests of simple visuo-motor reaction time.
Design
Cross-sectional, observational study.
Setting
Outpatient academic physiatry clinic.
Participants
31 healthy adults aged 54 ± 15 years.
Methods
Participants completed a clinical test of reaction time (RTclin) and a computerized test of reaction time with and without performance feedback (RTcompFB and RTcompNoFB, respectively) in randomly assigned order. They then ranked their degree of motivation during each test. RTclin measured the time required to catch a suspended vertical shaft by hand closure after its release by the examiner. RTcompFB and RTcompNoFB both measured the time required to press a computer key in response to a visual cue displayed on a computer monitor. Performance feedback (visual display of the previous trial and summary results) was provided for RTcompFB, but not for RTcompNoFB.
Main Outcome Measurements
Means and standard deviations of RTclin, RTcompFB, and RTcompNoFB; Participants’ self-reported motivation on a 5-point Likert scale for each test.
Results
There were significant differences in both the means and standard deviations of RTclin, RTcompFB, and RTcompNoFB (F2,60 = 81.66, p < 0.0001; F2,60 = 32.46, p < 0.0001, respectively) with RTclin being both the fastest and least variable of the reaction time measures. RTclin was more strongly correlated with RTcompFB (r = 0.449, p = 0.011) than with RTcompNoFB (r = 0.314, p = 0.086). Participants reported similar levels of motivation between RTclin and RTcompFB, both of which were reported to be more motivating than RTcompNoFB.
Conclusions
The stronger correlation between RTclin and RTcompFB as well as the higher reported motivation during RTclin and RTcompFB testing suggest that performance feedback is a positive motivating factor that is implicit to RTclin testing. RTclin is a simple, inexpensive technique for measuring reaction time and appears to be an intrinsically motivating task. This motivation may promote faster, more consistent reaction time performance compared to currently available computerized programs, which do not typically provide performance feedback.
INTRODUCTION
Reaction time (RT) is an important performance measure with broad functional relevance that is under-utilized in routine clinical practice. In order to safely perform basic day-to-day activities human beings rely on the ability to rapidly react to their environment. Reaction time has been found to be predictive of multiple walking parameters including gait speed, both on level surfaces [1, 2], and on stairs [3]. Furthermore, an increased, or slower, RT has been associated with falls in young, healthy people [4] as well as in the general older population [5–8]. Longer RT’s have been associated with an increased risk of motor vehicle accidents in a driving simulator in many clinical populations including those with depression [9], Huntington’s disease [10], Alzheimer’s dementia [11], and obstructive sleep apnea [12]. Complex RT has been found to correlate strongly with on-road driving performance evaluations conducted on elderly drivers in traffic [13]. In addition, color choice RT was found to be one of the 3 visual, cognitive, and motor tests most predictive of driving safety during a standardized on-road test of driving performance in elderly drivers [14]. In a large prospective survival study, mean choice RT and simple RT variability were even identified as the best independent predictors of mortality among all of the potential predictor variables studied [15].
In addition to its value as a predictor of performance for a variety of functional tasks, RT is known to be prolonged in many of the populations commonly encountered in physiatric practice. Examples include stroke [16], traumatic brain injury [17, 18], dementia [19, 20], polyneuropathy [21, 22], and those experiencing adverse medication side-effects [23, 24]. The role of RT prolongation in sport related concussion deserves special mention. Several computerized cognitive assessment tools have been developed to assess cognitive performance in athletes suspected of having sustained a concussion, each of which include a measure of RT. The IMPACT (Immediate Post-concussion Assessment and Cognitive Test) [25], CogState-Sport [26], and ANAM (Automated Neuropsychological Assessment Metrics) [27] computerized neurocognitive test batteries are three of the most popular examples of such programs. In the setting of sport related concussion it is now advocated that each athlete’s baseline cognitive performance be assessed using one of these programs during the preseason so that after-injury comparisons can be made following concussion with the goal of determining when the athlete has recovered back to their own individual cognitive baseline [28–29].
While RT is both affected by many disease and injury processes as well as predictive of many outcomes of important functional relevance, it remains underutilized in routine clinical practice. One important reason for this is that RT assessment typically requires access to a computer equipped with specialized software or to other lab-based equipment that are not available in most clinical settings. To address this, we developed a low-tech, inexpensive clinical measure of simple visuo-motor RT (RTclin). The technique involves the standardization of a simple experiment commonly performed in high school physics classrooms (e.g., Chudler [30]). The apparatus used is a thin, rigid cylinder affixed to a weighted disc that assures verticality and consistency of hand position. The apparatus is vertically suspended before being released by the examiner and caught as quickly as possible by the subject being evaluated. The distance the apparatus falls before being arrested is measured, in cm, and converted into the clinical reaction time (RTclin), in ms, using the formula for a free body falling under the influence of gravity.
We have found that RTclin is reliable and valid in a healthy adult population [31] and a population of collegiate athletes [32, 33]. We have demonstrated that RTclin is strongly correlated with the ability to raise the hands to protect the head [34] and we have completed preliminary work demonstrating that RTclin is prolonged after sport-related concussion as compared to baseline testing [35]. While collecting the data for these studies, we have observed that study participants generally appear to be highly motivated to perform their best during RTclin testing. This observation has been especially noticeable in the athletes we have tested, who typically appear to be much more motivated during RTclin testing than during concurrently administered computerized cognitive test batteries. In the sport concussion setting it is especially important that the athlete being tested be motivated to give their best effort during baseline testing as the results of this testing will be used as a basis for comparison following concussion. Since athletes know that they will not receive medical clearance for return to play unless their post-injury test performance compares favorably to their baseline test performance, the post-injury test environment is one in which they are typically highly motivated to perform well [36]. If there is a difference in the athlete’s level of motivation during baseline and post-injury testing, then this differential motivation may confound the effects of concussion on test performance [36].
Given these observations, we hypothesize that performance feedback in the form of knowledge of results plays an important role in motivating subjects during RTclin testing since they receive implicit visual feedback during each trail in the form of the distance the apparatus fell before being caught. In contrast, knowledge of results is not typically provided during computerized RT assessment. We further hypothesize that more highly motivated subjects will put forth greater effort during RT testing, resulting in improved performance. Therefore, the purpose of this study was to compare participant motivation and performance during RTclin testing to that during computerized RT testing with (RTcompFB) and without (RTcompNoFB) performance feedback in the form of knowledge of results.
METHODS
Subjects
We recruited 31 adult volunteers (45% female; mean age 54 ± 15 years, range 22–84 years) from the waiting room of an outpatient academic physical medicine & rehabilitation clinic while they waited for friends or relatives to complete their medical appointments. Adults over the age of 18 with no history of disease or injury involving the central or peripheral nervous system or to the dominant upper extremity were eligible to participate. Participants were excluded if they had corrected visual acuity less than 20/40, were not fluent in English, or in the preceding 30 days had started a new medication or changed the dose of a medication known or suspected to affect the central or peripheral nervous system. All study participants provided informed written consent that was approved by the IRB at the lead author’s institution prior to participating.
Data collection
Testing was conducted in a quiet, well lit room by a single examiner. Each study participant completed RTclin, RTcompFB, and RTcompNoFB testing in randomly assigned order. Upon completing all 3 tests, study participants were asked to rate their level of motivation during each RT test using the following 5-point Likert scale: 1 = not motivated, 2 = somewhat motivated, 3 = moderately motivated, 4 = very motivated, 5 = extremely motivated.
Measurement of RTclin
RTclin was measured as previously described [31–33, 35] using an 80 cm dowel rod coated in high-friction tape and marked in 0.5 cm increments that was embedded into a weighted rubber disc of diameter 7.5 cm, height 2.5 cm, and weight 256 g. Participants sat at a table with their dominant forearm resting at the edge of the table surface, such that their hypothenar eminence was positioned at the edge of the table with their hand in an open “C shape” position. The examiner suspended the apparatus vertically such that the weighted disk was positioned within the participant’s open hand with the participants’ first and second digits within approximately 0.5 cm of the disk and the top of the disk aligned horizontally with the participants’ first and second digits. At pre-determined randomly assigned time intervals ranging from 2 to 5 s, the examiner released the apparatus and the participant caught it as quickly as possible once it began to fall. The examiner recorded the distance the apparatus fell, in cm, by recording the position of superior-most aspect of the participants’ hands after they completely arrested the falling apparatus. Participants were given 4 practice trials before data were collected for 8 trials. If a participant was unsuccessful in catching the apparatus, resulting in its falling to the floor then a “drop” trial was recorded and the examiner continued with the next trial. The fall distances were then converted into RTclin values, in ms, using the formula for a body falling under the influence of gravity (g = ½ dt2). Mean and standard deviations were then calculated for RTclin for each participant.
Measurement of RTcomp
RTcompFB and RTcompNoFB were measured using a Windows-based personal laptop computer running two simple RT tasks programmed in E-Prime (Version 1.1. Pittsburgh, PA: Psychology Software Tools, Inc.). In both computerized RT tests, participants sat at the laptop computer with their dominant hand resting comfortably over the keyboard and their gaze fixed on the monitor. At the beginning of each trial a black circle was presented on a white background. The circle was then replaced by a black “X” after a randomly assigned time delay ranging from 2 to 5 s for each of 4 practice and 40 data acquisition trials. Participants were instructed to depress the space bar as quickly as possible after the visual stimulus changed. The program recorded the elapsed time in ms for each trial and saved this data on the device’s hard drive. The 2 computerized RT tasks were identical, except that RTcompFB provided performance feedback after each trial while RTcompNoFB did not. After each RTcomp+FB trial the participant’s measured RT for that trial, as well as their longest and shortest RTs for the set of trials, were presented. In contrast, after each RTcompNoFB trial, the program displayed the following neutrally-worded statement: “Get ready now for the next trial.” If any irregularities occurred, including depressing the space bar before the stimulus cue or attempting to depress the space bar but the attempt not being registered by the computer, then the examiner noted the trial number and that data point was omitted from the final analysis. Mean and standard deviations were calculated for RTcompFB and RTcompNoFB for each participant.
Statistical Analysis
The data for all 3 RT tests appeared right skewed based on visual inspection of data histograms and normal probability plots. Therefore the data were log transformed to allow the data to more closely approximate normality. The standard deviations of each subject’s response were used as a measure of within subject variability. The means and standard deviations of the various reaction times were evaluated using repeated measures ANOVA. The RT condition was a within-subjects factor to evaluate group differences in the 3 RT conditions. Pearson correlation coefficients were calculated to assess the strength of the relationships between mean RTclin, RTcompFB, and RTcompNoFB. Fisher’s exact test was used to compare the distribution of self-reported motivation ranking scores between the 3 RT conditions. All statistical analyses were performed using SAS (Version 9.1. Cary, NC: SAS Institute Inc.). Figure 1 was generated using Microsoft Excel (Version 12.0. Seattle, WA: Microsoft Corp.).
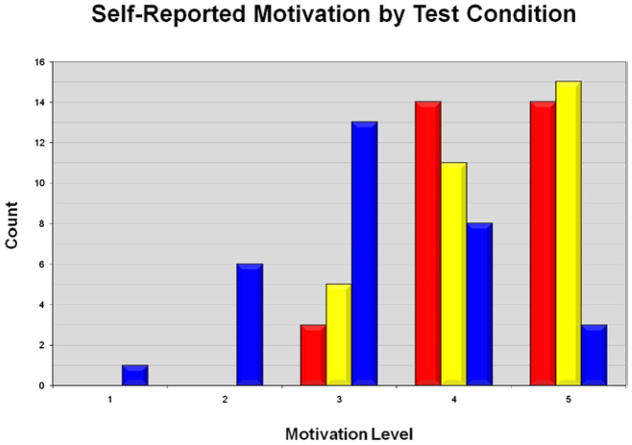
Figure 1.
Graphical illustration of participant self-reported motivation during each of the 3 RT test conditions: RTclin (red), RTcompFB (yellow), RTcompNoFB (blue). 1 = not motivated, 2 = somewhat motivated, 3 = moderately motivated, 4 = very motivated, 5 = extremely motivated.
RESULTS
Mean RT, as well as RT variability as measured by standard deviation, differed significantly between the 3 tests, with RTclin being the fastest and least variable measure: mean RTclin = 234 ± 28 ms, mean RTcompFB = 301 ± 45 ms, mean RTcompNoFB = 327 ± 52 ms, F2,60 = 81.66, p < .0001; RTclin variability = 26 ± 14 ms, RTcompFB variability = 80 ± 54 ms, RTcompNoFB variability = 88 ± 60 ms, F2,60 = 32.46, p < 0.0001 (Table 1). There was a significant positive correlation between RTclin and RTcompFB (r = 0.449, p = 0.011), whereas a weaker, non-significant correlation was observed between RTclin and RTcompNoFB (r = .314, p = 0.086).
Table 1.
Mean RT and RT variability, as measured by SD, for each of the 3 RT test conditions.
| RT Test Condition | Mean RT | RT Variability |
|---|---|---|
| RTclin | 234 ± 28 ms* | 26 ± 14 ms** |
| RTcompFB | 301 ± 45 ms* | 80 ± 54 ms** |
| RTcompNoFB | 327 ± 52 ms* | 88 ± 60 ms** |
F2,60 = 81.66, p < .0001 for test of equality across groups; F1,30 = 93.07, p< .0001 for RTclin-RTcompFB comparison;F1,30 = 133.53, p< .0001 for RTclin-RTcompNoFB comparison; F1,30 = 11.14, p= .0023 for RTcompFB-RTcompNoFB comparison.
F2,60 = 32.46, p < .0001 for equality across groups; F1,30 = 37.36, p< .0001 for RTclin-RTcompFB comparison;F1,30 = 75.01, p< .0001 for RTclin-RTcompNoFB comparison; F1,30 = 0.52, p= .4748 for RTcompFB-RTcompNoFB comparison.
Figure 1 illustrates the distribution of participants’ self-reported motivation level during each of the 3 test conditions. Participant motivation differed across tests (p < .0001). This finding was driven by differential motivation between RTclin and RTcompNoFB (p < .0001) as well as RTcompFB and RTcompNoFB (p = .0002). Participant motivation was similar between RTclin and RTcompFB (p = .6057). When participants were asked to directly compare their level of motivation between RTclin and RTcompFB, 26% rated RTclin as more highly motivating, 52% rated them as equally motivating, and 22% rated RTclin as less highly motivating. When the same comparison was made between RTclin and RTcompNoFB, 74% rated RTclin as more highly motivating and 26% rated RTclin and RTcompNoFB as equally motivating.
DISCUSSION
Reaction time is typically measured using computer programs that do not provide performance feedback and are not routinely available in most clinical settings. We developed RTclin to increase the availability of RT testing to clinicians. RTclin can easily be measured during a clinical encounter using simple low-tech equipment that costs far less than the computer software currently available for RT assessment. The nature of RTclin testing inherently provides the test subject with performance feedback after each trial since they can see how far the device fell before being caught. In this study, participants rated RTclin as being similarly motivating to RTcompFB, a computerized RT test that provides performance feedback after each trial, and more motivating than RTcompNoFB, a computerized RT test that does not provide performance feedback. Furthermore, RTclin correlated more strongly with RTcompFB than RTcompNoFB and was significantly faster and less variable than either of the computerized RT measures. These findings suggest that performance feedback, which is an intrinsic quality of RTclin, improves motivation during RT testing. A high level of motivation on the part of the test taker may contribute to faster, more consistent RTclin results. Previous work [33] which found RTclin to be more consistent over one year than an accepted computerized measure of reaction time supports this perspective.
The main argument against providing feedback during RT testing is that feedback “facilitates the learning process” and that “learning should not be reflected in RT measures [37].” The literature evaluating the effect of performance feedback on RT measurement does support the idea that knowledge of results improves RT performance [38–43]. In fact, only partial or even false knowledge of results have been shown to improve RT performance compared to no knowledge of results [38, 39, 43]. The subjective observation that study participants given knowledge of results appear to be more motivated to perform well than those given no knowledge of results is not unique to our work [40]. When the mechanism by which knowledge of results improves RT was investigated, it was demonstrated that goal-setting on the part of the study participants, and not the amount of knowledge of results provided, was responsible for the positive effect of feedback on RT performance [42]. This further supports the concept that knowledge of results works to improve RT performance by increasing subject motivation.
While there is a theoretical concern that performance feedback may facilitate learning during RT measurement, it is unclear how much RT improvement a study participant can achieve through a learning effect during such a simple, rapid task as RTclin. In this study, the potential learning effect was minimized by randomly assigning the intervals at which both RT tasks required response. Furthermore, the potential learning effect needs to be balanced against the motivating effect subjects receive from performance feedback. Motivated participants are more likely to give a consistently high level of effort during RT measurement than unmotivated or bored participants. This is especially important when baseline RT performance is compared to post-concussion RT performance in highly motivated athletes, as is increasingly popular in the field of sport concussion management. In this setting, especially, reliable baseline RT data that represents an athlete’s best effort is essential to ensure an “apples to apples” comparison between baseline and after-injury data.
The merits of this study are tempered by its limitations. This study was designed with differing numbers of trials between the clinical and computerized RT test protocols. While this may affect statistical comparisons between the test methods, particularly comparisons of variability, it was done intentionally in an effort to simulate a “real world” test environment. At least 40 RT trials have been advocated to accurately represent a study subject’s actual ability [37], and most commonly used computer-based RT tests include approximately this number of trials. In contrast, the intention of RTclin is to provide clinicians with rapid method of measuring RT that is feasible in a busy clinical setting. During pilot reliability and validity testing we found that analysis of 8 trials yielded statistically similar results to analyses including larger numbers of trials [31]. Therefore, in an effort to limit testing time we chose to use an RTclin testing protocol comprised of 8 trials. A second study limitation is that RTclin is limited by a “ceiling effect,” in that RT’s greater than 400 ms cannot be recorded The reason for this is that the 80 cm device falls for only about 400 ms before striking the ground. In practice, it is rare that a study participant is unable to generate a response within 400 ms. This did not occur once during data collection for this study and it only occurred on 0.1% of simple RTclin trials during our pilot reliability and validity study [31]. If the computerized RT data are truncated at an analogous “ceiling” value of 400 ms, there are no changes in the results or conclusions. A third limitation of this study is that the Likert scale used to assess study participant motivation during the 3 methods of RT assessment are novel and have not been independently validated as outcome measures. Yet they are simple and straight-forward with good face validity, and the associated results were not ambiguous.
CONCLUSION
RTclin is a simple, inexpensive method of measuring RT that provides intrinsic performance feedback, which appears to be a positively motivating factor. Improved subject motivation is likely to promote better effort during testing and results that more consistently represent a subject’s true abilities. While this may be especially beneficial in the setting of pre-post RT comparisons, as is commonly used in the field of sport concussion management, a clinical tool capable of consistently measuring a subject’s optimum RT may have additional valuable applications in physiatric practice. Further work is warranted to define RTclin’s potential role in such diverse areas as medication side-effect monitoring, fall risk assessment, driver safety evaluation, and response monitoring during the treatment of sleep apnea and other medical conditions that can impair RT. In conclusion, RTclin is a promising clinical tool that appears to offer advantages over currently-available computer-based RT assessment methods including simplicity, low cost, and intrinsic motivation.
Contributor Information
James T. Eckner, Department of Physical Medicine and Rehabilitation, University of Michigan.
SriKrishna Chandran, Department of Physical Medicine and Rehabilitation, Johns Hopkins University.
James K. Richardson, Department of Physical Medicine and Rehabilitation, University of Michigan.
References
- 1.Callisaya ML, Blizzard L, Schmidt MD, McGinley JL, Lord SR, Srikanth VK. A population-based study of sensorimotor factors affecting gait in older people. Age Ageing. 2009;38(3):290–295. doi: 10.1093/ageing/afp017. [DOI] [PubMed] [Google Scholar]
- 2.Lord SR, Lloyd DG, Li SK. Sensori-motor function, gait patterns and falls in community-dwelling women. Age Ageing. 1996;25(4):292–299. doi: 10.1093/ageing/25.4.292. [DOI] [PubMed] [Google Scholar]
- 3.Tiedemann AC, Sherrington C, Lord SR. Physical and psychological factors associated with stair negotiation performance in older people. J Gerontol A Biol Sci Med Sci. 2007;62(11):1259–1265. doi: 10.1093/gerona/62.11.1259. [DOI] [PubMed] [Google Scholar]
- 4.Smeesters C, Hayes WC, McMahon TA. The threshold trip duration for which recovery is no longer possible is associated with strength and reaction time. J Biomech. 2001;34(5):589–595. doi: 10.1016/s0021-9290(01)00005-7. [DOI] [PubMed] [Google Scholar]
- 5.Lord SR, Clark RD, Webster IW. Physiological factors associated with falls in an elderly population. J Am Geriatr Soc. 1991;39(12):1194–1200. doi: 10.1111/j.1532-5415.1991.tb03574.x. [DOI] [PubMed] [Google Scholar]
- 6.Lord SR, Ward JA, Williams P, Anstey KJ. Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc. 1994;42(10):1110–1117. doi: 10.1111/j.1532-5415.1994.tb06218.x. [DOI] [PubMed] [Google Scholar]
- 7.Lord SR, Fitzpatrick RC. Choice stepping reaction time: a composite measure of falls risk in older people. J Gerontol A Biol Sci Med Sci. 2001;56(10):M627–M632. doi: 10.1093/gerona/56.10.m627. [DOI] [PubMed] [Google Scholar]
- 8.Lajoie Y, Gallagher SP. Predicting falls within the elderly community: comparison of postural sway, reaction time, the Berg balance scale and the Activities-specific Balance Confidence (ABC) scale for comparing fallers and non-fallers. Arch Gerontol Geriatr. 2004;38(1):11–26. doi: 10.1016/s0167-4943(03)00082-7. [DOI] [PubMed] [Google Scholar]
- 9.Bulmash EL, Moller HJ, Kayumov L, Shen J, Wang X, Shapiro CM. Psychomotor disturbance in depression: assessment using a driving simulator paradigm. J Affect Disord. 2006;93(1–3):213–218. doi: 10.1016/j.jad.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 10.Rebok GW, Bylsma FW, Keyl PM, Brandt J, Folstein SE. Automobile driving in Huntington’s disease. Mov Disord. 1995;10(6):778–787. doi: 10.1002/mds.870100611. [DOI] [PubMed] [Google Scholar]
- 11.Rebok GW, Keyl PM, Bylsma FW, Blaustein MJ, Tune L. The effects of Alzheimer disease on driving-related abilities. Alzheimer Dis Assoc Disord. 1994;8(4):228–240. doi: 10.1097/00002093-199408040-00002. [DOI] [PubMed] [Google Scholar]
- 12.Pichel F, Zamarron C, Magan F, Rodriguez JR. Sustained attention measurements in obstructive sleep apnea and risk of traffic accidents. Respir Med. 2006;100(6):1020–1027. doi: 10.1016/j.rmed.2005.09.036. [DOI] [PubMed] [Google Scholar]
- 13.Odenheimer GL, Beaudet M, Jette AM, Albert MS, Grande L, Minaker KL. Performance-based driving evaluation of the elderly driver: safety, reliability, and validity. J Gerontol. 1994;49(4):M153–M159. doi: 10.1093/geronj/49.4.m153. [DOI] [PubMed] [Google Scholar]
- 14.Wood JM, Anstey JK, Kerr GK, Lacherez PF, Lord S. A multidomain approach for predicting older driver safety under in-traffic road conditions. J Am Geriatr Soc. 2008;56(6):986–993. doi: 10.1111/j.1532-5415.2008.01709.x. [DOI] [PubMed] [Google Scholar]
- 15.Deary IJ, Der G. Reaction time explains IQ’s association with death. Psychol Sci. 2005;16(1):64–69. doi: 10.1111/j.0956-7976.2005.00781.x. [DOI] [PubMed] [Google Scholar]
- 16.Miscio G, Pisano F, Del Conte C, Colombo R, Schieppati M. Concurrent changes in shortening reaction latency and reaction time of forearm muscles in post-stroke patients. Neurol Sci. 2006;26(6):402–410. doi: 10.1007/s10072-005-0523-0. [DOI] [PubMed] [Google Scholar]
- 17.McDowell S, Whyte J, D’Esposito M. Working memory impairments in traumatic brain injury: evidence from a dual-task paradigm. Neuropsychologia. 1997;35(10):1341–1353. doi: 10.1016/s0028-3932(97)00082-1. [DOI] [PubMed] [Google Scholar]
- 18.Warden DL, Bleiberg J, Cameron KL, et al. Persistent prolongation of simple reaction time in sports concussion. Neurology. 2001;57(3):524–526. doi: 10.1212/wnl.57.3.524. [DOI] [PubMed] [Google Scholar]
- 19.Ferris S, Crook T, Sathananthan G, Gershon S. Reaction time as a diagnostic measure in senility. J Am Geriatr Soc. 1976;24(12):529–533. doi: 10.1111/j.1532-5415.1976.tb03277.x. [DOI] [PubMed] [Google Scholar]
- 20.Gorus E, Lambert M, De Raedt R, Mets T. The influence of galantamine on reaction time, attention processes, and performance variability in elderly Alzheimer patients. J Clin Psychopharmacol. 2007;27(2):182–187. doi: 10.1097/JCP.0b013e318032eadb. [DOI] [PubMed] [Google Scholar]
- 21.Menz HB, Lord SR, St George R, Fitzpatrick RC. Walking stability and sensorimotor function in older people with diabetic peripheral neuropathy. Arch Phys Med Rehabil. 2004;85(2):245–252. doi: 10.1016/j.apmr.2003.06.015. [DOI] [PubMed] [Google Scholar]
- 22.Richerson SJ, Robinson CJ, Shum J. A comparative study of reaction times between type II diabetics and non-diabetics. Biomed Eng Online. 2005;4(1):12. doi: 10.1186/1475-925X-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O’Neill WM, Hanks GW, Simpson P, Fallon MT, Jenkins E, Wesnes K. The cognitive and psychomotor effects of morphine in healthy subjects: a randomized controlled trial of repeated (four) oral doses of dextropropoxyphene, morphine, lorazepam and placebo. Pain. 2000;85(1–2):209–215. doi: 10.1016/s0304-3959(99)00274-2. [DOI] [PubMed] [Google Scholar]
- 24.Turner C, Handford AD, Nicholson AN. Sedation and memory: studies with a histamine H-1 receptor antagonist. J Psychopharmacol. 2006;20(4):506–17. doi: 10.1177/0269881106059804. [DOI] [PubMed] [Google Scholar]
- 25.Iverson GL, Lovell MR, Collins MW. Validity of ImPACT for measuring processing speed following sports-related concussion. J Clin Exp Neuropsychol. 2005;27(6):683–689. doi: 10.1081/13803390490918435. [DOI] [PubMed] [Google Scholar]
- 26.Collie A, Maruff P, Darby D, Makdissi M, McCrory P, McStephen M. CogSport. In: Echemendia RJ, editor. Sports Neuropsychology: A clincial primer. New York, NY: Guildford Publications; 2005. pp. 240–262. [Google Scholar]
- 27.Cernich A, Reeves D, Sun W, Bleiberg J. Automated Neuropsychological Assessment Metrics sports medicine battery. Arch Clin Neuropsychol. 2007;22:S101–S114. doi: 10.1016/j.acn.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 28.Guskiewicz KM, Bruce SL, Cantu RC, et al. National Athletic Trainers’ Association Position Statement: Management of Sport-Related Concussion. J Athl Train. 2004;39(3):280–297. [PMC free article] [PubMed] [Google Scholar]
- 29.McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on Concussion in Sport 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Clin J Sport Med. 2009;19(3):185–200. doi: 10.1097/JSM.0b013e3181a501db. [DOI] [PubMed] [Google Scholar]
- 30.Chudler EH. [Accessed December 13, 2010.];Neuroscience for Kids. 2007 Available at: http://faculty.washington.edu/chudler/chreflex.html.
- 31.Eckner JT, Whitacre RD, Kirsh NL, Richardson JK. Evaluating a Clinical Measure of Reaction Time: An Observational Study. Percept Mot Skills. 2009;108:717–720. doi: 10.2466/PMS.108.3.717-720. [DOI] [PubMed] [Google Scholar]
- 32.Eckner JT, Kutcher JS, Richardson JK. Pilot evaluation of a novel clinical test of reaction time in national collegiate athletic association division I football players. J Athl Train. 2010;45(4):327–32. doi: 10.4085/1062-6050-45.4.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eckner JT, Kutcher JS, Richardson JK. Between season test-retest reliability of clinically measured reaction time in NCAA Division I collegiate athletes. J Athl Train. doi: 10.4085/1062-6050-46.4.409. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eckner JT, Lipps DB, Kim H, Richardson JK, Ashton-Miller JA. Can A Clinical Test Of Reaction Time Predict A Functional Head-Protective Response? Med Sci Sports Exerc. 2011;43(3):382–387. doi: 10.1249/MSS.0b013e3181f1cc51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eckner JT, Kutcher JS, Richardson JK. Effect of concussion on clinically measured reaction time in nine NCAA Division I collegiate athletes: a preliminary study. PM&R. 2011;3:212–218. doi: 10.1016/j.pmrj.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bailey CM, Echemendia RJ, Arnett PA. The impact of motivation on neuropsychological performance in sports-related mild traumatic brain injury. J Int Neuropsychol Soc. 2006;12(4):475–484. doi: 10.1017/s1355617706060619. [DOI] [PubMed] [Google Scholar]
- 37.Crabtree DA, Antrim LR. Guidelines for measuring reaction time. Percept Mot Skills. 1988;66(2):363–370. doi: 10.2466/pms.1988.66.2.363. [DOI] [PubMed] [Google Scholar]
- 38.McCormack PD, Binding FR, McElheran WG. Effects on Reaction Time of Partial Knowledge of Results of Performance. Percept Mot Skills. 1963;17:279–281. doi: 10.2466/pms.1963.17.1.279. [DOI] [PubMed] [Google Scholar]
- 39.McCormack PD, McElheran WG. Follow-up Effects on Reaction Time with Partial Knowledge of Results. Percept Mot Skills. 1963;17:565–566. doi: 10.2466/pms.1963.17.2.565. [DOI] [PubMed] [Google Scholar]
- 40.Church RM, Camp DS. Change in Reaction-Time as a Function of Knowledge of Results. Am J Psychol. 1965;78:102–106. [PubMed] [Google Scholar]
- 41.McCormack PD, Binding FR, Chylinski J. Effects on reaction time of knowledge of results of performance. Percept Mot Skills. 1962;14:367–372. doi: 10.2466/pms.1963.17.1.279. [DOI] [PubMed] [Google Scholar]
- 42.Locke EA. Effects of knowledge of results, feedback in relation to standards, and goals on reaction-time performance. Am J Psychol. 1968;81(4):566–574. [PubMed] [Google Scholar]
- 43.Peretti P. Effects on reaction time of random false knowledge of results of performance. Percept Mot Skills. 1970;30:838. [Google Scholar]