Abstract
Background
The etiology of chronic fatigue syndrome (CFS) remains unknown. Personality traits influence well-being and may play a role in CFS and unexplained chronic fatigue.
Purpose
To examine the association of emotional instability and extraversion with chronic fatigue and CFS in a genetically informative sample.
Methods
We evaluated 245 twin pairs for two definitions of chronic fatigue. They completed the Neuroticism and Extraversion subscales of the NEO-FFI. Using a co-twin control design, we examined the association between personality and chronic fatigue.
Results
Higher emotional instability was associated with both definitions of chronic fatigue and was confounded by shared genetics. Lower extraversion was also associated with both definitions of fatigue, but was not confounded by familial factors.
Conclusions
Both emotional instability and extraversion are related to chronic fatigue and CFS. Whereas emotional instability and chronic fatigue are linked by shared genetic mechanisms, the relationship with extraversion may be causal and bi-directional.
Keywords: chronic fatigue, personality, extraversion, neuroticism, twin, genetic
INTRODUCTION
Chronic fatigue syndrome (CFS) is one of several medically unexplained conditions that challenge contemporary understandings of health and disease. Developed in 1994 by a Centers for Disease Control and Prevention (CDC) study group, the current case definition of CFS (1) requires the presence of debilitating fatigue for at least six months that interferes substantially with normal activity levels and is not better accounted for by another known illness or condition. In addition, fatigue must be accompanied during a six-month period by at least four of the following secondary symptoms: impaired memory or concentration, sore throat, tender glands, aching or stiff muscles, multi-joint pain, new headaches, unrefreshing sleep, and post-exertional fatigue. Finally, clinical examination, including history, physical examination, mental status examination, and laboratory testing must rule out other causes of fatigue, including but not limited to clinical depression, eating disorders, substance abuse, and side effects of medication (1). There is no objective test or marker for CFS.
Several other clinical phenotypes are relevant to the range of fatiguing illness and are often studied in relation to CFS. By common consent, chronic fatigue involves the presence of unexplained fatigue for six months or longer, and is one of the main defining characteristics of CFS. Chronic impairing fatigue additionally stipulates impairment in functioning. CFS-like illness involves the same presence of fatigue, secondary symptoms, and absence of exclusionary conditions required by the CDC-based diagnosis of CFS, and is often used in lieu of CFS in epidemiological studies that have logistical barriers to the clinical examination requirement. The boundaries between these non-mutually-exclusive definitions of fatiguing illness are to some degree arbitrary (2, 3), but they have consistently been studied together or conceptualized as the range of fatiguing illness. For example, a CDC-conducted, community-based survey of 14 627 adults found a 1.8% point prevalence of unexplained chronic fatigue and a 0.2% prevalence of CFS-like illness (4), which are consistent with estimates of the prevalence of CFS from 0.007% to 0.56% in community samples and from 0.3% to 2.6% in primary care settings. Despite decades of research, the etiology and pathophysiology of the conditions along this continuum of chronic fatigue remain unknown. While earlier research focused on determining whether the etiology of unexplained chronic fatigue and CFS was primarily physical (especially virologic) or psychological in nature, current thinking is that CFS is likely a complex condition with multiple predisposing and perpetuating factors. In fact, a pure dichotomy between an illness with a specific pathophysiology and one with important psychological aspects is neither necessary nor especially likely (5). Given advances in understanding the reciprocal relationship between psychological distress and physiological functioning—that is, understanding how stress “gets under the skin”—a simple physical or psychological explanation of CFS appears unlikely (6-8). Moreover, Wessely (9, 10), Greenberg (11), and others have presented a strong argument that a single model, either medical or psychiatric, is insufficient to understand CFS.
In pursuit of a multidisciplinary understanding of CFS, one important area of research has been the relationship between personality factors and the development and maintenance of CFS. Personality refers to stable trait-like patterns of perceiving and relating to oneself and one’s environment. Well-validated personality traits are relatively stable over time, are expressed in a wide range of personal and social contexts, and have consistent influences on behavior. The Five Factor Model (or “The Big Five”) has emerged as the most empirically validated and robust model to describe personality and its relationship to health and behavior (12). The Five Factor Model comprises the five dimensions of emotional instability, extraversion, agreeableness, conscientiousness, and openness.
Emotional instability is also known as “neuroticism” (13) and defined by Costa and McCrae as “a broad dimension of individual differences in the tendency to experience negative, distressing emotions and to possess associated behavioral and cognitive traits. Among the traits that define this dimension are fearfulness, irritability, low self-esteem, social anxiety, poor inhibition of impulses, and helplessness” (14). Vulnerability to stress is also a facet, or subscale, of the neuroticism domain (13).
High emotional instability has been associated with CFS in a variety of studies (15-21). Of particular importance for the present study, in a large population-based, longitudinal, co-twin control analysis, Kato and colleagues (22) found that emotional instability, assessed 25 years earlier, predicted chronic impairing fatigue and CFS-like illness through non-causal shared genetic mechanisms common to both emotional instability and fatiguing illness. For each standard deviation increase in emotional instability the risk for chronic impairing fatigue and for CFS-like illness increased 55% and 72%, respectively, after correction for stress and extraversion. According to these data, emotional instability does not cause CFS nor does CFS cause emotional instability. Rather, both arise in at-risk individuals through a common, underlying genetic mechanism. Another set of analyses of the same twin sample linked high levels of emotional instability to increased likelihood of developing a variety of physical and psychological conditions, including CFS, arthritis, cardiovascular disease, ulcers, headaches, and chronic widespread pain (23).
Extraversion is defined as tendencies toward interpersonal warmth, gregariousness, assertiveness, activity, excitement-seeking, and positive emotion. Extraverts are predisposed to experience positive emotions and show a higher degree of social activity (13). Evidence also indicates a positive association between extraversion and healthy exercise behavior, whereas neuroticism has a negative association (24-26). Several studies have noted low extraversion in patients with CFS (16) and fibromyalgia (20, 27), but these findings have not been consistent (28). In addition, Masuda and colleagues found higher levels of extraversion in post-infectious but not non-infectious CFS patients (21). The longitudinal co-twin control study described above found no association between extraversion at baseline and chronic fatigue 25 years later, after adjusting for emotional instability (22).
Even with these mixed results, extraversion is a potentially important factor in understanding how CFS develops and is sustained in individuals, because extraversion correlates with subjective well-being (29-32), and guiding a person to act in a more extraverted manner can increase subjective well-being (33). Such an effect, along with the positive effects of extraversion on exercise behavior (24-26), may explain some of the benefits of cognitive behavioral and graded exercise therapies in CFS (34-36). That is, acting in an extraverted way may have a “navigational effect” that positively alters the daily experience of fatigue, pain, and associated negative mood states described by people with CFS.
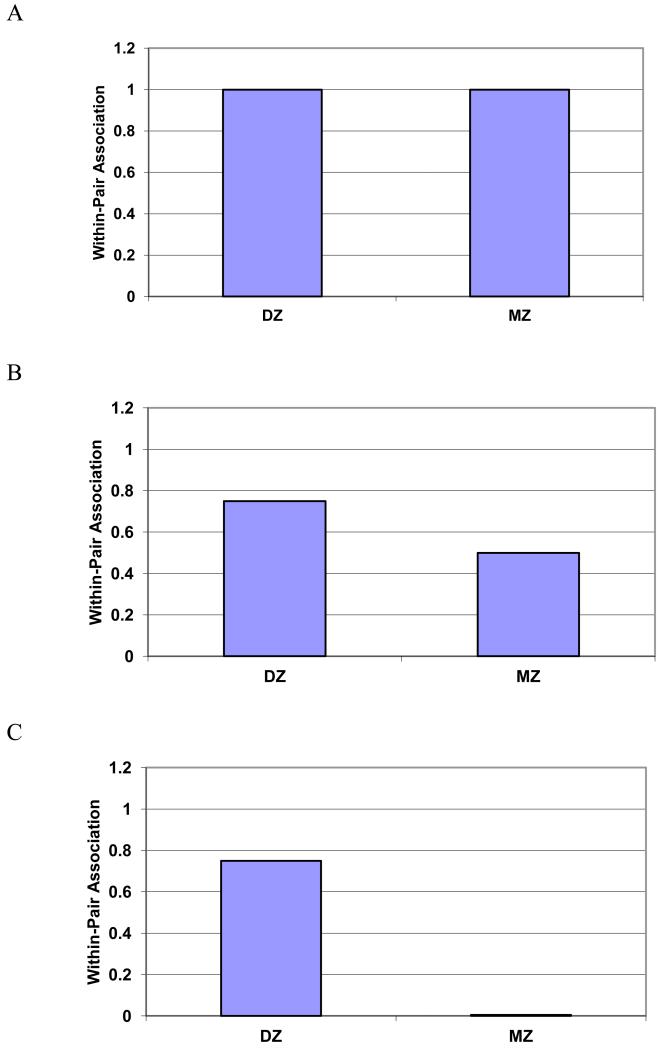
Twins are especially helpful in the study of conditions of unknown cause and disorders for which appropriate comparison groups are ill-defined. Because of the excellent match between twins for critical confounders such as genes and childhood environment, co-twin studies provide the best matched controls in a case-control study. A co-twin design is therefore one of the most sensitive approaches to assessing the association of subtle clinical measurements, such as personality traits, with a specific condition, such as CFS. Because monozygotic (MZ) twins who are reared together share 100% of their genes and 100% of their developmental environment, and dizygotic (DZ) twins share an average of 50% of their genes and 100% of their common developmental environment, co-twin control studies can examine whether shared genes and common developmental environment—referred to jointly as “familial factors”—account for the relationship between two traits. In so doing, co-twin studies can help to distinguish between potentially causal relationships among clinical phenotypes, or alternatively, between shared genetic or environmental linkages among phenotypes (37). For example, within a sample of MZ twin pairs discordant for chronic fatigue, a potential causal role for emotional instability can be considered when higher emotional instability is consistently linked with the affected twin but not the unaffected twin. However, if affected and unaffected co-twins do not differ with regard to emotional instability, familial factors linking both emotional instability and chronic fatigue may be indicated. Further, the relationship of the phenotypes within DZ twins is useful in establishing whether the shared familial linkage is genetic or environmental. If the link between two phenotypes is significant within DZ pairs but not MZ pairs, a shared genetic linkage is suggested. For clarity, Figure 1 (adapted from McGue et al., 2010 (37)) presents the potential patterns of within-twin pair associations for two hypothetical phenotypes.
Figure 1.
*Interpreting Patterns of Within-Pair Associations for Causation and Confounding in Monozygotic (MZ) and Dizygotic (DZ) Twins
Figure 1a) Causal association – the magnitude of the association within pairs is the same for both MZ and DZ pairs
Figure 1b) Partial genetic confounding – the magnitude of the association within pairs is attenuated but not eliminated in MZ compared to DZ twins
Figure 1c) Complete genetic confounding – the magnitude of the association is completely attenuated in MZ pairs compared to DZ pairs
*Adapted from: McGue M, Osler M, Christensen K: Causal Inference and Observational Research: The Utility of Twins. Perspect Psychol Sci. 2010, 5:546-556, Figure 1
The purpose of the present study was to extend the current literature by examining the traits of emotional instability and extraversion and their association with chronic fatigue in twins from the University of Washington Chronic Fatigue Twin Registry. We used two non-mutually exclusive definitions of chronic fatigue in order to evaluate whether increasing specificity of diagnostic criteria changed the associations between personality factors and chronic fatigue. Our aim was to replicate the finding of shared genetic loading for emotional instability (22) and to investigate whether extraversion and chronic fatigue were similarly confounded by familial factors, either genes or common environment. Given prior mixed results with extraversion and CFS, we did not expect to find familial confounding. We therefore hypothesized that 1) high emotional instability and low extraversion are associated with chronic fatigue and CFS-like illness; 2) the relationship between emotional instability and both definitions of chronic fatigue is accounted for by familial factors, particularly shared genetic mechanisms; 3) the relationship between extraversion and both definitions of chronic fatigue is not accounted for by familial factors; and 4) relatively strict diagnostic criteria do not change the association between these personality factors and chronic fatigue.
METHODS
Participants
All 514 twins (257 twin pairs) who contributed to the present analyses were volunteers in the University of Washington Chronic Fatigue Twin Registry (38). A detailed description of the construction of the Registry and the evaluation procedures is provided elsewhere (38). Twin pairs in which at least one member was chronically fatigued (a specified fatigue duration or diagnosis of CFS was not required) or had chronic pain were solicited through advertisements in patient support groups (55%), solicitations placed on CFS electronic bulletin boards (18%), clinicians and researchers familiar with CFS (10%), twin researchers or organizations (6%), friends or relatives (3%), and various other uncategorized means (9%). To be included in the Registry, all study participants completed a detailed mailed questionnaire assessing a range of topics, including demographics, habits, lifestyle, physical and emotional health, zygosity, and symptoms of CFS. The 1994 CDC case definition of CFS (1) was used to measure chronic fatigue of six months duration and CFS symptom criteria. A control version of the questionnaire that did not refer to fatigue was used for non-fatigued twins. Written, informed consent was obtained from each Registry member, and all procedures were approved by the University of Washington Institutional Review Board and in accordance with the ethical standards of the Helsinki Declaration.
Eligibility Criteria and Definitions of Chronic Fatigue
Fatigued twins were classified according to two non-mutually exclusive case definitions of chronic fatigue. The first definition, chronic fatigue lasting at least six months, required a positive response to the question: “Have you been fatigued for at least six months?” Twins who did not endorse this question were considered controls. The second, more stringent definition, chronic fatigue for at least six months not explained by medical and psychiatric conditions, used an algorithm based on the inclusionary and medical and psychiatric exclusionary components of the CDC case definition for CFS (1). Specifically, to be classified as positive for the second definition, participants had to endorse the presence of at least four of eight symptoms: impaired memory or concentration, sore throat, tender glands, aching or stiff muscles, multi-joint pain, new headaches, unrefreshing sleep, and post-exertional fatigue (1). Participants also had to endorse that their fatigue lasted for at least six months, was not lifelong, and resulted in a reduction in occupational, educational, social, or personal activities. All twins with a body mass index ≥ 45 kg/m2 or who reported any of the exclusionary conditions were excluded from this definition. The first definition was called “chronic fatigue” and the second, more stringent definition was called “CFS-like illness.”
The Registry questionnaire contained a checklist of self-reported medical and psychiatric conditions that was used to determine exclusionary conditions in both fatigued and non-fatigued co-twins. Twins reported whether a condition was currently active or had resolved, and whether a physician had evaluated the condition. Examples of exclusionary conditions included (but were not limited to) steroid-dependent asthma, infectious hepatitis, diabetes, bipolar disorder, cancer (other than skin), congestive heart failure, stroke, cirrhosis, multiple sclerosis, and systemic lupus erythematosus. Exclusionary conditions were determined by consensus of two general internists, a psychologist with expertise in CFS, an infectious disease specialist, and an internist/emergency room physician with knowledge of, but little exposure to, patients with CFS. To assess the reliability of the exclusionary diagnoses, self-reported conditions were compared to physician confirmation of those diagnoses by chart review and telephone contact with treating physicians for a subsample of 44 twins. Within this subsample, no fatigued twin was determined to be ineligible because of an exclusionary condition that was missing or inaccurately reported on the self-report questionnaire. Conversely, no exclusionary conditions were observed in any twin who self-reported good health.
Assignment of Zygosity
We employed a commonly-used self-report measure to assign zygosity. This measure contains multiple questions about childhood similarity in twin pairs. Twin pairs whose responses were concordant for the question, “As children, were you and your twin as alike as two peas in a pod, or of only ordinary family resemblance?” were classified as either MZ (both twins agreed on “alike as two peas in a pod”) or DZ (both twins agreed on “ordinary family resemblance”). In cases where responses were discordant, zygosity was assigned by using an algorithm based on several additional questions assessing childhood similarity. The use of this method to assign zygosity has been demonstrated to be 95%-98% accurate compared to biological indicators (39, 40). Pairs with indeterminate zygosity were excluded from the analyses.
Measures of Emotional Instability and Extraversion
Twins completed the Neuroticism and Extraversion subscales of the NEO-Five Factor Inventory (NEO-FFI) (13). The NEO-FFI is a 60-item version of the Revised NEO Personality Inventory, a 240-item measure of the Five Factor Model domains of Emotional Instability, Extraversion, Agreeableness, Conscientiousness, and Openness to Experience. The Emotional Instability and Extraversion subscales of the 60-item NEO-FFI comprise 12 questions each and have acceptable reliability and construct validity (13). Alphas for emotional instability and extraversion in the present sample were 0.90 and 0.81, respectively. Strong evidence indicates that both traits are substantially heritable, with estimates ranging from 0.41 to 0.58 for emotional instability and 0.49 to 0.57 for extraversion (41).
Statistical Analyses
Descriptive statistics were calculated by using means and standard deviations for continuous variables and frequencies for categorical variables. In the full sample, we also examined concordance rates for both definitions of chronic fatigue by zygosity, and mean levels of extraversion and emotional instability for both definitions by zygosity. We then examined the full sample for individual-level associations of emotional instability and extraversion with both definitions of chronic fatigue by using generalized estimating equations (GEE) to account for correlations within twin pairs. These analyses also controlled for age and sex. Because 4 of the 8 defining symptoms for CFS-like illness involve pain, our analyses did not control for chronic pain status. Our initial models were similar to standard, non-twin investigations of associations insofar as they adjusted for correlated data but otherwise ignored twin status to estimate the overall effects among the variables of interest in the population. This first step was imperative because it is unnecessary to investigate familial confounding without an overall phenotypic association.
A second set of analyses examined the within-twin pair associations of emotional instability and extraversion with both definitions of chronic fatigue. For these analyses, we first calculated the within-pair difference scores for twin pairs who were discordant for both definitions. Using those scores, we estimated a new set of GEE models for MZ and DZ pairs separately. An examination of these zygosity-stratified, within-twin pair models can illuminate the potential familial confounding in the relationship between the personality factors and both definitions of chronic fatigue. Thus, if the within-twin pair effects for emotional instability and extraversion were comparable for both MZ and DZ twin pairs who were discordant for fatigue status, we can infer that the individual-level association between these personality factors and chronic fatigue may be causal (i.e., relatively high emotionally instability at a trait level predisposes one to chronic fatigue or CFS-like illness). Alternately, if the within-twin pair effects were large only for the discordant DZ twin pairs (and not for the MZ pairs), we would suspect possible genetic confounding for both traits (42).
RESULTS
Of the 257 twin pairs identified in the Registry, 12 twin pairs were excluded from our sample because of indeterminate zygosity, yielding a total usable sample of 245 pairs (490 individuals). Among these pairs, 9% were male-male twins and 91% were female-female twins. On average, participants were born in 1953, and all participants were white. Most of the sample was composed of MZ twin pairs (67%), although the zygosity distribution within the two definitions of fatigue was similar (64-65% MZ and 35-36% DZ). There were 158 twin pairs who were discordant for chronic fatigue for six months or longer and 118 twin pairs who were discordant for CFS-like illness. The demographic characteristics by fatigue definition and case or control status are presented in Table 1. Twin pairs discordant for fatigue by either definition were significantly different on measures of body mass index, and income was significantly different for twins classified according to the first definition of fatigue. Most of the sample was married or living as married, had 14-15 years of education, and reported an income of $50,000 or more.
Table 1.
Participant characteristics by fatigue definition and case or control status.
| Chronic fatigue of 6 months or longer |
CFS-like illness | |||||
|---|---|---|---|---|---|---|
| Cases n = 308 |
Controls n = 151 |
P | Cases n = 214 |
Controls n =199 |
p | |
| Body mass index, mean (SD) |
26 (7) | 25 (6) | < 0.001 | 26 (6) | 24 (5) | 0.002 |
| Married or living as married, % |
61 | 63 | 0.85 | 56 | 59 | 0.83 |
| Years of education, mean (SD) |
14 (3) | 15 (3) | 0.25 | 15 (3) | 15 (3) | 0.83 |
| Annual income category,% | 0.007 | 0.09 | ||||
| $0 – 14,999 | 16 | 6 | 15 | 6 | ||
| $15,000 – 24,999 | 12 | 13 | 14 | 16 | ||
| $25,000 – 34,999 | 17 | 17 | 18 | 14 | ||
| $35,000– 49,999 | 14 | 20 | 12 | 20 | ||
| $50,000 or more | 40 | 45 | 41 | 43 | ||
CFS = chronic fatigue syndrome; SD = standard deviation.
Fatigue Concordance Rates and Personality Means
While 42% of the MZ twin pairs were concordant for chronic fatigue of six months or longer, only 29% of the DZ twin pairs were concordant for this definition of chronic fatigue. Likewise, 26% of the MZ and 13% of the DZ twin pairs were concordant for CFS-like illness. The higher concordance rates in MZ than in DZ twin pairs suggest that chronic fatigue and CFS-like illness are heritable, a condition that is necessary for further analysis of genetic confounding between personality and chronic fatigue.
Table 2 presents the means and standard deviations for the personality variables by fatigue definition and zygosity. For chronic fatigue of six months or longer, the means for emotional instability were similar for MZ twins who were discordant for the condition, but DZ twins differed by 6 points. Findings were similar for CFS-like illness, suggesting a pattern that is consistent with genetic confounding. For extraversion, mean differences for discordant MZ and DZ twin pairs were of similar magnitude and direction for both definitions of chronic fatigue. This pattern suggests a causal association between extraversion and chronic fatigue.
Table 2.
Means and standard deviations for Emotional Instability and Extraversion by fatigue<break/>definition and zygosity
|
Chronic fatigue of 6 months
or longer |
CFS-like illness | |||
|---|---|---|---|---|
| Cases MZ n = 214 DZ n = 94 |
Controls MZ n = 99 DZ n = 51 |
Cases MZ n = 148 DZ n = 66 |
Controls MZ n = 133 DZ n = 65 |
|
| Emotional Instability | ||||
| MZ Twins, mean (SD) | 56 (11) | 56 (11) | 55 (11) | 56 (11) |
| DZ Twins, mean (SD) | 58 (11) | 52 (10) | 59 (10) | 53 (10) |
| Extraversion | ||||
| MZ Twins, mean (SD) | 44 (13) | 49 (10) | 43 (13) | 49 (11) |
| DZ Twins, mean (SD) | 44 (11) | 52 (9) | 44 (11) | 51 (9) |
CFS = chronic fatigue syndrome; MZ = monozygotic; DZ = dizygotic; SD = standard deviation
Individual-level Associations
Emotional instability and extraversion were not correlated in our sample (r = −0.08, p > .10). Therefore, our analyses to examine the individual-level association of each personality variable and both definitions of fatigue were based on separate GEE models.
Emotional instability
Because we found no fatigue-based mean difference in emotional instability within MZ pairs (see Table 2), and because MZ pairs made up about two-thirds of the sample, our initial models to examine the individual-level association of emotional instability with both definition of chronic fatigue included an interaction term for zygosity X emotional instability in addition to the main effect terms for age, sex, zygosity, and emotional instability. For chronic fatigue of six months or longer, we observed main effects for zygosity (B = −1.81, p = .007) and emotional instability (B = −0.03, p = .002), as well as the expected zygosity X emotional instability interaction effect (B = 0.03, p = .009). This finding verifies that the mean difference in emotional instability in DZ cases and controls was both statistically significant and the primary reason for the significant main effect of emotional instability. Chronic fatigue of six months or longer was associated with higher emotional instability scores, but only in the DZ pairs. Results for CFS-like illness were nearly identical (emotion instability zygosity X emotional instability interaction B = 0.04, p = .002).
Extraversion
Because we found fatigue-based mean differences on emotional instability within both MZ and DZ pairs (see Table 2), the models to examine the individual-level association of extraversion with both definition of chronic fatigue included main effects only for age, sex, and extraversion. For chronic fatigue of six months or longer, only extraversion contributed to the model in the expected direction (B = 0.03, p < .0005). Results were identical for the CFS-like illness model. Both definitions of chronic fatigue were associated with lower extraversion scores.
Within-twin pair analyses
The within-twin pair analyses focused only on twin pairs who were discordant for both definitions of chronic fatigue. For chronic fatigue of six months or longer, 88 MZ and 44 DZ twin pairs were discordant. For CFS-like illness, 76 MZ and 41 DZ pairs were discordant.
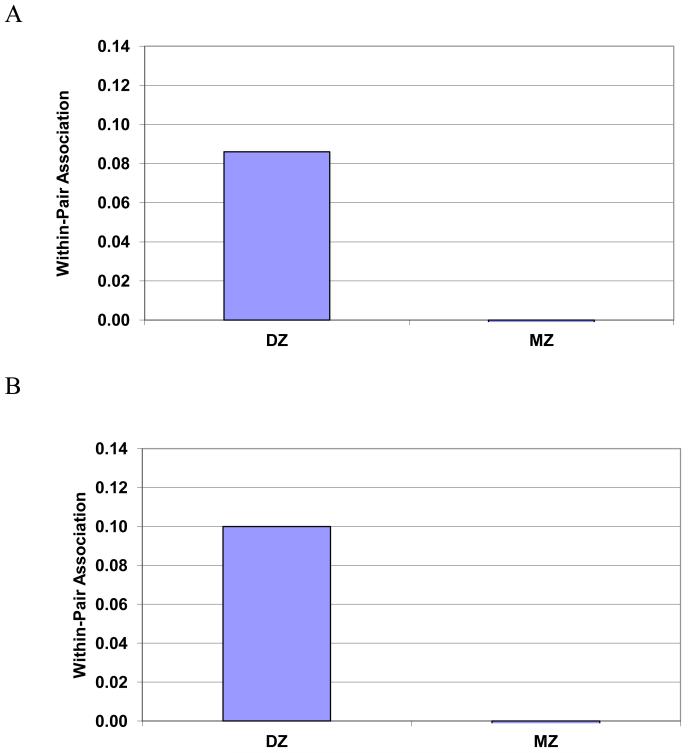
Emotional instability
Figure 2 presents the MZ and DZ within-twin pair associations of emotional instability with both definitions of chronic fatigue. Although the MZ within-twin pair associations with both definitions of fatigue were not reliably different from zero (B’s for both definitions < −0.004, p’s > .70), the DZ within-twin pair associations were significant (B = 0.086, p = .003 for chronic fatigue of six months or longer; B = 0.100, p = .001 for CFS-like illness). This finding suggests that the association between emotional instability and both definitions of chronic fatigue is almost completely confounded by common genetic mechanisms, regardless of the stringency of diagnostic criteria.
Figure 2.
Monozygotic (MZ) and dizygotic (DZ) within-twin pair associations of emotional instability with two definitions of chronic fatigue
Figure 2a) Chronic fatigue of 6 months or longer
Figure 2b) CFS-like illness
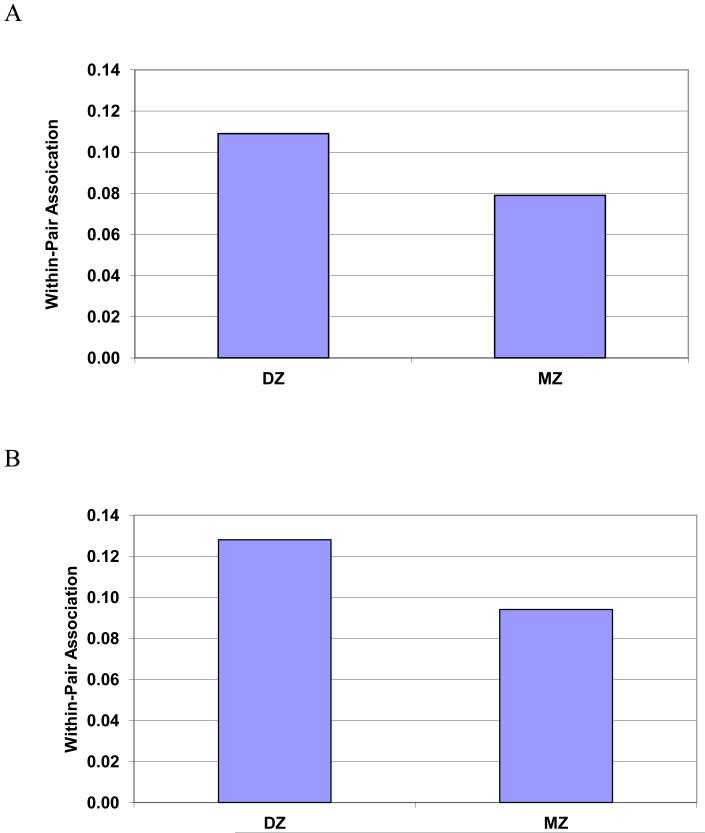
Extraversion
Figure 3 presents the MZ and DZ within-twin pair associations of extraversion with both definitions of chronic fatigue. We found that the MZ within-twin pair associations were significant for both chronic fatigue of six months or longer (B = −0.079, p < .0005) and CFS-like illness (B = −0.094, p < .0005). Moreover, the DZ within-twin pair associations were also significant and slightly greater in magnitude for both definitions of chronic fatigue (B = −0.109, p < .0005 for chronic fatigue of six months or longer; B = −0.128, p = .011 for CFS-like illness). The slight attenuation of the effect in MZ compared to DZ pairs suggests that the association between low extraversion and both definitions of chronic fatigue may be somewhat confounded by familial factors. Nevertheless, the strong association that remained in the MZ pairs, even when controlling for shared genetics, is consistent with the hypothesis that, to an important degree, extraversion affects fatigue, fatigue affects extraversion, and the relationship may be mutually reinforcing, regardless of the initial direction of causation.
Figure 3.
Monozygotic (MZ) and dizygotic (DZ) within-twin pair associations of extraversion with two definitions of chronic fatigue
Figure 3a) Chronic fatigue of 6 months or longer
Figure 3b) CFS-like illness
DISCUSSION
In this co-twin control study we found associations between the personality traits of emotional instability and extraversion and two non-mutually exclusive definitions of chronic fatigue, such that the second definition is more stringent than the first. Our findings support each of our four initial hypotheses. First, we detected an overall individual-level effect for emotional instability and chronic fatigue of six months or longer as well as CFS-like illness, but only for DZ twins. We also found an overall effect for extraversion for both definitions of chronic fatigue, regardless of zygosity. Second, after controlling for familial factors in within-twin pair analyses, we found a significant association between high emotional instability and both definitions of chronic fatigue, but only in the DZ twin pairs. These results are consistent with shared genetic confounding between emotional instability and chronic fatigue. Third, we found significant within-twin pair associations between low extraversion and both definitions of chronic fatigue for both MZ and DZ pairs, although there was a slight attenuation of the effect in MZ pairs. The strong association that remained even when we controlled for familial factors suggests that the link between low extraversion and chronic fatigue may be causal. Fourth, the patterns of our findings were consistent for both definitions of chronic fatigue, with a trend toward greater magnitude for the more stringent definition of CFS-like illness. Therefore, it is likely that the relationships among these personality traits and chronic fatigue appear even in less severe cases of chronic fatigue, for which no additional exclusionary criteria are applied.
Our results on emotional instability are consistent with the only other twin studies to date that have examined fatiguing illness and Five Factor Model personality traits (22), (23). Kato and colleagues found that emotional instability predicted chronic fatigue, and that this link involved shared genetic mechanisms that contribute both to emotional instability and to fatiguing illness (22). In their sample, emotional instability was measured 25 years before fatigue was assessed, suggesting that emotional instability was not merely a consequence of the fatiguing illness but rather a significant factor in its etiology. As in our study, the association with emotional instability in their sample held for two different definitions of fatigue, with one definition more stringent than the other. High levels of emotional instability have also been linked to various other physical conditions (23, 43-45). Emotional instability was initially conceptualized by Eysenck as neuroticism or an expression of chronic excitation of the central nervous system. As such, it may cause continuous physiological wear and tear, increasing vulnerability to disease (23). This possibility suggests the need for identifying vulnerable individuals early in life, before emotional instability takes its toll. Prevention and intervention strategies might involve personality screening, stress-reduction practices, and exercise (43). Our findings suggest the need for similar strategies aimed at people who are at risk for developing CFS.
In contrast to our results on emotional instability, our finding of an association between low extraversion and both definitions of chronic fatigue differed from those of Kato and colleagues (22), who found no such association. Our finding suggests that this association is not driven by familial factors. The lack of familial confounding in our data is consistent with the possibility that low extraversion and chronic fatigue have causal dynamics (37). However, these findings do not allow us to determine whether low extraversion predisposes a person to develop a fatiguing illness or whether having a disabling illness such as CFS pushes a person down the extraversion scale over time in the direction of greater introversion, which can then amplify and maintain the condition. Nevertheless, our finding of a potentially causal association, combined with Kato and colleagues’ finding that pre-existing introversion did not increase risk for subsequent development of fatiguing illness, suggests that introversion is likely to be the result of CFS rather than the cause. Prospective studies are needed to clarify the robustness of this association and the direction of causality.
These results may have important implications for clinical interventions for people with CFS. Considerable evidence suggests that extraverted individuals tend to achieve greater levels of subjective well-being than introverted individuals (30, 31). Self and spousal reports of dispositional extraversion and overall positive affect have shown reasonably robust correlations that vary in the range of 0.10 to 0.70 (29, 32) across various ages and cultures (46). Evidence also indicates that guiding introverted people toward acting as if they were extraverted can increase subjective well-being (33). That is, positive affect tends to follow on what individuals do regardless of what traits they have or who they are (33, 47). Therefore, this navigational effect of “doing” may positively alter a person’s daily experience of fatigue and well-being. Clinically, therapeutic efforts can capitalize on this effect to reverse the slide toward greater introversion in everyday life – an outcome to which individuals with CFS may be prone. Consistent with this approach, several randomized clinical trials have demonstrated that cognitive-behavioral and graded exercise interventions that focus on increasing social and physical activity are efficacious in lowering fatigue and improving physical function in people with CFS (36, 48-54). In addition, higher extraversion has also been shown to predict positive response to both antidepressant medication and cognitive-behavioral interventions (34, 35).
A notable strength of this study is our co-twin control design, which is uniquely suited to parse the effects of shared genes and environment on the link between personality and chronic fatigue. Nonetheless, we note several potential limitations. First, Registry twins were recruited by multiple strategies and represent essentially a volunteer rather than a population-based sample. Second, our analyses included more MZ twin pairs than DZ pairs. Despite the smaller number of DZ pairs, however, we found robust associations even in this subsample, suggesting that statistical power was not an issue. Third, none of our analyses controlled for the potential contribution of chronic pain to the relationship between personality and chronic fatigue. Since chronic fatigue and CFS rarely occur without a pain component, we erred on the side of ecological validity. Nonetheless, future studies should examine the link between personality and chronic pain only to determine if our findings are unique to fatiguing illness. Finally, we relied on self-report rather than clinical assessment for exclusionary medical and psychiatric conditions. This methodology could have led to misclassification of twins with regard to either definition of chronic fatigue, but the perfect correspondence between self-reported conditions and chart review information in a subsample of twins argues against this possibility. In addition, any potential misclassification would result in an underestimation of effects, not an overestimation. Future cross-sectional and prospective studies should further examine the link between personality and chronic fatigue in larger, population-based samples.
In conclusion, we found that higher emotional instability and lower extraversion were linked to chronic fatigue, such that emotional instability acted through shared genetic mechanisms and extraversion acted primarily through a bi-directional, causal pathway. Behavioral prevention and intervention strategies can be used to mitigate or reverse the development and maintenance of CFS and other fatiguing illness. Taking an extraverted approach in day-to-day interactions may have a “navigational” effect that lowers morbidity and improves subjective well-being and functioning in people who suffer from chronic fatigue.
ACKNOWLEDGEMENTS
This research was supported by National Institutes of Health awards U19AI38429 (Buchwald) and R01AR51524 (Afari). Drs. Strachan, Buchwald, and Afari are supported in part by award RC2HL103416 (Buchwald). Dr. Strachan is supported in part by R21AI81347. Dr. Afari is also supported by the VA Center of Excellence for Stress and Mental Health.
Footnotes
Conflict of Interest Statement: The authors have no conflict of interest to disclose.
REFERENCES
- 1.Fukuda K, Straus SE, Hickie I, et al. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med. 1994;121:953–959. doi: 10.7326/0003-4819-121-12-199412150-00009. [DOI] [PubMed] [Google Scholar]
- 2.Wessely S, Hotopf M, Sharpe M. Chronic fatigue and its syndromes. Oxford University Press; Oxford; New York: 1998. [Google Scholar]
- 3.Ranjith G. Epidemiology of chronic fatigue syndrome. Occup Med (Lond) 2005;55:13–19. doi: 10.1093/occmed/kqi012. [DOI] [PubMed] [Google Scholar]
- 4.Steele L, Dobbins JG, Fukuda K, et al. The epidemiology of chronic fatigue in San Francisco. Am J Med. 1998;105:83S–90S. doi: 10.1016/s0002-9343(98)00158-2. [DOI] [PubMed] [Google Scholar]
- 5.van Geelen SM, Sinnema G, Hermans HJ, Kuis W. Personality and chronic fatigue syndrome: methodological and conceptual issues. Clin Psychol Rev. 2007;27:885–903. doi: 10.1016/j.cpr.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 6.Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Psychoneuroimmunology and psychosomatic medicine: back to the future. Psychosom Med. 2002;64:15–28. doi: 10.1097/00006842-200201000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Maier SF, Watkins LR. Cytokines for psychologists: implications of bidirectional immune-to-brain communication for understanding behavior, mood, and cognition. Psychol Rev. 1998;105:83–107. doi: 10.1037/0033-295x.105.1.83. [DOI] [PubMed] [Google Scholar]
- 8.Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004;130:601–630. doi: 10.1037/0033-2909.130.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wessely S. Old wine in new bottles: neurasthenia and ‘ME’. Psychol Med. 1990;20:35–53. doi: 10.1017/s0033291700013210. [DOI] [PubMed] [Google Scholar]
- 10.Wessely S. Neurasthenia and Chronic Fatigue: Theory and Practice in Britain and America. Transcultural Psychiatry. 1994;31:173–209. [Google Scholar]
- 11.Greenberg DB. Neurasthenia in the 1980s: chronic mononucleosis, chronic fatigue syndrome, and anxiety and depressive disorders. Psychosomatics. 1990;31:129–137. doi: 10.1016/S0033-3182(90)72185-8. [DOI] [PubMed] [Google Scholar]
- 12.Digman J. Personality structure: Emergence of the five-factor model. Annu Rev Psychol. 1990;41:417–440. [Google Scholar]
- 13.Costa P, McCrae R. Revised NEO Personality lnventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. Psychological Assessment Resources, Inc.; Odessa, FL: 1992. [Google Scholar]
- 14.Costa PT, Jr., McCrae RR. Neuroticism, somatic complaints, and disease: is the bark worse than the bite? J Pers. 1987;55:299–316. doi: 10.1111/j.1467-6494.1987.tb00438.x. [DOI] [PubMed] [Google Scholar]
- 15.Blakely AA, Howard RC, Sosich RM, et al. Psychiatric symptoms, personality and ways of coping in chronic fatigue syndrome. Psychol Med. 1991;21:347–362. doi: 10.1017/s0033291700020456. [DOI] [PubMed] [Google Scholar]
- 16.Buckley L, MacHale SM, Cavanagh JT, et al. Personality dimensions in chronic fatigue syndrome and depression. J Psychosom Res. 1999;46:395–400. doi: 10.1016/s0022-3999(98)00120-2. [DOI] [PubMed] [Google Scholar]
- 17.Christodoulou C, Deluca J, Johnson SK, et al. Examination of Cloninger’s basic dimensions of personality in fatiguing illness: chronic fatigue syndrome and multiple sclerosis. J Psychosom Res. 1999;47:597–607. doi: 10.1016/s0022-3999(99)00063-x. [DOI] [PubMed] [Google Scholar]
- 18.Fiedler N, Lange G, Tiersky L, et al. Stressors, personality traits, and coping of Gulf War veterans with chronic fatigue. J Psychosom Res. 2000;48:525–535. doi: 10.1016/s0022-3999(00)00088-x. [DOI] [PubMed] [Google Scholar]
- 19.Johnson SK, DeLuca J, Natelson BH. Personality dimensions in the chronic fatigue syndrome: a comparison with multiple sclerosis and depression. J Psychiatr Res. 1996;30:9–20. doi: 10.1016/0022-3956(95)00040-2. [DOI] [PubMed] [Google Scholar]
- 20.Kersh BC, Bradley LA, Alarcon GS, et al. Psychosocial and health status variables independently predict health care seeking in fibromyalgia. Arthritis Rheum. 2001;45:362–371. doi: 10.1002/1529-0131(200108)45:4<362::AID-ART349>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 21.Masuda A, Munemoto T, Yamanaka T, Takei M, Tei C. Psychosocial characteristics and immunological functions in patients with postinfectious chronic fatigue syndrome and noninfectious chronic fatigue syndrome. J Behav Med. 2002;25:477–485. doi: 10.1023/a:1020423124675. [DOI] [PubMed] [Google Scholar]
- 22.Kato K, Sullivan PF, Evengard B, Pedersen NL. Premorbid predictors of chronic fatigue. Arch Gen Psychiatry. 2006;63:1267–1272. doi: 10.1001/archpsyc.63.11.1267. [DOI] [PubMed] [Google Scholar]
- 23.Charles ST, Gatz M, Kato K, Pedersen NL. Physical health 25 years later: the predictive ability of neuroticism. Health Psychol. 2008;27:369–378. doi: 10.1037/0278-6133.27.3.369. [DOI] [PubMed] [Google Scholar]
- 24.Courneya KSHL. Personality correlates of exercise behavior, motives, barriers and preferences: An application of the five-factor model. Personality and Individual Differences. 1998;24:625–633. [Google Scholar]
- 25.De Moor MH, Beem AL, Stubbe JH, Boomsma DI, De Geus EJ. Regular exercise, anxiety, depression and personality: a population-based study. Prev Med. 2006;42:273–279. doi: 10.1016/j.ypmed.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 26.Rhodes RE, Courneya KS, Bobick TM. Personality and exercise participation across the breast cancer experience. Psychooncology. 2001;10:380–388. doi: 10.1002/pon.516. [DOI] [PubMed] [Google Scholar]
- 27.Zautra AJ, Fasman R, Reich JW, et al. Fibromyalgia: evidence for deficits in positive affect regulation. Psychosom Med. 2005;67:147–155. doi: 10.1097/01.psy.0000146328.52009.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chubb HL, Jones I, Hillier J, et al. Chronic fatigue syndrome—Personality and attributional style of patients in comparison to healthy controls and depressed individuals. Journal of Mental Health. 1999;8:351–359. [Google Scholar]
- 29.Diener E, Lucas R. Personality and subjective well-being. In: Kahneman D, Diener E, Schwarz N, editors. Well-being: The foundations of hedonic psychology. Russell Sage Foundation; New York: 1999. pp. 213–229. [Google Scholar]
- 30.Diener E, Suh EM, Lucas RE, Smith HL. Subjective Well-Being: Three Decades of Progress. Psychological Bulletin. 1999;125:276–302. [Google Scholar]
- 31.Diener E, Oishi S, Lucas RE. Personality, culture, and subjective well-being: emotional and cognitive evaluations of life. Annu Rev Psychol. 2003;54:403–425. doi: 10.1146/annurev.psych.54.101601.145056. [DOI] [PubMed] [Google Scholar]
- 32.Lucas RE, Fujita F. Factors influencing the relation between extraversion and pleasant affect. J Pers Soc Psychol. 2000;79:1039–1056. doi: 10.1037//0022-3514.79.6.1039. [DOI] [PubMed] [Google Scholar]
- 33.Fleeson W, Malanos AB, Achille NM. An intraindividual process approach to the relationship between extraversion and positive affect: is acting extraverted as “good” as being extraverted? J Pers Soc Psychol. 2002;83:1409–1422. [PubMed] [Google Scholar]
- 34.Bagby R, Joffe R, Parker J, Kalemba B, Harkness K. Major depression and the five-factor model of personality. J Personal Disord. 1995;9:224–234. [Google Scholar]
- 35.Bagby RM, Quilty LC, Segal ZV, et al. Personality and differential treatment response in major depression: a randomized controlled trial comparing cognitive-behavioural therapy and pharmacotherapy. Can J Psychiatry. 2008;53:361–370. doi: 10.1177/070674370805300605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.White PD, Goldsmith KA, Johnson AL, et al. Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome (PACE): a randomised trial. Lancet. 2011;377:823–836. doi: 10.1016/S0140-6736(11)60096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McGue M, Osler M, Christensen K. Causal Inference and Observational Research: The Utility of Twins. Perspect Psychol Sci. 2010;5:546–556. doi: 10.1177/1745691610383511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Buchwald D, Herrell R, Ashton S, et al. The Chronic Fatigue Twin Registry: method of construction, composition, and zygosity assignment. Twin Res. 1999;2:203–211. doi: 10.1375/136905299320565870. [DOI] [PubMed] [Google Scholar]
- 39.Eisen S, Neuman R, Goldberg J, Rice J, True W. Determining zygosity in the Vietnam Era Twin Registry: an approach using questionnaires. Clin Genet. 1989;35:423–432. doi: 10.1111/j.1399-0004.1989.tb02967.x. [DOI] [PubMed] [Google Scholar]
- 40.Torgersen S. The determination of twin zygosity by means of a mailed questionnaire. Acta Genet Med Gemellol (Roma) 1979;28:225–236. doi: 10.1017/s0001566000009077. [DOI] [PubMed] [Google Scholar]
- 41.Bouchard TJ, Jr., McGue M. Genetic and environmental influences on human psychological differences. J Neurobiol. 2003;54:4–45. doi: 10.1002/neu.10160. [DOI] [PubMed] [Google Scholar]
- 42.Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry. 1999;156:837–841. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- 43.Friedman HS, Booth-Kewley S. The “disease-prone personality”. A meta-analytic view of the construct. Am Psychol. 1987;42:539–555. doi: 10.1037//0003-066x.42.6.539. [DOI] [PubMed] [Google Scholar]
- 44.Stanwyck DJ, Anson CA. Is personality related to illness? Cluster profiles of aggregated data. Advances. 1986;3:4–15. [Google Scholar]
- 45.Yousfi S, Matthews G, Amelang M, Schmidt-Rathjens C. Personality and disease: correlations of multiple trait scores with various illnesses. J Health Psychol. 2004;9:627–647. doi: 10.1177/1359105304045339. [DOI] [PubMed] [Google Scholar]
- 46.Lucas RE, Diener E, Grob A, Suh EM, Shao L. Cross-cultural evidence for the fundamental features of extraversion. J Pers Soc Psychol. 2000;79:452–468. doi: 10.1037//0022-3514.79.3.452. [DOI] [PubMed] [Google Scholar]
- 47.Cantor N,JN, Langston C, et al. Life tasks and daily life experience. Journal of Personality. 1991;59:425–451. [Google Scholar]
- 48.Deale A, Chalder T, Marks I, Wessely S. Cognitive behavior therapy for chronic fatigue syndrome: a randomized controlled trial. Am J Psychiatry. 1997;154:408–414. doi: 10.1176/ajp.154.3.408. [DOI] [PubMed] [Google Scholar]
- 49.Fulcher KY, White PD. Randomised controlled trial of graded exercise in patients with the chronic fatigue syndrome. Bmj. 1997;314:1647–1652. doi: 10.1136/bmj.314.7095.1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moss-Morris R, Sharon C, Tobin R, Baldi JC. A randomized controlled graded exercise trial for chronic fatigue syndrome: outcomes and mechanisms of change. J Health Psychol. 2005;10:245–259. doi: 10.1177/1359105305049774. [DOI] [PubMed] [Google Scholar]
- 51.Prins JB, Bleijenberg G, Bazelmans E, et al. Cognitive behaviour therapy for chronic fatigue syndrome: a multicentre randomised controlled trial. Lancet. 2001;357:841–847. doi: 10.1016/S0140-6736(00)04198-2. [DOI] [PubMed] [Google Scholar]
- 52.Sharpe M, Hawton K, Simkin S, et al. Cognitive behaviour therapy for the chronic fatigue syndrome: a randomized controlled trial. Bmj. 1996;312:22–26. doi: 10.1136/bmj.312.7022.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Price JR, Mitchell E, Tidy E, Hunot V. Cognitive behaviour therapy for chronic fatigue syndrome in adults. Cochrane Database Syst Rev. 2008:CD001027. doi: 10.1002/14651858.CD001027.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Edmonds M, McGuire H, Price J. Exercise therapy for chronic fatigue syndrome. Cochrane Database Syst Rev. 2004:CD003200. doi: 10.1002/14651858.CD003200.pub2. [DOI] [PubMed] [Google Scholar]