Abstract
OBJECTIVES
To estimate risk of comorbid depression on all-cause mortality over time among individuals with diabetes
METHODS
Medline, CINAHL, Cochrane Library, Embase, and Science Direct database were searched through September. 30, 2012. We limited our search to longitudinal or prospective studies reporting all-cause mortality among those having depression and diabetes, compared with those having diabetes alone that used hazard ratios as the main outcome. Two reviewers independently extracted primary data and evaluated quality of studies using predetermined criteria. The pooled random effects adjusted hazard ratios (HRs) were estimated using meta-analysis. The impact of moderator variables on study effect size was examined with meta-regression.
RESULTS
A total of 42,363 respondents from 10 studies were included in the analysis. Depression was significantly associated with risk of mortality (Pooled HRs: 1.50, 95% CI: 1.35, 1.66). Little evidence for heterogeneity was found across the studies (Cochran Q: 13.52, p-value: 0.20, I2: 26.03). No significant possibility of publication bias was detected (Egger’s regression intercept: 0.98, p-value: 0.23).
CONCLUSION
Depression significantly increases the risk of mortality among individuals with diabetes. Early detection and treatment of depression may improve health outcomes in this population.
Depression and type 2 diabetes mellitus (DM) are among the most prevalent chronic diseases in the United States. Approximately 15% of adults in the U.S. will experience a major depressive episode at some point in their life. In 2010, 11.3% of U.S. adults aged 20 or older were diagnosed with diabetes, and this number is growing exponentially. About 1.9 million people aged 20 years or older were newly diagnosed with DM in 2010.
Depression and type 2 DM often co-occur. Up to 30% of individuals with DM have a significant number of depressive symptoms on depression rating scales and 12 to 18% meet diagnostic criteria for major depression. Patients with DM experience significantly higher rates of depression compared with their age- and gender-matched counterparts. Robust evidence supports the presence of bidirectional interactions between depression and type 2 DM. Depressive episodes often begin early in adult life and are associated with a higher risk of subsequent development of type 2 diabetes. Comorbid depression in patients with DM is strongly associated with burden of DM symptoms, poor self-management and treatment adherence, increase in health care services utilization and medical expenditures and an increased risk of diabetes complications. Diabetes complications such as myocardial infarction, amputation or loss of vision can in turn precipitate or worsen depressive episodes.
Co-morbid depression has been linked with increased mortality among individuals with diabetes in some but not all studies. However no study has systematically reviewed this relationship. This paper addresses that gap by estimating the risk of mortality in patients with comorbid depression and diabetes compared to those with diabetes alone from published and unpublished literature using meta-analysis.
METHODS
Search Strategy
We conducted primary systematic literature searches using combinations of keywords (depression, depressive disorders, major depression, diabetes, diabetes mellitus, and mortality). We first searched five databases: Medline, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Library, Embase, and Science Direct. We limited our search to peer-reviewed articles published up to September 30, 2012 with abstracts in English. We reviewed the reference lists of eligible studies to increase the yield of our search. Finally, we searched the Institute of Scientific Information Web of Science database for studies citing the eligible studies and reviewed their titles and abstracts to determine eligibility.
Selection Criteria
To be included in the current analysis, a report needed to have a longitudinal or prospective study design, report all-cause mortality with Hazard Ratios (HRs), and include individuals with a measure of depression (self-report questionnaire, structured psychiatric interview, ICD-9 code or antidepressant prescription) and type 1 or type 2 diabetes (self-report, ICD-9 code, laboratory result or prescription of glucose lowering medication). We decided to have such broad inclusion criteria because we preferred to err on the side of inclusiveness. To maximize the generalizability of the results of the study, we excluded studies with special populations such as those with a specific complication of diabetes (such as a foot ulcer). We chose HRs to include the effect of depression on all-cause mortality among individuals with diabetes over time; this approach limited the analytic technique of the study to cox-regression. We did not use Relative Risk (RR) or Odds Ratios (ORs) as proxy for HR in our analysis because these do not account for time in the calculation. Furthermore, some studies have shown that longer follow-up time increases the divergence between RR, OR and HR. In the event of multiple publications, only the most recent manuscript was included.
Data Extraction
M.P. and W.J.K. reviewed all the studies using a standardized data extraction form. Discrepancies were resolved by consensus. Primary data extracted for the current analyses included the method by which depression and diabetes were diagnosed, study design, sample size, setting, duration of the follow-up, outcome measures, covariates, hazard ratio, and 95% confidence intervals. Our primary goal was to compare the risk of all-cause mortality between those with diabetes alone and those with comorbid depression and diabetes. Thus, when four group results were presented (no DM/depression, depression only, DM only, and DM and depression), we calculated hazard ratios of having both DM and depression relative to those with DM only using the method outlined by Altman and Gland. If multiple risk estimates were presented in a given manuscript, we selected the estimate that most closely adjusted for demographic characteristics, behavioral risk factors, comorbidity, and DM status. For studies that presented graded relationships (e.g., low, medium, high depressive symptoms), only the cutting scores that correlated the highest with a probable major depression diagnosis were used.
Assessment of Validity
M.P. and W.J.K. independently rated each study on six components of quality with an instrument similar to that used by Grote et al. The components of quality included: clarity of description of the study population, quality of diagnosis of depression, quality of diagnosis of diabetes, appropriateness of statistical test, percentage of successful recruitment of study population, adequacy of sample size, representativeness of study population, attrition rate reported and reflected statistically, and number of key potential confounders adjusted for in multivariate analyses. The quality scores can range from 0 to 16; discrepancies between reviewers were resolved by consensus.
Data Synthesis and Statistical Analysis
M.P. and F.M.W. performed analyses using Review Manager 5 and Comprehensive Meta-Analysis. The studies were weighted by the inverse variance methods described in the user’s manual of the Comprehensive Meta-Analysis. We used both a random effect model and a fixed effect model to pool the study results. We pooled adjusted hazard ratios (HR) with a 95% confidence interval (95% CI). Values greater than 1 indicate an unfavorable impact of depression on mortality. Forrest plots of the estimates and 95% CIs, with the weight of each point estimate indicated by the relative size of the marker, were used to visually examine the range of effects. The heterogeneity of effect sizes was assessed using the Cochran Q statistic (Q-value) and the I2 statistic. A p-value smaller than .01 was considered evidence of significant heterogeneity. Higher I2 values (ranging between 0 and 100 %) indicate greater variability among the studies than would be expected by chance alone.
Using meta-regression, we examined the impact of the following moderator variables on study effect size: study populations (community vs. clinical population), duration of follow-up, study site (U.S. vs. non-U.S.), and age and gender of the majority of subjects, number of observations, quality scores of the report. We also conducted leave-one-out analyses for each study to examine the magnitude of influence of each study on pooled mortality. Publication bias was assessed using funnel plot, Egger’s test, Duval and Tweedie’s trim-and-fill approach, and classic fail-safe N.
RESULTS
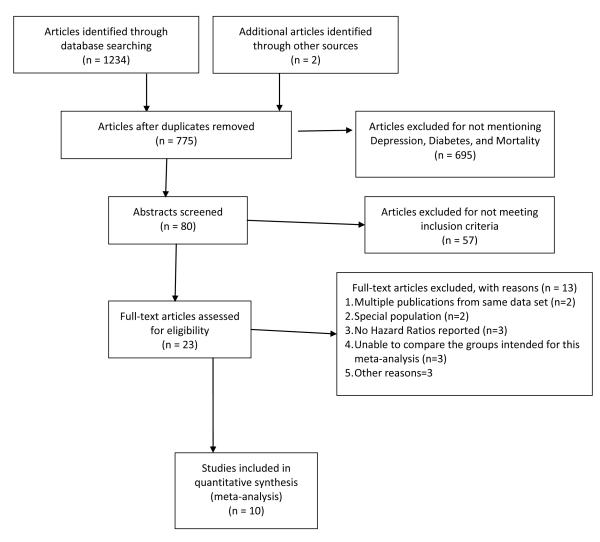
Study Selection (Figure 1)
Figure 1.
Diagram of Study Selection for Meta-Analysis
Adapted from MOOSE Guideline51
EndNote computer software was used to store search results, organize them, and identify duplicate citations. We identified 1236 records from the initial search. After duplicates were identified and removed, 775 potentially relevant unique articles were retrieved. One author (MP) reviewed and excluded 700 manuscripts that did not refer to depression, diabetes, or mortality in the title. When in doubt whether to exclude or include a study based on the title, we included the study for abstract review. Abstracts of the remaining 75 studies were reviewed and 23 articles were selected for full text review. One report that was currently under review in a peer-reviewed journal was identified by an expert researcher and one additional record was identified through bibliographic review. Two authors (M.P. and W.J.K) independently reviewed manuscripts. One study treated depression scores as a continuous variable without a cut-point; we unsuccessfully contacted the first author of the study for additional analyses so that we could include the study in our analysis. Nine reports published in English and one in German were included in the meta-analysis. Figure 1 presents the overall search flow. Table 1 shows the main characteristics of the studies. The characteristics of the 13 studies excluded from the analysis and the reasons for exclusion appear in Table 2.
Table 1.
Description of Studies Included in the Meta-Analysis
| Study | # of cases |
Age at baseline Both vs. DM alone |
Follow- up Years |
Women (%) |
Minority (%) | Site | Population | Measures2 |
Covariates3 | Quality Score |
||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Both | DM alone |
DM | Depression | |||||||||
| Black 200328 | 52 | 401 | 65 | 7 | 59.6 | 100 | US | Community | Self-report | CES-D CIDI |
1 | 13 |
| Zhang 200529 | 1471 | 4121 | 64.2 (12.6) | 10 | 61.3 | 23.7 | US | Community | Self-report | CES-D>16 | 1,2,3 | 14 |
| Bruce 200530 | 401 | 872 | 63.2 (12.2) vs. 64.5 (10.7) |
7.8 ± 2.4 | 48.6 vs. 57.1 | <10 | Australia | Community | Blood Test | GHS | 1,2,3 | 14.5 |
| Richardson 200831 | 806 | 13,694 | 56 vs. 61.9 | 10 | 0 | 53.2 vs. 53.2 | US | Inpatient/outpatient | ICD-9 code | ICD-9 code | 1,2,3 | 13 |
| Katon 200832 | 1657 | 9047 | 71 (12.5) vs. 76.4 (8.2) | 2 | 43 vs.58.7 | <10 | US | Community | DRG ICD-9 code Blood Test |
ICD-9 code | 1,2,3 | 13.5 |
| Lin 200933 | 493 | {Pieper, 2011 #3758} |
59.6 (12.8) vs. 64.7 (12.2) |
4.4 ± 1.5 | 58 vs. 46.9 | 20.4 vs. 21.3 | US | Inpatient/outpatient | Blood Test Physician diagnosis Filled prescription of Insulin or an oral hypoglycemic agent |
PHQ-9 probable major depression diagnosis |
1,2,3 | 16 |
| Pieper 201137 | 165 | 976 | 67.0 (9.6) vs. 64.6 (11.5) |
3.5 | 50 | N/R | Germany | Inpatient/outpatient | Blood Test | DSQ 8 | 1,2,3 | 13 |
| Pan 201134 | 1000 | 3873 | 54~79 | 6 | 100 | <5 | US | Community | Questionnaire | MHI5 51 | 1,2,3 | 14 |
| Sullivan 201235 | 301 | 1326 | 62.2 ± 6.7 | 4.67 ± 1.45 |
39.6 | 34.9 | US | Inpatient/outpatient | Physician diagnosis | PHQ-9 probable major depression diagnosis |
1,2,3 | 13 |
| Ahola 201236 | 313 | 3103 | 43.4 ± 11.4 | 9 | 40.1 vs. 45.9 | <10 | Finland | Community | Blood Test | Purchase of antidepressant |
1,2,3 | 14 |
The study reported only percentage (Total diabetic population n=558). We estimated the numbers of cases using the percentage.
abbreviations: DRG: Diagnosis Related Groups ICD: International Classification of Disease CESD: Center for Epidemiological Studies Depression Scale, CIDI: Composite International Diagnostic Interview, GHS: General Health Status Questionnaire, SCAN: Schedule for Clinical Assessment in Neuropsychiatry 2.1 DSQ: Depression Screening Questionnaire, MHI5: 5-item Mental Health Index Subscale of 36-item Short Form Health Survey BDI: Beck Depression Inventory
Covariates. 1: Sociodemographic characteristics (e.g. age, gender, race/ethnicity, education, marital status, income or income/poverty ratio) 2.Health behaviors (e.g. smoking, physical activity, diet, drinking) 3.Clinical characteristics (e.g. condition, BMI, complications, BP, depression medications)
Table 2.
Description of excluded studies
| Citation | Key findings | Reason for exclusion | |
|---|---|---|---|
| 1 |
38Ismail K, Winkley K, Stahl D, Chalder T, Edmonds M. A cohort study of people with diabetes and their first foot ulcer: the role of depression on mortality. Diabetes Care. 2007; 30(6): 1473-1479. |
Minor and major depressive disorders were associated with an approximately threefold hazard risk for mortality compared with no depression (HR 3.23 [95% CI 1.39–7.51] and HR 2.73 [1.38–5.40], respectively). |
Special population only: patients with first foot ulcer |
| 2 |
39Bot M, Pouwer F, Zuidersma M, van Melle JP, de Jonge P. Association of Coexisting Diabetes and Depression With Mortality After Myocardial Infarction. Diabetes Care. March 1, 2012 2012;35(3):503-509.39 |
Hazard ratios for all-cause mortality were 1.38 (95% CI 1.00–1.90) for patients with diabetes only, and 2.90 (2.07–4.07) for patients with both diabetes and depression. |
Special population only: Only patients Post-MI |
| 3 |
40Katon WJ, Rutter C, Simon G, et al. The Association of Comorbid Depression With Mortality in Patients With Type 2 Diabetes. Diabetes Care. November 2005 2005; 28(11): 2668-2672. |
Minor depression was associated with a 1.67-fold increase in mortality (P = 0.003), and major depression was associated with a 2.30-fold increase (P < 0.0001). |
Same patient population as used with Lin et al (2009), but only three-year follow-up |
| 4 |
41Egede LE, Nietert PJ, Zheng D. Depression and all-cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care. Jun 2005;28(6):1339-1345. |
Compared with the reference group, HRs for all-cause mortality were diabetes present, no depression 1.88 (1.55-2.27); and diabetes present, depression present, 2.50 (2.04-3.08). |
Same data set as paper of Zhang et al (2005) |
| 5 | Lee TA, Shields AE, Vogeli C, et al. Mortality rate in veterans with multiple chronic conditions. J Gen Intern Med. Dec 2007;22 Suppl 3:403-407. |
Veterans with depression and DM experienced lower five-year age adjusted mortality rate than those with diabetes only (OR: 6.50, 95% CI: 5.12, 7.88 vs. OR: 7.07, 95%CI: 6.75, 7.39). |
Outcomes reported ORs, not HRs |
| 6 |
43Rosenthal MJ, Fajardo M, Gilmore S, Morley JE, Naliboff BD. Hospitalization and Mortality of Diabetes in Older Adults: A 3-year prospective study. Diabetes Care. February 1, 1998 1998;21(2):231- 235. |
Compared to older adults with DM only, those with depression and DM experienced 1.32-fold increased mortality in 5-year follow-up period (OR: 1.32, 95% CI: 1.02, 1.70) |
Outcomes reported as ORs, not HRs |
| 7 |
44Black SA, Markides KS. Depressive symptoms and mortality in older Mexican Americans. Ann Epidemiol. Jan 1999;9(1):45-52. |
The odds of having died among diabetics with high levels of depressive symptoms (OR: 4.03, 95% CI: 2.67, 6.11) were three times that of diabetics without high levels of depressive symptoms (OR: 1.36, 95% CI: 0.89, 2.06). |
Same data set as paper of Black et al (2003) |
| 8 |
45Prisciandaro JJ, Gebregziabher M, Grubaugh AL, Gilbert GE, Echols C, Egede LE. Impact of psychiatric comorbidity on mortality in veterans with type 2 diabetes. Diabetes Technol Ther. Jan 2011; 13(1): 73-78. |
Only externalizing disorders were significantly associated with mortality: hazard ratio = 1.22 (95% confidence interval = 1.02-1.47). |
Depression was not clearly defined. The authors categorized psychiatric disorder into two groups: internalizing and externalizing disorders and aggregated data about individuals with depression with other internalizing disorders (e.g. anxiety) |
| 9 |
46Reynolds SL, Haley WE, Kozlenko N. The Impact of Depressive Symptoms and Chronic Diseases on Active Life Expectancy in Older Americans. American Journal of Geriatric Psych. 2008; 16(5): 425-432 410.1097/JGP.1090b1013e31816ff31832e. |
Depressive symptoms reduced active live expectancy by 6.5 years for young-old men (age 70), 3.2 years for old-old men (age 85), 4.2 years for young-old women, and 2.2 years for old-old women. |
Outcome was life expectancy not mortality |
| 10 |
47Gallo JJ, Bogner HR, Morales KH, Post EP, Ten Have T, Bruce ML. Depression, cardiovascular disease, diabetes, and two-year mortality among older, primary-care patients. The American journal of geriatric psychiatry: official journal of the American Association for Geriatric Psychiatry. 2005; 13(9): 748-755. |
Persons with depression at baseline were more likely to die at the end of the 2-year follow-up interval than were persons without depression (relative odds 1.81, 95% confidence interval [1.07, 3.05]; Wald χ2 = 4.96, df = 1, p = 0.03) |
Data on individuals with MI and Diabetes were aggregated. Thus, unable to compare mortality among those with Depression and DM and those with DM only. The outcome was not reported as Hazard Ratio. |
| 11 | Bogner HR, Morales KH, Post EP, Bruce ML. Diabetes, depression, and death: a randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT). Diabetes Care. 2007;30(12):3005-3010. |
Depressed patients with diabetes in the intervention group were less likely to have died during the 5-year follow-up interval than depressed diabetic patients in usual care (adjusted HR 0.49, 95% CI 0.24-0.98) |
Compares mortality rate between individuals who received depression treatment and those who were in comparison group. There was no way to compare the mortality among those with diabetes only and diabetes and depression. |
| 12 |
49Landman GWD, van Hateren KJJ, Kleefstra N, Groenier KH, Gans10 ROB, Bilo HJG. Health-Related Quality of Life and Mortality in a General and Elderly Population of Patients With Type 2 Diabetes (ZODIAC-18). Diabetes Care. November 1, 2010 2010; 33(11): 2378- 2382. |
A 10-point-higher score on the Mental Component Score (MCS) decreased the risk for total mortality by 10%. |
No clear depression cut-off point. |
| 13 |
50Milano A, Singer R. Mortality in co-morbidity (II)--excess death rates derived from a follow-up study on 10,025 subjects divided into 4 groups with or without depression and diabetes mellitus. J Insur Med. 2007;39(3):160-166. |
Appear to be using Egede’s table for basis of their findings. No original data. |
Participants
A total of 42,363 respondents with DM were included in this meta-analysis. Among them, 5,325 individuals had both depression and DM and the remaining 37,038 cases had a diagnosis of DM alone. The number of depression and DM cases in each study ranged between 52 and 1657, whereas the number of DM only cases in each study ranged between 401 and 13,694. Six out of 10 studies recruited study samples from the community, and other studies used hospital or other primary care clinic settings. Seven studies analysed data from mixed age populations and three studies used older adult populations.
Measurement of Depression and Diabetes
Depression was measured by self-reported scales such as the Center for Epidemiologic Studies Depression Scale (CES-D), Patient Health Questionnaire-9 (PHQ-9), ICD-9 code, or antidepressant use. Depression measures were dichotomized with a cut-off point. Two studies measured depression with CES-D with a cut-off point of 16; two studies used the PHQ-9 diagnosis of major depression; two studies used ICD-9 codes; and the other two studies used other symptom severity instruments. One study used purchase of antidepressant as proxy for depression. The baseline depression status was included in the current meta-analysis. To diagnose diabetes, five studies used blood tests, two studies used patient self-report and questionnaire, two studies used ICD-9 codes and one study used filled prescription of insulin or an oral hypoglycaemic agent as DM indicator. Whereas other studies examined individuals with type 2 DM or combined individuals with type 1 and type 2 DM, Ahola and colleagues studied individuals with type 1 DM only.
Study Outcomes
All studies reported adjusted HRs for all-cause mortality and four studies also reported adjusted HRs for cardiovascular mortality. Ahola et al reported the results for women and for men separately. We treated these results as separate studies, instead of calculating pooled HRs. The mean length of follow-up varied from 2 to 10 years. Five studies reported data for five years or longer.
Statistics and Covariates
All studies used Cox-regression models. Nine studies reported the crude number of deaths or Odds Ratio in addition to HR. All results were adjusted for sociodemographic characteristics, and 9 studies also included covariates such as health behaviors (e.g., smoking and physical activity) and clinical characteristics (e.g., comorbidity or Charlson comorbidity score, diabetes complications) in the analysis. However, specific characteristics adjusted for varied among the studies.
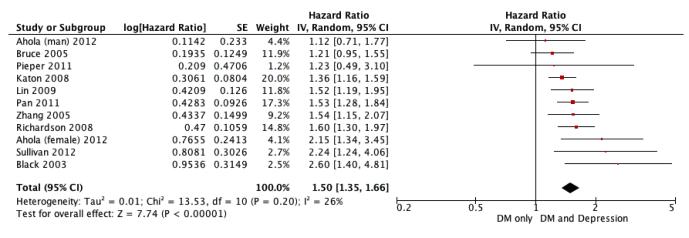
Effect of Depression on Mortality among those with Diabetes (Table 3 and Figure 2)
Table 3.
RESULTS FROM META-ANALYSIS AND META-REGRESSION
| Within group | Between Group | |||||||
|---|---|---|---|---|---|---|---|---|
| N of studies |
Pooled HRs |
95% CI | Cochran Q | p-value | I2 (%) | Cochran Q | p-value | |
| Meta-Analysis | ||||||||
| Random effects | 10 | 1.50 | 1.35, 1.66 | |||||
| Fixed effects | 10 | 1.48 | 1.36, 1.60 | |||||
| Meta-Regression | ||||||||
| Study site | 2.41 | 0.12 | ||||||
| U.S. | 7 | 1.50 | 1.39, 1.62 | 6.88 | 0.33 | 13 | ||
| Non-U.S. | 3 | 1.36 | 1.39, 1.62 | 0.51 | 0.78 | 0 | ||
| Study populations | 0.08 | 0.78 | ||||||
| Community-based | 6 | 1.46 | 1.27, 1.68 | 2.53 | 0.47 | 0 | ||
| Hospitals or Clinics | 4 | 1.66 | 1.38, 1.63 | 10.55 | 0.10 | 43 | ||
| Populations | 0.24 | 0.63 | ||||||
| Mixed-age | 7 | 1.47 | 1.33, 1.62 | 8.73 | 0.27 | 20 | ||
| Older adults | 3 | 1.56 | 1.24, 1.96 | 4.80 | 0.09 | 58 | ||
| Gender | 0.12 | 0.73 | ||||||
| Majority female | 7 | 1.47 | 1.34, 1.61 | 9.54 | 0.22 | 27 | ||
| Majority male | 3 | 1.55 | 1.15, 2.09 | 3.53 | 0.17 | 43 | ||
| Quality Scores | 0.28 | 0.60 | ||||||
| Less than or equal to 13.5 | 5 | 1.48 | 1.32, 1.64 | 4.97 | 0 .29 | 19.5 | ||
| Greater than >13.5 | 5 | 1.42 | 1.26, 1.58 | 6.07 | 0.30 | 17.7 | ||
| Mean follow-up years | 0.00 | 0.97 | ||||||
| Shorter than or equal to 6.5 years | 5 | 1.45 | 1.29, 1.62 | 2.43 | 0.66 | 0.0 | ||
| Longer than 6.5 years | 5 | 1.45 | 1.29, 1.60 | 8.89 | 0.11 | 43.7 | ||
| Number of observations | 0.18 | 0.67 | ||||||
| Less than or equal to 5000 | 7 | 1.42 | 1.26, 1.59 | 9.00 | 0.25 | 22.2 | ||
| Great than 5000 | 3 | 1.47 | 1.32, 1.62 | 2.13 | 0.34 | 6.2 | ||
Figure 2.
Forrest Plot of Studies Included in Meta-analysis of All-cause Mortality Associated with Depression Among Individuals with Diabetes
Depression was significantly associated with increased risk of mortality (Pooled HR: 1.48, 95% CI: 1.36, 1.61). Little evidence for significant heterogeneity was found across the studies (Cochran Q: 13.52, p-value: 0.20, I2: 26.03). Four studies reported risk of cardiovascular mortality in addition to all-cause mortality. Using a random-effect model, depression was significantly associated with increased risk of cardiovascular mortality (Pooled HR=1.21, 95% CI: 1.05, 1.37). We found little evidence for significant heterogeneity in cardiovascular mortality across the studies (Cochran Q=3.96; P=0.41; I2=0%). (Figure 2: Forrest Plot of Studies Included in Meta-analysis of All-Cause Mortality Associated with Depression Among Individuals with Diabetes)
Sensitivity Tests
We conducted three tests to examine the degree of robustness of the above results. First, we compared the random-effect and fixed-effect models and did not find a significant difference in pooled HR between the two (fixed model pooled HR: 1.48 95% CI: 1.36, 1.60 vs. random model pooled HR: 1.50, 95% CI: 1.35, 1.66)(Table 3). The leave-one-out analyses found that no single report unduly influenced the pooled risk ratio estimates of the association between depression and all cause mortality among those with diabetes. Finally, we conducted a series of random effect single covariate meta-regression analyses to examine how each moderator is associated with the pooled HR. We calculated regression coefficients to describe the differences in HRs between the groups categorized by covariate and p-value of the coefficient to examine whether there is a linear relationship between HRs and the covariate. Moderators examined include location of study (the U.S. vs. the non-U.S.), quality scores, sampling frame (community vs. hospital/clinic), length of follow-up, gender of the majority of sample (majority women vs. majority men), age of sample (older adults vs. mixed-age), and the number of observations. No significant moderating effects were found.
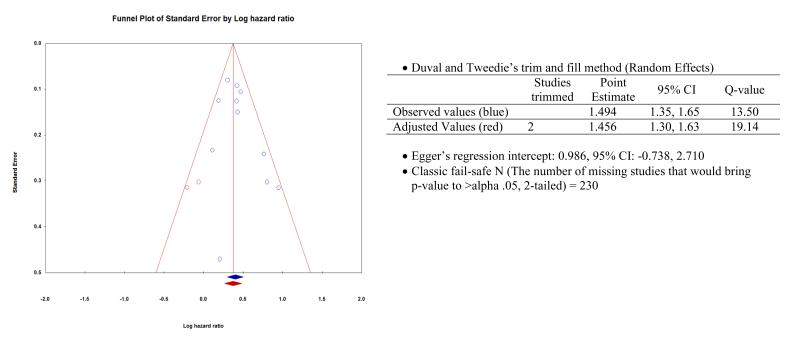
Publication Bias
We first visually inspected the funnel plots, in which each study’s effect size was plotted against the standard error. The asymmetry suggested that small studies with negative results might not have been published. Duval and Tweedie’s trim-and-fill analysis suggested that two studies were missing in the left side of the mean effect. The imputed HR using the trim-and-fill approach was 1.46 (95% CI: 1.30, 1.63), which was slightly lower than our estimation. The result of Egger’s regression intercept approach indicated no significant evidence of publication bias (intercept=0.99, two tailed 95% CI: −0.74, 2.72, p-value = 0.23). The result of classic fail-safe N suggested that 230 nil- or null-reports would be needed to raise the p-value associated with the average effect above an alpha level .05. The fail-safe N value is larger than the recommended 5k+10 limit (=60). The results of these 4 tests indicated that it is unlikely that publication bias poses a significant threat to the validity of findings reported in the current analysis. Figure 3 presents the results of testing for publication bias.
Figure 3.
Results of Publication Bias Tests: Funnel Plot, Trim-and-Fill method, Egger’s regression intercept, and Classic Fail-safe N.
DISCUSSION
Comorbid depression in respondents with diabetes was associated with an approximately 1.5-fold increase in risk of mortality among the individuals with diabetes. Little evidence of heterogeneity was found across studies and the results were consistent across several sensitivity analyses including the leave one out analysis, and the analysis that compared random effect and fixed effect models. Moreover results were also consistent when examining several potential moderators including geographic location of study, gender, community versus hospital/clinic populations, age of population, length of follow-up, and qualities of the studies. Comorbid depression was also associated with an approximately 20% higher risk of cardiovascular mortality in these respondents with diabetes in the four studies examining specific cause of death.
The results of the current analyses are consistent with the existing literature and, to our knowledge, this paper is the first meta-analysis to estimate risk of all-cause mortality associated with comorbid depression among individuals with diabetes. Two studies that did not meet the inclusion criteria because of examining only subgroups of patients with DM who had specific complications were excluded from this meta-analysis but also found increases in mortality among those with comorbid depression and DM. Ismail and colleagues and Bot and colleagues examined individuals with their first diabetes related foot ulcer and those with after myocardial infarction, respectively. Both studies concluded that comorbid depression increased mortality in these patient groups with diabetes complications (adjusted HR: 2.73, 95% CI: 1.38-5.40 and adjusted HR: 2.10, 95% CI: 1.32, 3.35 respectively). Furthermore, the greater risk of mortality in these patients with significant diabetes complications compared to the risk found in the above systematic review suggests that the risk of comorbid depression for mortality may be higher among those with greater severity of disease.
Depression may contribute to negative DM outcomes in several ways. Katon proposed a complex bidirectional relationship between depression and type 2 DM. Depression early in adult life is a risk factor for subsequent development of diabetes. The increased risk of diabetes in patients with depression has been hypothesized to be the result of maladaptive health risk behaviors associated with depression such as smoking, obesity and lack of physical exercise as well as psychobiologic factors such as increased cortisol levels, increased inflammatory factors and insulin resistance. On the other hand, diabetes may increase risk of depression or worsen the depression symptoms due to increased symptom burden, diabetes complications causing functional impairment and decreased quality of life, as well as vascular brain changes secondary to diabetes. Comorbid depression has been found to impair the ability to perform self-care activities necessary to control diabetes by affecting memory, energy level, and executive function. Lack of self-care and the psychobiologic changes associated with comorbid depression may explain why individuals with comorbid depression experience increased risk of macro- and micro-vascular complications and dementia. Two publications allowed examination of whether clinical characteristics (such as severity of diabetes and other medical comorbidity) or health risk behaviors potentially mediated the risk of depression on mortality: Lin et al (33) and Pieper et al (37). When clinical characteristics (such as number of diabetes complications) were added to the models that initially only adjusted for demographic characteristics, there was a decrease in point estimates of the HRs. However, adding covariates related to health risk behaviors (such as smoking, BMI, physical inactivity and HbA1c) into the previous models resulted in little change in the point estimates. This suggests that the mechanism for the relationship between depression and excess mortality in individuals with diabetes may be largely psychobiological. As discussed earlier, because these covariates are not uniform across the studies, head-to-head comparisons are not possible. Further studies are sorely needed to have meaningful conclusion about the mechanism of excess mortality associated with depression in individuals with diabetes.
Prior literature found an approximately 2-fold increase of mortality in patients with comorbid depression and each of the following chronic medical conditions: stroke, coronary heart disease, cancer and COPD. The current meta-analysis and literature support the finding that comorbid depression increases the risk of mortality among those with chronic disease. However, whether depression alone decreases life expectancy is controversial. Reynolds et al reported that depression symptoms reduced total life expectancy significantly, but controlling for chronic diseases eliminated the effect of depression symptoms on mortality across age and gender groups. In contrast, Cuijpers & Smit’s meta-analysis of community studies concluded that having depression increased overall mortality by almost 2-fold. However, their results did not control for lifestyle factors or the presence of chronic conditions.
This systematic review of the literature revealed several major important gaps in knowledge. Although some minority populations experience an increased prevalence of both depression and diabetes, and a disproportionate burden of these illnesses, few epidemiological studies provide conclusive data whether minority populations experience greater mortality burden from comorbid depression and DM compared to other populations. Among the ten studies included in the current analysis, the study by Black and colleagues was the only one that reported the mortality risk associated with comorbid depression and DM in a large aging Hispanic population. They reported a higher risk of mortality associated with depression and diabetes in this population compared to the other studies. However, their study only adjusted for demographic characteristics whereas the other studies also controlled for important other potential confounders including health risk behaviours and disease severity. There are also no studies in developing countries that have examined the risk of comorbid depression in patients with type 2 diabetes. Studies of diverse populations and in developing countries are urgently needed to draw conclusions about potential disparities in mortality burden associated with depression among minority patients with diabetes. Additionally, studies on type 1 diabetes are also needed. DM is a heterogeneous metabolic disease with distinctive aetiology and requirements for disease management. Thus, psychological reactions to onset of disease and burdens of disease may differ between type 1 and type 2 DM. However, both Type 1 and Type 2 DM require constant monitoring and self-management. Depression adversely affects a person’s ability to optimally perform these functions and may increase mortality in individuals with DM regardless of the type. In the current analysis, only Ahola and colleagues’ study examined populations with type 1 diabetes. Other community based or primary care based studies examined populations with type 2 DM only or those where over 90% of the sample were likely to have type 2 DM.
Considering the frequent multi-morbidity found in aging adult populations, early intervention and treatment of depression may be particularly important to improve mortality outcomes. Yet there is limited data about whether screening and treating depression more effectively would decrease pre-mature death associated with DM. A recent report has found that older adults with depression and diabetes who received more effective depression treatment in primary care settings experienced a decrease in 5-year mortality rates compared to those received usual primary care (adjusted HR 0.49, 95% CI 0.24–0.98). However, three other studies that enhanced depression care and improved depressive outcomes compared to usual primary care in patients with diabetes and depression did not find a significant decrease in mortality. This was not an priori hypothesis in these three studies which were likely underpowered to examine mortality outcomes
LIMITATIONS
The results of the current analyses should be interpreted in the context of some limitations. First, despite our best efforts to capture all publications that meet the criteria, we may have missed some studies published in journals that are not indexed in the databases where we conducted searches, those published in non-journal venues, or studies that have not been published. However, our results regarding publication bias suggest that publication bias in very unlikely to have affected our findings. Secondly, we pooled the adjusted HRs from the studies reviewed using different covariates. As seen in Table 1, we categorized covariates into 3 groups. However, each category was defined differently across the studies. Despite the evidence for strong associations between mortality and characteristics such as severity of diabetes, other comorbid conditions, and health behaviors, not all studies adjusted for all these covariates. Such variation in control for potential confounders may have reduced compatibility of the studies and introduced noise into our estimation. Nonetheless, the lack of heterogeneity and negligible differences in the pooled adjusted HRs in the random-effect and fixed-effect models both suggest that these differences in controlling for potential confounders across studies is unlikely to have effected our findings.
CONCLUSION
The results of this meta-analysis provide robust evidence of the adverse impact of comorbid depression on mortality among patients with DM. Large-scale intervention studies are need to test whether decreasing the burden of comorbid depression in patients with type 2 diabetes would decrease mortality rates.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kessler RC, et al. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention . National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2011. [Google Scholar]
- 3.Anderson RJ, et al. The Prevalence of Comorbid Depression in Adults With Diabetes. Diabetes Care. 2001;24(6):1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 4.Li C, et al. Prevalence of depression among U.S. adults with diabetes: findings from the 2006 Behavioral Risk Factor Surveillance System. Diabetes Care. 2008;31:105. doi: 10.2337/dc07-1154. [DOI] [PubMed] [Google Scholar]
- 5.Ali S, et al. The prevalence of co-morbid depression in adults with Type 2 diabetes: a systematic review and meta-analysis. Diabetic Medicine. 2006;23(11):1165–1173. doi: 10.1111/j.1464-5491.2006.01943.x. [DOI] [PubMed] [Google Scholar]
- 6.Ludman EJ, et al. Depression and diabetes symptom burden. General Hospital Psychiatry. 2004;26(6):430–436. doi: 10.1016/j.genhosppsych.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez JS, et al. Depression and Diabetes Treatment Nonadherence: A Meta-Analysis. Diabetes Care. 2008;31(12):2398–2403. doi: 10.2337/dc08-1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Egede LE, Zheng D, Simpson K. Comorbid Depression is Associated With Increased Health Care Use and Expenditures in Individuals With Diabetes. Diabetes Care. 2002;25(3):464–470. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 9.Symons MJ, Moore DT. Hazard rate ratio and prospective epidemiological studies. Journal of Clinical Epidemiology. 2002;55(9):893–899. doi: 10.1016/s0895-4356(02)00443-2. [DOI] [PubMed] [Google Scholar]
- 10.Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003;326(7382):219. doi: 10.1136/bmj.326.7382.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grote NK, et al. A Meta-analysis of Depression During Pregnancy and the Risk of Preterm Birth, Low Birth Weight, and Intrauterine Growth Restriction. Arch Gen Psychiatry. 2010;67(10):1012–1024. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The Nordic Cochrane Centre . Review Manager. The Cochrane Collaboration; Copenhagen: 2008. [Google Scholar]
- 13.Borenstein M, et al. Comprehensive meta-analysis: A computer program for meta-analysis. Biostat Inc; 2007. [Google Scholar]
- 14.Rosenthal R, DiMatteo MR. Meta analysis: Recent developments in quantitative methods for literature reviews. Annual Review of Psychology;Annual Review of Psychology. 2001;52:59–82. doi: 10.1146/annurev.psych.52.1.59. [DOI] [PubMed] [Google Scholar]
- 15.Parmar MKB, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Statistics in Medicine. 1998;17(24):2815–2834. doi: 10.1002/(sici)1097-0258(19981230)17:24<2815::aid-sim110>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 16.Freels S. Extracting summary statistics to perform meta-analysis of the published literature for survival endpoints. Statistics in Medicine. 2004;23(11):1817–1817. doi: 10.1002/(sici)1097-0258(19981230)17:24<2815::aid-sim110>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 17.Spruance SL, et al. Hazard Ratio in Clinical Trials. Antimicrobial Agents and Chemotherapy. 2004;48(8):2787–2792. doi: 10.1128/AAC.48.8.2787-2792.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Michiels S, et al. Meta-analysis when only the median survival times are known: A comparison with individual patient data results. International Journal of Technology Assessment in Health Care. 2005;21(01):119–125. doi: 10.1017/s0266462305050154. [DOI] [PubMed] [Google Scholar]
- 19.Lewis S, Clarke M. Forest plots: trying to see the wood and the trees. BMJ. 2001;322(7300):1479–1480. doi: 10.1136/bmj.322.7300.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 21.Higgins JPT, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thompson SG, Higgins JPT. How should meta-regression analyses be undertaken and interpreted? Statistics in Medicine. 2002;21(11):1559–1573. doi: 10.1002/sim.1187. [DOI] [PubMed] [Google Scholar]
- 23.Wallace B, et al. Meta-Analyst: software for meta-analysis of binary, continuous and diagnostic data. BMC Medical Research Methodology. 2009;9(1):80. doi: 10.1186/1471-2288-9-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Egger M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sterne JAC, Egger M. Funnel plots for detecting bias in meta-analysis: Guidelines on choice of axis. Journal of clinical epidemiology. 2001;54(10):1046–1055. doi: 10.1016/s0895-4356(01)00377-8. [DOI] [PubMed] [Google Scholar]
- 26.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 27.Rosenthal R. The file drawer problem and tolerance for null results. Psychological Bulletin. 1979;86(3):638–641. [Google Scholar]
- 28.Black SA, Markides KS, Ray LA. Depression predicts increased incidence of adverse health outcomes in older Mexican Americans with type 2 diabetes. Diabetes Care. 2003;26(10):2822–8. doi: 10.2337/diacare.26.10.2822. [DOI] [PubMed] [Google Scholar]
- 29.Zhang X, et al. Depressive symptoms and mortality among persons with and without diabetes. Am J Epidemiol. 2005;161(7):652–60. doi: 10.1093/aje/kwi089. [DOI] [PubMed] [Google Scholar]
- 30.Bruce DG, et al. A prospective study of depression and mortality in patients with type 2 diabetes: The Fremantle Diabetes Study. Diabetologia. 2005;48(12):2532–2539. doi: 10.1007/s00125-005-0024-3. [DOI] [PubMed] [Google Scholar]
- 31.Richardson LK, Egede LE, Mueller M. Effect of race/ethnicity and persistent recognition of depression on mortality in elderly men with type 2 diabetes and depression. Diabetes Care. 2008;31(5):880–1. doi: 10.2337/dc07-2215. [DOI] [PubMed] [Google Scholar]
- 32.Katon W, et al. Depression and diabetes: a potentially lethal combination. J Gen Intern Med. 2008;23(10):1571–5. doi: 10.1007/s11606-008-0731-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lin EHB, et al. Depression and Increased Mortality in Diabetes: Unexpected Causes of Death. Ann Fam Med. 2009;7(5):414–421. doi: 10.1370/afm.998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pan A, et al. Increased mortality risk in women with depression and diabetes mellitus. Arch Gen Psychiatry. 2011;68(1):42–50. doi: 10.1001/archgenpsychiatry.2010.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sullivan MD, et al. Depression Predicts All-Cause Mortality. Diabetes Care. 2012 doi: 10.2337/dc11-1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ahola A, et al. Purchase of antidepressant agents by patients with type 1 diabetes is associated with increased mortality rates in women but not in men. Diabetologia. 2012;55(1):73–79. doi: 10.1007/s00125-011-2347-6. [DOI] [PubMed] [Google Scholar]
- 37.Pieper L, et al. Longitudinale Assoziationen zwischen depressiven Symptomen und Typ-2-Diabetes sowie deren Auswirkung auf die Mortalität von Hausarztpatienten. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz. 2011;54(1):98–107. doi: 10.1007/s00103-010-1181-1. [DOI] [PubMed] [Google Scholar]
- 38.Ismail K, et al. A cohort study of people with diabetes and their first foot ulcer: the role of depression on mortality. Diabetes Care. 2007;30(6):1473–1479. doi: 10.2337/dc06-2313. [DOI] [PubMed] [Google Scholar]
- 39.Bot M, et al. Association of Coexisting Diabetes and Depression With Mortality After Myocardial Infarction. Diabetes Care. 2012;35(3):503–509. doi: 10.2337/dc11-1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Katon WJ, et al. The Association of Comorbid Depression With Mortality in Patients With Type 2 Diabetes. Diabetes Care. 2005;28(11):2668–2672. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- 41.Egede LE, Nietert PJ, Zheng D. Depression and all-cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care. 2005;28(6):1339–45. doi: 10.2337/diacare.28.6.1339. [DOI] [PubMed] [Google Scholar]
- 42.Lee T, et al. Mortality Rate in Veterans with Multiple Chronic Conditions. Journal of General Internal Medicine. 2007;22(0):403–407. doi: 10.1007/s11606-007-0277-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rosenthal MJ, et al. Hospitalization and Mortality of Diabetes in Older Adults: A 3-year prospective study. Diabetes Care. 1998;21(2):231–235. doi: 10.2337/diacare.21.2.231. [DOI] [PubMed] [Google Scholar]
- 44.Black SA, Markides KS. Depressive symptoms and mortality in older Mexican Americans. Ann Epidemiol. 1999;9(1):45–52. doi: 10.1016/s1047-2797(98)00025-8. [DOI] [PubMed] [Google Scholar]
- 45.Prisciandaro JJ, et al. Impact of psychiatric comorbidity on mortality in veterans with type 2 diabetes. Diabetes Technol Ther. 2011;13(1):73–8. doi: 10.1089/dia.2010.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reynolds SL, Haley WE, Kozlenko N. The Impact of Depressive Symptoms and Chronic Diseases on Active Life Expectancy in Older Americans. American Journal of Geriatric Psych. 2008;16(5):425–432. doi: 10.1097/JGP.0b013e31816ff32e. 10.1097/JGP.0b013e31816ff32e. [DOI] [PubMed] [Google Scholar]
- 47.Gallo JJ, et al. Depression, cardiovascular disease, diabetes, and two-year mortality among older, primary-care patients. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2005;13(9):748–755. doi: 10.1176/appi.ajgp.13.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bogner HR, et al. Diabetes, depression, and death: a randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT) Diabetes Care. 2007;30(12):3005–3010. doi: 10.2337/dc07-0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Landman GWD, et al. Health-Related Quality of Life and Mortality in a General and Elderly Population of Patients With Type 2 Diabetes (ZODIAC-18) Diabetes Care. 2010;33(11):2378–2382. doi: 10.2337/dc10-0979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Milano A, Singer R. Mortality in co-morbidity (II)--excess death rates derived from a follow-up study on 10,025 subjects divided into 4 groups with or without depression and diabetes mellitus. J Insur Med. 2007;39(3):160–6. [PubMed] [Google Scholar]
- 51.Stroup DF, et al. Meta-analysis of Observational Studies in Epidemiology. JAMA: The Journal of the American Medical Association. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 52.Pan A, et al. Increased mortality risk in women with depression and diabetes mellitus. Archives of General Psychiatry. 2011;68(1):42–50. doi: 10.1001/archgenpsychiatry.2010.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Duval S, Tweedie R. Trim and Fill: A Simple Funnel-Plot–Based Method of Testing and Adjusting for Publication Bias in Meta-Analysis. Biometrics. 2000;56(2):455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 54.Carson KP, Schriesheim CA, Kinicki AJ. The Usefulness of the “Fail-Safe” Statistic in Meta-Analysis. Educational and Psychological Measurement. 1990;50(2):233–243. [Google Scholar]
- 55.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66(6):802–13. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 56.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biological Psychiatry. 2003;54(3):216–226. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- 57.Golden S, et al. Examining a bidirectional association between depressive symptoms and diabetes. Jama. 2008;299:2751. doi: 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stuart MJ, Baune BT. Depression and type 2 diabetes: Inflammatory mechanisms of a psychoneuroendocrine co-morbidity. Neuroscience & Biobehavioral Reviews. 2012;36(1):658–676. doi: 10.1016/j.neubiorev.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 59.Silva N, Atlantis E, Ismail K. A review of the association between depression and insulin resistance: pitfalls of secondary analyses or a promising new approach to prevention of type 2 diabetes? Curr Psychiatry Rep. 2012;14(1):8–14. doi: 10.1007/s11920-011-0245-8. [DOI] [PubMed] [Google Scholar]
- 60.de Groot M, et al. Association of Depression and Diabetes Complications: A Meta-Analysis. Psychosomatic Medicine. 2001;63(4):619–630. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 61.Katon W, L.C.R., Parker M, Karter AJ, Huang ES, Whitmer RA. Association of depression with increased risk of dementia in patients with type 2 diabetes: The diabetes and aging study. Archives of General Psychiatry. 2012;69(4):410–417. doi: 10.1001/archgenpsychiatry.2011.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pan A, et al. Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA. 2011;306(11):1241–9. doi: 10.1001/jama.2011.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pinquart M, Duberstein PR. Depression and cancer mortality: a meta-analysis. Psychological Medicine. 2010;40(11):1797–1810. doi: 10.1017/S0033291709992285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.de Voogd JN, et al. Depressive symptoms as predictors of mortality in patients with COPD. Chest. 2009;135(3):619–25. doi: 10.1378/chest.08-0078. [DOI] [PubMed] [Google Scholar]
- 65.Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. Journal of Affective Disorders. 2002;72(3):227–236. doi: 10.1016/s0165-0327(01)00413-x. [DOI] [PubMed] [Google Scholar]
- 66.Akincigil A, et al. Racial and Ethnic Disparities in Depression Care in Community-Dwelling Elderly in the United States. American Journal of Public Health. 2011;102(2):319–328. doi: 10.2105/AJPH.2011.300349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bhugra D, Jones P. Migration and mental illness. Adv Psychiatr Treat. 2001;7(3):216–222. [Google Scholar]
- 68.McBean AM, et al. Differences in Diabetes Prevalence, Incidence, and Mortality Among the Elderly of Four Racial/Ethnic Groups: Whites, Blacks, Hispanics, and Asians. Diabetes Care. 2004;27(10):2317–2324. doi: 10.2337/diacare.27.10.2317. [DOI] [PubMed] [Google Scholar]
- 69.Katon W, et al. The pathways study: A randomized trial of collaborative care in patients with diabetesand depression. Archives of General Psychiatry. 2004;61(10):1042–1049. doi: 10.1001/archpsyc.61.10.1042. [DOI] [PubMed] [Google Scholar]
- 70.Ell K, et al. Collaborative Care Management of Major Depression Among Low-Income, Predominantly Hispanic Subjects With Diabetes: A randomized controlled trial. Diabetes Care. 2010;33(4):706–713. doi: 10.2337/dc09-1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Williams JW, Jr., et al. The effectiveness of depression care management on diabetes-related outcomes in older patients. Ann Intern Med. 2004;140(12):1015–24. doi: 10.7326/0003-4819-140-12-200406150-00012. [DOI] [PubMed] [Google Scholar]