Abstract
Objectives
To evaluate the effect of concussion on clinically-measured reaction time (RTclin) with comparison to a computerized reaction time measure (RTcomp).
Design
Prospective, repeated measures observational study.
Setting
Athletic training clinic at an NCAA Division I university.
Participants
Data are reported for 9 collegiate athletes with acute concussion who were part of a larger cohort of 209 athletes recruited from the university’s football, women’s soccer, and wrestling teams prior to the start of their respective athletic seasons.
Methods
Baseline RTclin and RTcomp were measured during pre-participation physical examinations. RTclin measured the time required to catch a suspended vertical shaft by hand closure after its release by the examiner. RTcomp was derived from the simple reaction time component of the CogState-Sport computerized neurocognitive test battery. Athletes who subsequently sustained a physician-diagnosed concussion underwent repeat RTclin and RTcomp testing within 72 hours of injury. A Wilcoxon signed rank test was used to compare baseline and after-injury reaction times.
Main Outcome Measurements
After-injury changes in RTclin and RTcomp calculated with respect to each athlete’s own pre-season baseline value.
Results
After-injury RTclin was prolonged in 8 of the 9 concussed athletes, while RTcomp was prolonged in 5 of the 9 concussed athletes. Mean RTclin increased from 193 ± 21 ms to 219 ± 31 ms (p = 0.050), and mean RTcomp increased from 247 ± 75 to 462 ± 120 ms (p = 0.214).
Conclusions
We conclude that RTclin appears to be sensitive to the known prolongation of reaction time following concussion, and compares favorably to an accepted computerized reaction time measure. This study supports the potential utility of RTclin as part of a multi-faceted concussion assessment battery.
INTRODUCTION
Sport related concussion is a common and serious injury. Recent estimates from the CDC are that approximately1.6 to 3.8 million sport associated traumatic brain injuries (TBI’s) occur annually in the United States, with the vast majority classified as mild TBI, or concussion [1]. Epidemiological studies have shown that concussion accounts for 5-10% of all injuries associated with organized sport participation at the high school and collegiate levels [2, 3]. Concussions were once considered minor injuries that an athlete could play through without consequence. However, an explosion in the number and quality of concussion research articles published in the scientific literature over the past 20 years coupled with a great deal of recent attention in the popular press have largely changed this attitude. Traumatic brain injury and the issue of determining the readiness of a concussed athlete to return to sport participation are now considered major public health issues [4, 5]. The appropriate diagnosis and management of concussed athletes remains of primary importance in minimizing the short-term effects of injury on an athlete and preventing poor outcomes that can result from premature return to sport participation. In addition, there has recently been increasing attention focused on the potential long term effects repeat or mismanaged concussions can have on athletes later in life [6-8].
With these considerations in mind, it is of clear importance that sports medicine providers be able to properly diagnose and manage these injuries. A significant challenge faced by physicians and the other sports medicine providers who evaluate concussed athletes is that there is no single diagnostic test for concussion. Given the heterogeneous nature of this injury, a multi-faceted approach to assessment is essential. All recently published concussion management guidelines appropriately emphasize the value of such a multi-faceted approach [9-11]. The concussion evaluation should assess the presence and severity of typical concussive symptoms and neurological signs including balance and cognition. Standardized assessment tools can be helpful as they allow for comparison of a concussed athlete’s after-injury performance to their own pre-season baseline. One form of standardized assessment tool that has been growing in popularity among the sports medicine community for this purpose is the computerized cognitive assessment battery. While numerous computerized test programs exist [12-14], all share several features, one of which is the ability to assess reaction time (RT).
Impaired RT is one of the most common cognitive sequelae of concussion. It represents one of the most sensitive indices of cognitive change following concussion [15, 16] and has been shown to have prognostic value in predicting time to recovery [17]. Reaction time is typically prolonged immediately after injury with a gradual return back to baseline during the recovery period [18-24]. Impaired RT generally parallels the presence of other self-reported concussion symptoms [18, 22, 25, 26], but in some athletes RT remains impaired even after the athlete has become asymptomatic [21, 23, 27]. Therefore, RT assessment is an important component of the sports medicine provider’s concussion assessment battery that can increase the sensitivity of the clinical examination for detecting the effects of sport related concussion. In addition to its importance as a sign of concussion, impaired RT has functional relevance given that a rapid RT is necessary for injury avoidance. Unfortunately, the dependence of current RT assessment tools on a computer platform running specialized software limits their utility as a sideline assessment tool and makes them inaccessible to many youth athletes who play in leagues with limited financial resources.
To broaden the availability of RT measurement, we developed a simple visuo-motor RT test that can be used on the sideline or in the athletic training clinic. In pilot work this clinical measure of RT (RTclin) was reliable and valid with comparable stability from season to season to reaction time measures currently included in computerized cognitive assessment batteries [28-30]. We have also shown functional relevance of RTclin, as it is highly correlated with the ability to quickly raise the hands to protect the head in a simulated sport environment [31]. This study’s primary aim was to determine the effect of concussion on RTclin by comparing pre-season RTclin to RTclin after sport related concussion. A secondary aim was to compare the effect of concussion on RTclin to its effect on an accepted and validated computerized measure of RT (RTcomp).
METHODS
Subjects
We recruited 209 student-athletes at a single university during pre-participation physical examinations over 2 seasons. Members of the football, women’s soccer, and wrestling teams who were at least 18 years of age at the time of their pre-participation examination were eligible to participate. Athletes were excluded if they were recovering from an acute concussion or an upper extremity injury that would prevent them from completing the RTclin task. Each athlete provided informed written consent approved by the IRB at the authors’ institution before completing baseline RTclin and RTcomp assessments.
Data Collection
The RTclin test protocol used has been previously described [28, 29]. In brief, athletes sat with their forearm resting on a desk surface with their hand at the edge such that it was held sufficiently open to fit around, but not touch, the weighted disk portion of the RTclin apparatus (Figure 1a). The apparatus is a rigid 80cm cylinder coated in high-friction tape, marked in ½ cm increments, and affixed to a weighted disk at one end. The examiner vertically suspended the device with the top of the weighted disk aligned with the superior-most aspect of the athlete’s open hand. The examiner released the apparatus after randomly determined delay intervals between 2 and 5 seconds to prevent the athlete from anticipating its time of release. Upon release, the athlete caught the device as rapidly as possible by hand closure (Figure 1b). The distance (in cm) the apparatus fell before being caught by the athlete was recorded and used to calculate RTclin (in ms) for each trial using the formula for a body falling under the influence of gravity (d = ½ gt2). Each athlete performed 2 practice trials, followed by 8 data acquisition trials. Mean (SD) baseline RTclin values were calculated for each athlete.
Figure 1.
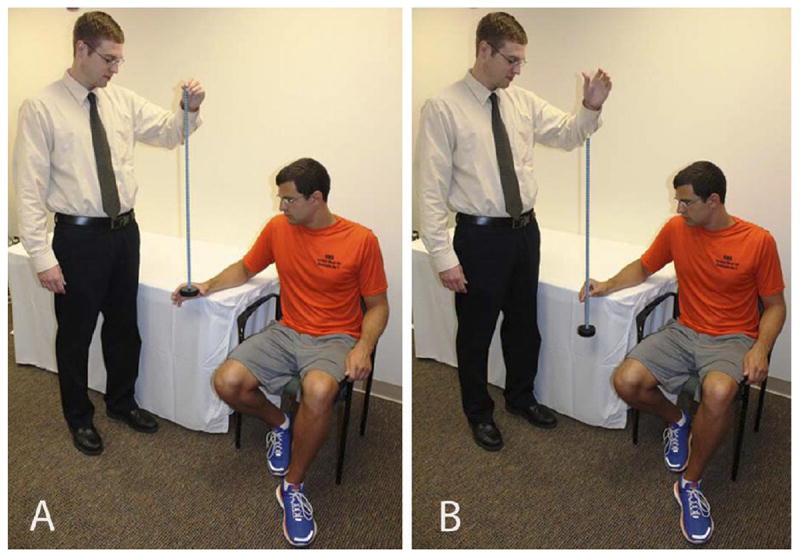
The clinical reaction time procedure. (a) Demonstration of the starting athlete and tester positioning. (b) Demonstration of the post-drop athlete and tester positioning.
RTcomp was derived from each athlete’s performance on the simple reaction time component of CogState-Sport (Version 5.6.4. Melbourne, Australia: CogState, Ltd.) as previously described [28]. CogState-Sport is a computerized neurocognitive assessment battery composed of 4 tasks assessing simple reaction time, choice reaction time, learning, and working memory. CogState-Sport also includes a brief self-reported concussion history and concussion symptom assessment using the Sideline Concussion Assessment Tool (SCAT) [32]. CogState-Sport’s repeatability [16, 33] and sensitivity to the cognitive effects of sport-related concussion [18] are well described in the literature, and the program has been generally accepted by the sports medicine community for use as a concussion assessment tool. The CogState-Sport program performs a series of integrity checks on each test aimed at detecting poor effort or understanding of the test protocol on the part of the test-taker in an effort to ensure valid baseline to after-injury comparisons. The simple reaction time component of the test battery requires the athlete to depress a computer key as rapidly as possible in response to a playing card displayed on the monitor turning face-up. Mean (SD) baseline RTcomp values (in ms) were calculated for each athlete from their raw CogState-Sport simple reaction time data.
During the 2-year study period, 9 student-athletes sustained a physician-diagnosed concussion and repeated RTclin and RTcomp assessments within 72 hours of injury. The after-injury RTclin and RTcomp tests were performed using an identical protocol to that used for baseline testing. Mean (SD) after-injury RTclin and RTcomp values (in ms) were again calculated, as were the changes in RTclin and RTcomp as compared to each athlete’s own pre-season baseline value. Change scores were calculated as after-injury value minus baseline value, such that decline is represented by a positive value and improvement is represented by a negative value.
Statistical Analysis
Given the small sample size, a Wilcoxon signed rank test was used to compare baseline and after-injury reaction time test performances. Effect sizes for RTclin and RTcomp were described using Cohen’s d. While the small sample size precluded any formal sub-group analyses, changes in RTclin and RTcomp were descriptively compared or plotted based on prior history of concussion, presence or absence of loss of consciousness and post-traumatic amnesia, and concussion symptom scores using the total SCAT post-concussion symptom score as well as the “feeling slowed down” SCAT sub-score.
RESULTS
Demographics, concussion histories, basic injury characteristics, and SCAT scores at the time of after-injury assessment for the 9 concussed athletes are presented in Table 1. As compared to their own baseline results, after-injury RTclin and RTcomp values were prolonged in 8 (89%) and 5 (56%) of the 9 concussed athletes, respectively (Table 2). On average, RTclin was 26 ms slower after concussion (p = 0.050) and RTcomp was 215 ms slower (p = 0.214). The effect sizes for RTclin and RTcomp were 1.03 and 2.20, respectively.
Table 1.
Concussion history and injury characteristics for the 9 concussed athletes.
| Athlete number |
Sport* | Age, Gender |
Prior concussions |
Loss of consciousness |
PTA | SCAT: slowed down score** |
SCAT: total score*** |
|---|---|---|---|---|---|---|---|
| 1 | FB | 22 M | 1 | Yes | No | 1 | 22 |
| 2 | SOC | 20 F | 2 | No | No | 2 | 26 |
| 3 | FB | 20 M | 0 | No | Yes | 2 | 24 |
| 4 | FB | 19 M | 0 | No | No | 4 | 25 |
| 5 | FB | 20 M | 0 | No | No | 1 | 31 |
| 6 | FB | 20 M | 2 | No | No | 3 | 62 |
| 7 | FB | 21 M | 0 | No | No | 2 | 34 |
| 8 | FB | 22 M | 3 | No | Yes | 6 | 111 |
| 9 | FB | 21 M | 1 | No | Yes | 2 | 26 |
FB = American football, SOC = soccer.
Each post-concussion SCAT symptom is graded on a 0-6 scale with 0 representing absence of a symptom and scores of 1-6 representing mild-severe presence of a symptom.
The SCAT Post-concussion symptom scale is composed of 24 symptoms and therefore has a possible range from 0-144.
Table 2.
RTclin and RTcomp summary data for the 9 concussed athletes. Mean (SD) in ms.
| Athlete number |
Baseline RTclin |
After-injury RTclin |
Δ RTclin |
Baseline RTcomp |
After-injury RTcomp |
Δ RTcomp |
|---|---|---|---|---|---|---|
| 1 | 180 (15) | 204 (20) | 24 | 275 (80) | 260 (39) | -15 |
| 2 | 195 (20) | 228 (25) | 33 | 256 (50) | 1128 (360) | 872 |
| 3 | 182 (22) | 200 (31) | 18 | 224 (28) | 248 (36) | 24 |
| 4 | 208 (21) | 238 (23) | 30 | 198 (36) | 317 (135) | 119 |
| 5 | 217 (24) | 186 (46) | -31 | 274 (212) | 248 (37) | -26 |
| 6 | 200 (32) | 218 (38) | 18 | 301 (137) | 285 (69) | -16 |
| 7 | 204 (14) | 251 (17) | 47 | 209 (23) * | 229 (30) | 20 |
| 8 | 156 (15) | 249 (34) | 93 | 220 (54) | 1189 (324) | 969 |
| 9 | 191 (29) | 201 (43) | 10 | 263 (57) | 257 (51) | -6 |
| Average | 193 (21) | 219 (31) | 26 | 247 (75) | 462 (120) | 215 |
Athlete #7 did not have a valid baseline test session from the season of injury, so the prior year’s baseline was used.
There appears to be a trend of greater after-injury change in RTclin in those athletes who have had more prior concussions as compared to those who have not, however no similar trend is apparent for RTcomp (Table 3a). The changes in RTclin and RTcomp in the athlete whose concussion was associated with loss of consciousness do not appear to differ from those of the other 8 athletes (Table 3b). There does appear to be a trend toward greater after-injury change in RTclin and RTcomp in the 3 athletes whose concussions were associated with post-traumatic amnesia as compared to the 6 athletes whose injuries were not (Table 3c). When changes in RTclin and RTcomp are plotted against total SCAT post-concussion symptom scores and the “feeling slowed down” SCAT sub-score, the only apparent trend is between RTclin and the “feeling slowed down” SCAT sub-score (Figure 2).
Table 3.
After-injury changes in RTclin and RTcomp in subgroups of athletes based on prior concussion history (a), presence of loss of consciousness (b), and presence of post-traumatic amnesia (c).
| Athlete subgroup | n | Δ RTclin (ms) | Δ RTcomp (ms) | |
|---|---|---|---|---|
| a. Prior concussions | 0 | 4 | 16 | 34 |
| 1 | 2 | 17 | -11 | |
| 2 | 2 | 26 | 428 | |
| 3 | 1 | 93 | 969 | |
| b. LOC* | Yes | 1 | 24 | -15 |
| No | 8 | 27 | 245 | |
| c. PTA** | Yes | 3 | 40 | 329 |
| No | 6 | 20 | 159 | |
Loss of consciousness
Post-traumatic amnesia
Figure 2.
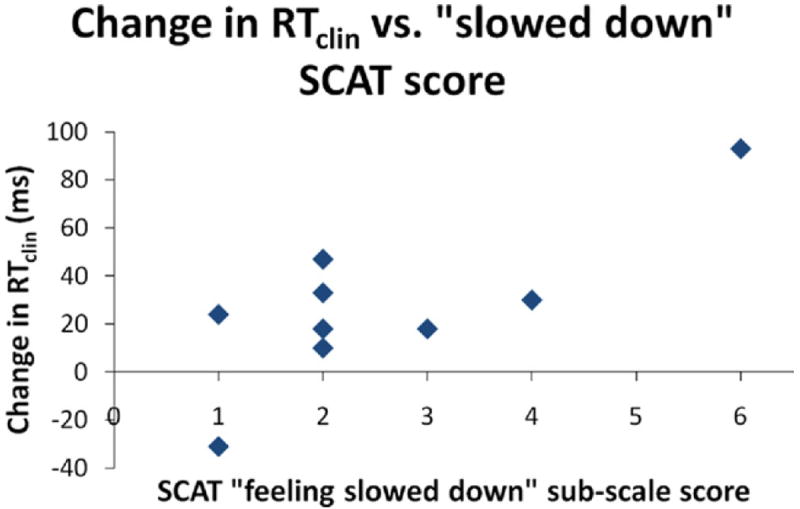
Plot illustrating the relationship between after-injury change in RTclin and the athlete’s self-reported rating of “feeling slowed down” on the SCAT at the time of after-injury testing.
DISCUSSION
This study’s primary aim was to determine the effect of concussion on RTclin. In this sample of 9 concussed athletes, RTclin was, on average, 13.5% slower after injury as compared to the athlete’s own preseason baseline. The associated effect size of 1.03, which represents the magnitude of the difference between the athletes’ baseline and after-injury RTclin performances proportional to the variability in RTclin, is generally considered to be large [34]. Only 1 of the concussed athletes demonstrated a faster RTclin after injury. Given that this athlete was also faster on RTcomp after injury, it is possible that this particular concussion did not cause a slowed reaction time. While concussions do typically result in slower reaction times, every concussion is unique and this phenomenon is not universal. Consistent with this, the athlete rated the subjective symptom of “feeling slowed down” as a 1 on his after-injury SCAT suggesting that he perceived minimal psychomotor slowing. An alternative explanation is that this athlete did not perform optimally during his baseline test sessions, a possibility supported by the observation that his baseline RTclin and RTcomp values were both among the slowest in our sample. Overall, these findings suggest that RTclin is, in fact, sensitive to the expected prolongation of RT following concussion.
A secondary study aim was to contrast the effect of concussion on RTclin and RTcomp. Although RTclin was more frequently prolonged than RTcomp, the average magnitude of change was greater for RTcomp, as was its variability. This effect was driven by two athletes whose after-injury RTcomp values were highly variable and very slow. Both of these athletes failed at least one of the CogState-Sport integrity checks during these after-injury evaluations and close inspection of the full reports for these test sessions reveals that their performance was very slow throughout all 4 of the CogState-Sport test modules. These findings are unlikely to be entirely attributable to cognitive slowing as a result of the athletes’ concussions. One possible explanation is distraction due to headache or some other post-concussion symptom. Another possible explanation is poor motivation due to the fact that the athletes already recognized that they had sustained a concussion and would not be immediately cleared to return to play regardless of their performance on that particular after-injury test. We do not believe that these athletes had any problem understanding the computerized test procedure because both had completed valid baseline tests at the beginning of the season during which they sustained their concussions. It is interesting to note that, although both of these athletes did have slower post-concussion RTclin performances, the magnitude of slowing is much smaller for RTclin than for RTcomp. Potential reasons for this difference include the fact that RTclin is bound by a maximum value of approximately 400 ms, the amount of time that elapses between release of the device and contact with the ground, while RTcomp has no upper limit. Also, athletes may more consistently attend to RTclin testing because it involves direct interaction between the athlete and the examiner, is an intrinsically more interesting task, and lasts only 3-5 minutes. In contrast, RTcomp testing does not involve human interaction, requires a more mundane task (pressing a computer keyboard key), and is part of a longer 15 minute test battery.
While no definitive inferences can be drawn from sub-group analysis of this small sample of concussed athletes, 3 interesting trends are noted. First, the magnitude of after-injury change in RTclin appears to increase as an athlete’s number of prior concussions increases. Prior studies, including our own previous work using RTclin, have failed to identify a relationship between an athlete’s prior concussion history and baseline RT measures [28, 35] or after-injury change in RT [36]; however, a prior history of 2 or more concussions has been associated with slower recovery of RT impairment following sport related concussion [37].
Second, the after-injury changes in both RTclin and RTcomp appear to be greater in the sub-set of athletes who experienced post-traumatic amnesia as compared to those who did not. Although we are unaware of any studies directly comparing presence or duration of post traumatic amnesia with after-injury changes in RT, this finding is noteworthy as previous studies have identified an association between post-traumatic amnesia and various concussion severity outcome measures [25, 38-41], Third, as illustrated in Figure 2, there appears to be a positive relationship between the concussed athlete’s subjective rating of “feeling slowed down” and their after-injury change in RTclin. If these apparent trends can be replicated in a larger sample of athletes with sport-related concussion, then these findings would further support the face and construct validity of RTclin.
The results of this preliminary RTclin study are consistent with existing literature reporting the detrimental short term effects of sport related concussion on computer-based RT measures. For example, Makdissi et al. [20] reported CogSport-based data obtained within 3 days of concussion in a series of 6 male Australian Rules football players showing an average increase in simple RT from 292.4 ± 88.6 ms at baseline to 339.9 ± 128.7 ms after injury. Similarly, Warden et al. [21] reported ANAM (Automated Neuropsychological Assessment Metrics)-based data at baseline and 4 days post-boxing concussion in 14 male military cadets that demonstrated an average increase in simple RT from 254 ± 33 ms to 342 ± 36 ms. Larger studies have reported similar trends in short term computerized RT performance using composite or throughput scores. Examples are McClincy et al. [2006], who reported impaired ImPACT (Immediate Post-Concussion Assessment and Cognitive Test) RT composite scores in 104 high school and collegiate athletes at 2 days and 1 week following concussion, with return to baseline 2 weeks after injury, and McCrea et al. [22], who reported impaired ANAM RT throughput scores in 28 high school and collegiate football players immediately following concussion, with a return to baseline when tested at post-injury days 8 and 45. While this format of data presentation does not permit direct comparison with our RTclin results, these findings are consistent with the trend of impaired RTclin performance in our sample of athletes in the days immediately following concussion.
This was a small, unblinded study and these are potential sources of bias. Therefore a larger, blinded study is necessary before firm conclusions are drawn. Follow-up studies should more precisely standardize the timing of after-injury testing and should test at multiple post-injury time points to monitor trends in RTclin performance during recovery. In addition, non-concussed athletes need to be tested concurrently to control for the effects of post-competition fatigue and non-concussion-inducing head contact. Despite the absence of control data, it is reasonable to hypothesize that repeated RTclin testing in uninjured athletes would result in faster RT’s given other work showing that baseline RTclin significantly decreased (became faster) by 11 ms in 102 uninjured college athletes over two seasons [30].
We do not propose that RTclin should replace computerized testing in athletes who have access to it, but rather that RTclin may complement computerized tests. However, should further work continue to support the sensitivity of RTclin to concussion, then its simplicity, portability, and low cost all represent advantages over computerized test batteries. These advantages may allow RTclin to serve as a true sideline tool during the initial evaluation of an athlete with suspected concussion, a setting in which computerized testing is impractical.
These attributes should also make RTclin available to a broader population of athletes, particularly youth athletes who sustain the majority of concussions [42] but usually have limited financial resources. Used with other clinical concussion assessment tools, RTclin has the potential to become a useful part of the sports medicine practitioner’s multi-faceted concussion assessment battery.
Contributor Information
James T. Eckner, Department of Physical Medicine and Rehabilitation, University of Michigan.
Jeffrey S. Kutcher, Department of Neurology, University of Michigan.
James K Richardson, Department of Physical Medicine and Rehabilitation, University of Michigan.
References
- 1.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–378. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Powell JW, Barber-Foss KD. Traumatic brain injury in high school athletes. JAMA. 1999;282(10):958–963. doi: 10.1001/jama.282.10.958. [DOI] [PubMed] [Google Scholar]
- 3.Gessel LM, Fields SK, Collins CL, Dick RW, Comstock RD. Concussions among United States high school and collegiate athletes. J Athl Train. 2007;42(4):495–503. [PMC free article] [PubMed] [Google Scholar]
- 4.Collins MW, Lovell MR, McKeag DB. Current issues in managing sports-related concussion. JAMA. 1999;282(24):2283–2285. doi: 10.1001/jama.282.24.2283. [DOI] [PubMed] [Google Scholar]
- 5.Kelly JP. Traumatic brain injury and concussion in sports. JAMA. 1999;282(10):989–991. doi: 10.1001/jama.282.10.989. [DOI] [PubMed] [Google Scholar]
- 6.McKee AC, Cantu RC, Nowinski CJ, et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol. 2009;68(7):709–735. doi: 10.1097/NEN.0b013e3181a9d503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gavett BE, Stern RA, Cantu RC, Nowinski CJ, McKee AC. Mild traumatic brain injury: a risk factor for neurodegeneration. Alzheimers Res Ther. 2010;2(3):18. doi: 10.1186/alzrt42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Beaumont L, Theoret H, Mongeon D, et al. Brain function decline in healthy retired athletes who sustained their last sports concussion in early adulthood. Brain. 2009;132:695–708. doi: 10.1093/brain/awn347. [DOI] [PubMed] [Google Scholar]
- 9.Guskiewicz KM, Bruce SL, Cantu RC, et al. National Athletic Trainers’ Association Position Statement: Management of Sport-Related Concussion. J Athl Train. 2004;39(3):280–297. [PMC free article] [PubMed] [Google Scholar]
- 10.McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on Concussion in Sport 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Clin J Sport Med. 2009;19(3):185–200. doi: 10.1097/JSM.0b013e3181a501db. [DOI] [PubMed] [Google Scholar]
- 11.Halstead ME, Walter KD. American Academy of Pediatrics. Clinical report--sport-related concussion in children and adolescents. Pediatrics. 2010;126(3):597–615. doi: 10.1542/peds.2010-2005. [DOI] [PubMed] [Google Scholar]
- 12.Iverson GL, Lovell MR, Collins MW. Validity of ImPACT for measuring processing speed following sports-related concussion. J Clin Exp Neuropsychol. 2005;27(6):683–689. doi: 10.1081/13803390490918435. [DOI] [PubMed] [Google Scholar]
- 13.Collie A, Maruff P, Darby D, Makdissi M, McCrory P, McStephen M. CogSport. In: Echemendia RJ, editor. Sports Neuropsychology: Assessment and Management of Traumatic Brain Injury. New York, NY: Guildford Publications; 2006. pp. 240–262. [Google Scholar]
- 14.Cernich A, Reeves D, Sun W, Bleiberg J. Automated Neuropsychological Assessment Metrics sports medicine battery. Arch Clin Neuropsychol. 2007;22:S101–S114. doi: 10.1016/j.acn.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 15.Erlanger D, Saliba E, Barth J, Almquist J, Webright W, Freeman J. Monitoring Resolution of Postconcussion Symptoms in Athletes: Preliminary Results of a Web-Based Neuropsychological Test Protocol. J Athl Train. 2001;36(3):280–287. [PMC free article] [PubMed] [Google Scholar]
- 16.Collie A, Maruff P, Makdissi M, McCrory P, McStephen M, Darby D. CogSport: reliability and correlation with conventional cognitive tests used in postconcussion medical evaluations. Clin J Sport Med. 2003;13(1):28–32. doi: 10.1097/00042752-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Lau B, Lovell MR, Collins MW, Pardini J. Neurocognitive and symptom predictors of recovery in high school athletes. Clin J Sport Med. 2009;19(3):216–221. doi: 10.1097/JSM.0b013e31819d6edb. [DOI] [PubMed] [Google Scholar]
- 18.Collie A, Makdissi M, Maruff P, Bennell K, McCrory P. Cognition in the days following concussion: comparison of symptomatic versus asymptomatic athletes. J Neurol Neurosurg Psychiatry. 2006;77(2):241–245. doi: 10.1136/jnnp.2005.073155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lovell MR, Collins MS, Fu FH, et al. Neuropsychological testing in sports: Past, present, and future. Br J Sports Med. 2001;35:373. [Google Scholar]
- 20.Makdissi M, Collie A, Maruff P, et al. Computerised cognitive assessment of concussed Australian Rules footballers. Br J Sports Med. 2001;35(5):354–360. doi: 10.1136/bjsm.35.5.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Warden DL, Bleiberg J, Cameron KL, et al. Persistent prolongation of simple reaction time in sports concussion. Neurology. 2001;57(3):524–526. doi: 10.1212/wnl.57.3.524. [DOI] [PubMed] [Google Scholar]
- 22.McCrea M, Prichep L, Powell MR, Chabot R, Barr WB. Acute effects and recovery after sport-related concussion: a neurocognitive and quantitative brain electrical activity study. J Head Trauma Rehabil. 2010;25(4):283–292. doi: 10.1097/HTR.0b013e3181e67923. [DOI] [PubMed] [Google Scholar]
- 23.Makdissi M, Darby D, Maruff P, Ugoni A, Brukner P, McCrory PR. Natural history of concussion in sport: markers of severity and implications for management. Am J Sports Med. 2010;38(3):464–471. doi: 10.1177/0363546509349491. [DOI] [PubMed] [Google Scholar]
- 24.McClincy MP, Lovell MR, Pardini J, Collins MW, Spore MK. Recovery from sports concussion in high school and collegiate athletes. Brain Inj. 2006;20(1):33–39. doi: 10.1080/02699050500309817. [DOI] [PubMed] [Google Scholar]
- 25.Collins MW, Field M, Lovell MR, et al. Relationship between postconcussion headache and neuropsychological test performance in high school athletes. Am J Sports Med. 2003;31(2):168–173. doi: 10.1177/03635465030310020301. [DOI] [PubMed] [Google Scholar]
- 26.Broglio SP, Sosnoff JJ, Ferrara MS. The relationship of athlete-reported concussion symptoms and objective measures of neurocognitive function and postural control. Clin J Sport Med. 2009;19(5):377–382. doi: 10.1097/JSM.0b013e3181b625fe. [DOI] [PubMed] [Google Scholar]
- 27.Broglio SP, Macciocchi SN, Ferrara MS. Neurocognitive performance of concussed athletes when symptom free. J Athl Train. 2007;42(4):504–508. [PMC free article] [PubMed] [Google Scholar]
- 28.Eckner JT, Kutcher JS, Richardson JK. Pilot evaluation of a novel clinical test of reaction time in National Collegiate Athletic Association Division I football players. J Athl Train. 2010;45(4):327–332. doi: 10.4085/1062-6050-45.4.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eckner JT, Whitacre RD, Kirsch NK, Richardson JK. Evaluating a clinical measure of reaction time: an observational study. Percept Mot Skills. 2009;108:717–720. doi: 10.2466/PMS.108.3.717-720. [DOI] [PubMed] [Google Scholar]
- 30.Eckner JT, Kutcher JS, Richardson JK. Between season test-retest reliability of clinically measured reaction time in NCAA Division I collegiate athletes. J Athl Train. 2011 doi: 10.4085/1062-6050-46.4.409. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eckner JT, Lipps DB, Kim H, Richardson JK, Ashton-Miller JA. Can a clinical test of reaction time predict a functional head-protective response? Med Sci Sports Exerc. 2011 doi: 10.1249/MSS.0b013e3181f1cc51. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McCrory P, Johnston K, Meeuwisse W, et al. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004. Br J Sports Med. 2005;39(4):196–204. doi: 10.1136/bjsm.2005.018614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Collie A, Maruff P, Darby DG, McStephen M. The effects of practice on the cognitive test performance of neurologically normal individuals assessed at brief test-retest intervals. J Int Neuropsychol Soc. 2003;9(3):419–428. doi: 10.1017/S1355617703930074. [DOI] [PubMed] [Google Scholar]
- 34.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1988. [Google Scholar]
- 35.Covassin T, Elbin R, Kontos A, Larson E. Investigating baseline neurocognitive performance between male and female athletes with a history of multiple concussion. J Neurol Neurosurg Psychiatry. 2010;81(6):597–601. doi: 10.1136/jnnp.2009.193797. [DOI] [PubMed] [Google Scholar]
- 36.Iverson GL, Gaetz M, Lovell MR, Collins MW. Cumulative effects of concussion in amateur athletes. Brain Inj. 2004;18(5):433–443. doi: 10.1080/02699050310001617352. [DOI] [PubMed] [Google Scholar]
- 37.Covassin T, Stearne D, Elbin R. Concussion history and postconcussion neurocognitive performance and symptoms in collegiate athletes. J Athl Train. 2008;43(2):119–124. doi: 10.4085/1062-6050-43.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McCrea M, Kelly JP, Randolph C, Cisler R, Berger L. Immediate neurocognitive effects of concussion. Neurosurgery. 2002;50(5):1032–1040. doi: 10.1097/00006123-200205000-00017. [DOI] [PubMed] [Google Scholar]
- 39.Pellman EJ, Viano DC, Casson IR, Arfken C, Powell J. Concussion in professional football: injuries involving 7 or more days out--Part 5. Neurosurgery. 2004;55(5):1100–1119. doi: 10.1227/01.neu.0000147063.12873.f5. [DOI] [PubMed] [Google Scholar]
- 40.Collins MW, Iverson GL, Lovell MR, McKeag DB, Norwig J, Maroon J. On-field predictors of neuropsychological and symptom deficit following sports-related concussion. Clin J Sport Med. 2003;13(4):222–229. doi: 10.1097/00042752-200307000-00005. [DOI] [PubMed] [Google Scholar]
- 41.Lovell MR, Collins MW, Iverson GL, et al. Recovery from mild concussion in high school athletes. J Neurosurg. 2003;98(2):296–301. doi: 10.3171/jns.2003.98.2.0296. [DOI] [PubMed] [Google Scholar]
- 42.CDC. Nonfatal traumatic brain injuries from sports and recreation activities--United States, 2001-2005. Morb Mortal Wkly Rep. 2007;56(29):733–737. [PubMed] [Google Scholar]


