Abstract
Preoperative laboratory markers of primary hyperparathyroidism including serum parathormone (PTH), calcium and phosphate level may have some predictive value about the size and volume of the abnormal parathyroid gland tissue which needs to be resected in primary hyperparathyroidism. In a Prospective study from 2003 to 2010, 69 patients with parathyroid adenoma were enrolled. The correlation between preoperative serum PTH, calcium and phosphate level with adenoma’s weight and volume was analyzed separately. Adenoma volume was calculated via an equation for the volume of a spheroid object. The data were analyzed via a multiple analysis of variance, and a correlation coefficient was calculated. The level of significance was set at p _ .05. There was a significant correlation between adenoma weight and serum calcium and parathormone levels (p = .0001 and p = .0001, respectively). There was no significant correlation between adenoma weight and serum phosphate. With respect to adenoma weight, there was a significant relationship with parathormone levels and serum calcium (p = .0001 and p = .0001, respectively). There was no significant relationship between serum phosphate and aden2oma weight. Preoperative serum PTH and calcium levels may be valuable in predicting parathyroid adenoma volume and weight in primary hyperparathyroidism for a single adenoma.
Keywords: Primary hyperparathyroidism, Adenoma, Weight, Volume, Biochemical markers
Introduction
Improper, excess secretion of parathyroid hormone (PTH), which leads to hypercalcemia and hypophosphatemia, is known as primary hyperparathyroidism (PHPT). Primary hyperparathyroidism is a common disorder, and since the main etiology of this disease in approximately 85–90 % patients is single parathyroid adenoma, it can usually (roughly 95 %) be successfully treated by parathyroidectomy [1]. The less common causes of hyperparathyroidism are parathyroid hyperplasia, multiple parathyroid adenomas, or parathyroid carcinoma. Excision of the adenomatous gland through bilateral neck exploration has been the standard treatment method in patients with single parathyroid adenoma. Because of lower success rate and considerable rise in mortality and morbidity of the second exploration, detection and excision of all the enlarged parathyroid tissue at the first surgery is the main goal of operative management in PHPT. The ability to predict the size and identify the approximate location of a parathyroid adenoma can therefore greatly assist the operating surgeon [2]. On the other hand, focused surgical techniques not only reduce operation time and lower complication rates but also can improve cosmetic view. However, in spite of the availability of a wide range of endocrinological and imaging investigations, which consist of ultrasonography, intraoperative PTH assays, scintigraphy, magnetic resonance imaging (MRI), and computed tomography (CT), no unique survey has been shown to definitely identify parathyroid adenomas in all patients. Finding a significant relationship between biochemical manifestations of hyperparathyroidism such as serum parathyroid hormone, serum calcium and serum phosphate levels, and parathyroid adenoma weight and volume could be used to determine the extent of surgical parathyroid gland resection. If such a correlation does exist, it may help the surgeon to formulate a sense of size of the adenoma during operation [3]. Up to now results about this correlation among different retrospective studies are controversial [2, 4–8]. In this study, we prospectively examine the predictive value of preoperative biochemical findings about the size and weight of parathyroid adenoma.
Methods
All patients who underwent minimally invasive parathyroidectomy because of hyperparathyroidism (HPT) from April 2003 to February 2010 have been included in this prospective study. Patients with parathyroid carcinoma, parathyroid hyperplasia, multiple adenomas, secondary or tertiary HPT, and those with serum creatinine more than 1.5 mg/dl were excluded. Sixty-nine patients who had single parathyroid adenoma were accepted to enter the study. The most recent preoperative serum parathyroid hormone, phosphate, calcium levels, albumin, creatinine, and demographic data such as sex and age were recorded. The maximum preoperative PTH and serum calcium levels were reported as percent more than normal upper limit to adjust different assays. These blood biomarkers had been measured for all patients within 45 days of surgery. None of the patients were treated with calcium-chelating agents. A single general surgeon had resected parathyroid adenoma in all these patients and the single pathologist had confirmed the parathyroid adenoma in all tissue samples. In the pathology department, the adenoma was stripped of fat and its weight and dimensions were measured before histological examination. The volume of the adenoma could not be measured directly but estimated via the measured dimensions and a standard mathematical formula for calculating the volume of an ellipsoid object (4/3 × # × ab2, where a is semi-major axis length, b is semi-minor axis length, and # = 3.14159). Separately the correlation of adenoma weight and volume with preoperative serum PTH, calcium, and phosphate was analyzed. Correlation coefficients were calculated for parathyroid adenoma weight and volume with preoperative serum calcium, serum iPTH. In addition, regression models were fit to try to predict the weight and volume of excised adenomas based on the preoperative serum calcium, phosphate, and PTH levels. Data analysis was conducted by using SPSS version 19 for Windows and the results were expressed as means ± SD. Probability values of less than 0.05 were considered significant. The protocol of the study was revised and approved by the institutional committee of Shahid Beheshti Medical University (SBMU), and each patient was provided the informed consent before participating in the study.
Results
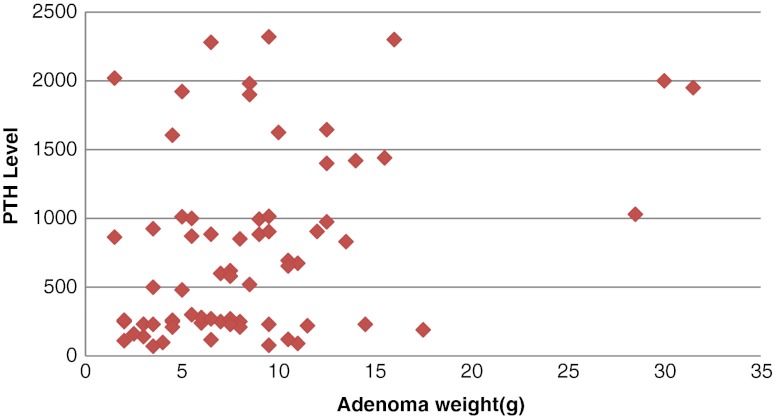
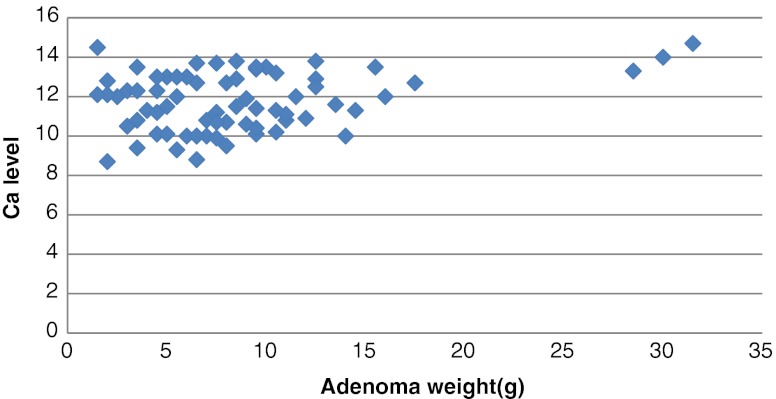
Of 69 patients entered, 52 (75 %) patients were women and 17 (25 %) were men. Their mean age was 54 ± 14 years. The mean preoperative parathyroid hormone level was 770.971 ± 659.19 ng/l, mean serum calcium was 11.74 ± 1.47 mg/dl, and mean serum phosphate was 3.95 ± 1.83 mg/dl. The weight of adenoma was ranged from 1.5 to 31.5 g by mean weight of 8.60 ± 5.91 g. The calculated volume of adenoma was ranged from 0.19 to 36.40 cm3 by mean volume of 6.20 ± 7.94 cm3. No relationship was seen between adenoma weight and age or sex of patients. A strong correlation between adenoma weight and serum parathyroid hormone level (r = 0.381, P = 0.001) (Fig. 1) and calcium level (r = 0.317, P = 0.008) (Fig. 2) was identified. Also, a strong correlation between adenoma volume and serum parathyroid hormone level (r = 0.327, P = 0.006) (Fig. 3) and calcium level (r = 0.333, P = 0.005) (Fig. 4) was identified. Preoperative serum phosphate had no predictive value, neither on adenoma weight (r = −0.101, P = 0.410) nor on volume (r = −0.188, P = 0.122).
Fig. 1.
Correlation between adenoma’s weight and serum PTH level (r = 0.381, p = ,001)
Fig. 2.
Correlation between adenoma’s weight and serum calcium (Ca) level (r = 0.317. p = 0.008)
Fig. 3.
Correlation between adenoma’s volume and serum PTH level (r = 0.327, p = 0.006)
Fig. 4.
Correlation between adenoma’s volume and serum calcium (Ca) level (r = 0.333, p = 0.005)
Discussion
Parathyroid gland features, including color and size, can influence operative decisions for additional exploration during parathyroidectomy. Surgical decisions regarding the extent of neck exploration and parathyroid gland excision may be influenced by preoperative laboratory data and adenoma size. Different studies have demonstrated variable degrees of relationship between several preoperative serum levels with respect to adenoma volume and weight [2, 4–8]. Rutledge et al. [5] displayed a relationship between preoperative serum PTH and calcium level with gland weight or volume. In 1992 Williams et al. [9] demonstrated a considerable correlation between adenoma weight and serum PTH level, but this correlation was mainly dependent on two extraordinarily heavy adenomas. They have explained that as compared with lighter adenomas larger ones secrete less PTH per unit weight. Bindlish et al. [4] not only have been found a significant correlation between PTH and adenoma weight, but also showed a negative weak correlation between adenoma weight and phosphate. In a retrospective study, Mozes et al. [10] suggest that preoperative PTH levels may contribute the surgeon to the probability of large or small parathyroid adenomas. On the other hand, some authors have found no relationship between serum markers of hyperparathyroidism due to adenoma and gland size or mass [6, 7, 11].
According to our results, there is a significant positive correlation between serum PTH and calcium levels with respect to parathyroid adenoma volume and weight. Our study has displayed a difference when other trials have not, mostly because of the exclusion criteria such as renal failure, parathyroid hyperplasia, multiple adenomas, and secondary or tertiary hyperparathyroidism. On the other hand, large sample size may have led to the positive results. Hence, preoperative serum PTH and calcium levels may have noteworthy predictive value about adenoma weight and volume in patients with primary hyperparathyroidism. These findings could have practical value for patients in which a small mass is localized but biochemical markers suggest a larger adenoma. Consequently, additional localization techniques should be performed preoperatively or intraoperatively that may discover another lesion because multiple adenomas have been found in about 4 % of patients with primary hyperparathyroidism [12–14].
Conclusion
As the final point our findings indicate a significant correlation between preoperative serum PTH and calcium levels with respect to the adenoma weight and volume.
Footnotes
This trial has been carried out in Taleghani hospital, Tehran, Iran.
References
- 1.Clarck OH, Duh QY. Primary hyperparathyroidism, a surgical perspective. Endocrinol Metab Clin North Am. 1989;18:701–714. [PubMed] [Google Scholar]
- 2.Randhawa PS, Mace AD, Nouraei SH, et al. Primary hyperparathyroidism: do perioperative biochemical variables correlate with parathyroid adenoma weight or volume? Clin Otolarygol. 2007;32:179–184. doi: 10.1111/j.1365-2273.2007.01447.x. [DOI] [PubMed] [Google Scholar]
- 3.Hamidi S, Aslani A, Nakhjavani M, et al. Are biochemical values predictive of adenoma’s weight in primary hyperparathyroidism? ANZ J Surg. 2006;76(10):882–885. doi: 10.1111/j.1445-2197.2006.03896.x. [DOI] [PubMed] [Google Scholar]
- 4.Bindlish V, Freeman JL, Witterick IJ, et al. Correlation of the biochemical parameters with single parathyroid adenoma weight and volume. Head Neck. 2002;24:1000–1003. doi: 10.1002/hed.10165. [DOI] [PubMed] [Google Scholar]
- 5.Rutledge R, Steigel M, et al. The relation of serum calcium and immunoparathormone levels to parathyroid size and weight in primary hyperparathyroidism. Surgery. 1985;98:1107–1112. [PubMed] [Google Scholar]
- 6.Dubest C, Bordier PJ, et al. The estimation of PTH in primary hyperparathyroidism. Nouvelle Presse Med. 1985;7:21–25. [PubMed] [Google Scholar]
- 7.Wagner PK, Rothmund M. Correlation of tumor weight and typical pathologic laboratory parameters in primary hyperparathyroidism. Langenbeck’s Arch Chir. 1983;360:133–139. doi: 10.1007/BF01254921. [DOI] [PubMed] [Google Scholar]
- 8.Hedback C, Oden A, Tisell LE. Parathyroid adenoma weight and the risk of death after treatment for primary hyperparathyroidism. Surgery. 1995;117:134–139. doi: 10.1016/S0039-6060(05)80076-5. [DOI] [PubMed] [Google Scholar]
- 9.Williams JG, Wheeler MH, Aston JP, et al. The relationship between adenoma weight and intact (1–84) parathyroid hormone level in primary hyperparathyroidism. Am J Surg. 1992;163:301–304. doi: 10.1016/0002-9610(92)90007-E. [DOI] [PubMed] [Google Scholar]
- 10.Mozes G, Curlee KJ, Rowland CM, et al. The predictive value of laboratory findings in patients with primary hyperparathyroidism. J Am Coll Surg. 2002;194:126–130. doi: 10.1016/S1072-7515(01)01139-5. [DOI] [PubMed] [Google Scholar]
- 11.Bland KI, Tidwell S, von Fraunhofer JA, et al. Intraoperative localization of parathyroid glands using methylthionine chloride/tetramethylthionine chloride in secondary hyperparathyroidism. Surg Gynecol Obstet. 1985;160:42–48. [PubMed] [Google Scholar]
- 12.Casas AT, Burke GJ, Sathyanaryana N, et al. Prospective comparison of technetium 99 m sestamibi/iodine 123 scan versus high resolution ultrasonography for the preoperative localization of abnormal parathyroid glands in patients with previously unoperated primary hyperparathyroidism. Am J Surg. 1993;166:369–373. doi: 10.1016/S0002-9610(05)80335-6. [DOI] [PubMed] [Google Scholar]
- 13.Thule P, Tharoke K, Vasant J, et al. Preoperative localization of parathyroid tissue with technetium-99 m sestamibi I123 subtraction scanning. J Clin Endocrinol Metab. 1994;78:77–82. doi: 10.1210/jc.78.1.77. [DOI] [PubMed] [Google Scholar]
- 14.Casas AT, Burke GJ, Mansberger AR, Jr, et al. Impact of technetium-99 m-sestamibi localization on operative time and success of operations for primary hyperparathyroidism. Am Surg. 1994;60:12–17. [PubMed] [Google Scholar]