Abstract
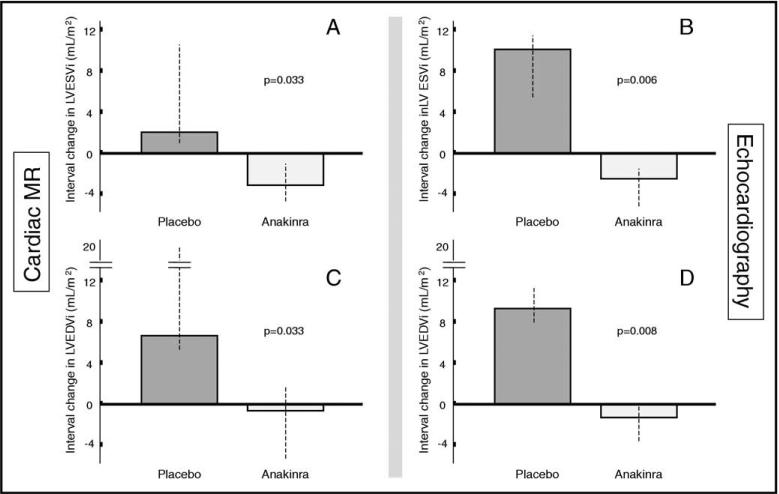
Acute myocardial infarction (AMI) initiates an intense inflammatory response in which interleukin-1 (IL-1) plays a central role. The IL-1 receptor antagonist is a naturally occurring antagonist, and anakinra is the recombinant form used to treat inflammatory diseases. The aim of the present pilot study was to test the safety and effects of IL-1 blockade with anakinra on left ventricular (LV) remodeling after AMI. Ten patients with ST-segment elevation AMI were randomized to either anakinra 100 mg/day subcutaneously for 14 days or placebo in a double-blind fashion. Two cardiac magnetic resonance (CMR) imaging and echocardiographic studies were performed during a 10- to 14-week period. The primary end point was the difference in the interval change in the LV end-systolic volume index (LVESVi) between the 2 groups on CMR imaging. The secondary end points included differences in the interval changes in the LV end-diastolic volume index, and C-reactive protein levels. A +2.0 ml/m2 median increase (interquartile range +1.0, +11.5) in the LVESVi on CMR imaging was seen in the placebo group and a –3.2 ml/m2 median decrease (interquartile range –4.5, –1.6) was seen in the anakinra group (p = 0.033). The median difference was 5.2 ml/m2. On echocardiography, the median difference in the LVESVi change was 13.4 ml/m2 (p = 0.006). Similar differences were observed in the LV end-diastolic volume index on CMR imaging (7.6 ml/m2, p = 0.033) and echocardiography (9.4 ml/m2, p = 0.008). The change in C-reactive protein levels between admission and 72 hours after admission correlated with the change in the LVESVi (R =+0.71, p = 0.022). In conclusion, in the present pilot study of patients with ST-segment elevation AMI, IL-1 blockade with anakinra was safe and favorably affected by LV remodeling. If confirmed in larger trials, IL-1 blockade might represent a novel therapeutic strategy to prevent heart failure after AMI.
Acute myocardial infarction (AMI) initiates an intense inflammatory response characterized by an accumulation of leukocytes in the injured myocardium and the production of cytokines and chemokines, which further promotes adverse cardiac remodeling and heart failure.1–3 Interleukin-1 (IL-1) is the prototypic inflammatory cytokine, inducing adhesion molecules and chemokines.4 IL-1 is also a known myocardial suppressant.4–5 In AMI, IL-1 is initially released by the ischemic endothelial cells and cardiomyocytes and, later, by the leukocytes infiltrating the myocardium.6 Although IL-1 leads to leukocyte recruitment, which contributes to infarct healing, IL-1 also promotes cell death in cardiomyocytes.6,7 The naturally occurring IL-1 receptor antagonist binds to the IL-1 receptor and prevents IL-1 activity.4 We have reported that a recombinant human IL-1 receptor antagonist, anakinra, ameliorated cardiac remodeling after a large anterior wall AMI in the experimental mouse model and improved survival.7 Moreover, mice with deletion of the IL-1 type I receptor were protected from adverse cardiac remodeling,8 demonstrating the critical role of IL-1 activity in AMI. We designed and conducted a randomized double-blind pilot trial comparing anakinra and placebo to test the hypothesis that IL-1 blockade would be safe and lead to more favorable left ventricular (LV) remodeling in patients with ST-segment elevation AMI.
Methods
The study design was registered at the ClinicalTrials.gov Website (National Clinical Trial no. 00789724). An exemption for investigational new drug use was allowed by the Food and Drug Administration according to the current regulations [Code of Federal Regulations 312.2(b)]. The Virginia Commonwealth University institutional review board approved the study, and all patients provided written consent. Starting on November 16, 2008, consecutive patients presenting to our institution with suspected ST-segment elevation AMI were screened for enrollment (Figure 1). The inclusion criteria were age >18 years, acute (<24 hours) onset of chest pain, new or presumably new ST-segment elevation (>1 mm) in ≥2 anatomically contiguous leads, and planned or completed angiography for urgent percutaneous coronary intervention. The exclusion criteria were a lack of informed consent; unsuccessful percutaneous revascularization or the need for urgent surgical revascularization; hemodynamic instability requiring the use of an intra-aortic balloon pump; dopamine, dobutamine, norepinephrine, or epinephrine infusions; pre-existing congestive heart failure stage C/D, New York Heart Association class IV; severe LV dysfunction (LV ejection fraction <20%) or severe aortic or mitral valve disease; contraindications to magnetic resonance imaging; pregnancy; chronic autoinflammatory or autoimmune disease; severe asthma; severe coagulopathy (international normalized ratio >2.0 or platelet count <50,000/mm3); or recent (<14 days) use of anti-inflammatory drugs (nonsteroidal anti-inflammatory drugs excluded).
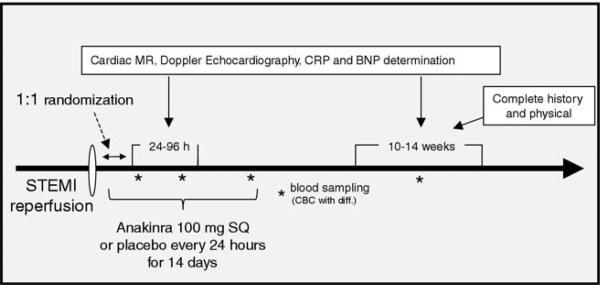
Figure 1.
Schematic diagram of study design. BNP = brain-type natriuretic peptide; CBC = complete blood cell count; CRP = C-reactive protein; MR = magnetic resonance; SQ = subcutaneous.
Randomization was performed by the investigational pharmacist using a dedicated randomization algorithm (available on-line at www.metcardio.org). The investigator in charge of randomization was not involved in patient care, data gathering, or data analysis. Anakinra (Amgen, Thousand Oaks, California) was purchased from the investigational pharmacy. For each patient, the pharmacist prepared a set of 14 syringes containing 100 mg of anakinra in 0.67 ml or matching syringes containing sodium chloride 0.9% placebo that were indistinguishable from the treatment syringes. Treatment consisted of 14 daily subcutaneous injections. The patients were monitored in the intensive care unit for >48 hours and were assessed daily for adverse treatment effects. A complete blood cell count was obtained at admission and daily for 4 days. A group of consultants (see Appendix) was available to the investigators to provide advice regarding potential adverse effects.
A cardiac magnetic resonance (CMR) study and Doppler echocardiography were performed 24 to 96 hours after admission and 10 to 14 weeks later. High-sensitivity C-reactive protein and brain-type natriuretic peptide were measured at 72 hours, 14 days, and 10 to 14 weeks. Serial cardiac markers were obtained, as clinically indicated. Clinical follow-up was performed in-hospital until discharge and then at the Cardiology Research Clinic at day 14 and 10 to 14 weeks later.
The primary end point was the difference in interval changes in the LV end-systolic volume index (LVESVi) assessed by CMR imaging from baseline to follow-up, comparing the anakinra- and placebo-treated patients. The secondary end points included the difference in interval changes in the LVESVi, as assessed by echocardiography, and the interval changes in the LV end-diastolic volume index, LV ejection fraction, LV mass, infarct size, wall motion score index, and estimated cardiac index, as assessed by CMR or echocardiography. The CMR studies were obtained in the Virginia Commonwealth University Cardiac Magnetic Resonance Imaging suite using a Siemens Avanto 1.5 Tesla magnet (Munich, Germany). After the initial localizer sequences in the transverse, frontal, and sagittal planes, contiguous 6-mm steady-state free precession cine images with 2-mm gaps were obtained from the mitral valve ring though the cardiac apex.9 The LV endsystolic volume, LV end-diastolic volume, and LV ejection fraction were computed by tracing the endocardial and epicardial LV contours in systole and diastole using this stack of 10 to 12 short-axis slices. Gadolinium was then administered through a peripheral intravenous line. To visualize the areas of infarction and no reflow, late gadolinium enhancement imaging was performed, beginning 10 minutes after contrast administration using a standard segmented inversion recovery gradient echo sequence in the short-axis plane at locations that spatially matched the cine acquisitions. The infarct size was calculated using a 17-segment model with the degree of transmurality graded by quartiles (0 to 4 scale). Partial volume effects were evaluated using a grading scale (0 to 4) for the visual intensity of enhancement. A value of 4 was assigned to the brightest region of enhancement and 0 to remote myocardium. Echocardio-graphic studies were obtained using an HP Phillips Sonos 5500 (Andover, Massachusetts) or IE33 apparatus with dual harmonic imaging and short- and long-axis views, as recommended by the American Society of Echocardiography.10 The LV end-systolic volume, LV end-diastolic volume, and LV ejection fraction were computed in the apical 4- and 2-chambers views over multiple cycles, using the modified Simpson formula.10 The wall motion score index was calculated as the ratio of the sum of the score from each of 16 segments using standard scoring recommendations divided by the total number of segments.10 Transmitral flow and LV outflow tract flow Doppler spectra and the annular tissue Doppler spectra were obtained from the apical window, and the cardiac index was calculated. All measurements and calculations were performed at the end of the study jointly by 2 investigators, who were unaware of the patient treatment, and decisions were made in consensus. The white blood cell count, brain-type natriuretic peptide, troponin I, creatine kinase-MB, creatinine, and other routine tests and measurements were performed in the Virginia Commonwealth University Health System Pathology Laboratories. The determination of the high-sensitivity C-reactive protein levels was performed by LabCorp (Burlington, North Carolina) using high-sensitivity rate nephelometry.
Given the limited funding for the present pilot study, we chose a sample size of 10 patients to provide >50% power to detect an estimated average intergroup difference in LVESVi ≥4 ml/m2, with an anticipated SD of ≤6 ml/m2 and an α of 0.05. Statistical analyses were conducted in a blinded fashion. At study completion, one investigator was made aware of the allocation to group 1 or 2, but without knowledge of the treatment received. Once the analyses were completed, the randomization code was opened and made available to all the investigators. The values are reported as the median and interquartile range for potential deviation from the gaussian distribution. The differences between the 2 groups were computed using the Wilcoxon test for continuous variables or Fisher's exact test for discrete variables. The differences in interval changes between the 2 groups were compared using random-effect analysis of variance for repeated measures to analyze the effects of time and group allocation. The Spearman correlation test was used to evaluate the correlation between the 2 variables. Unadjusted p values are reported throughout, with statistical significance set at the 2-tailed 0.05 level. The analyses were completed using the Statistical Package for Social Sciences, version 11.0.1, software (SPSS, Chicago, Illinois).
Results
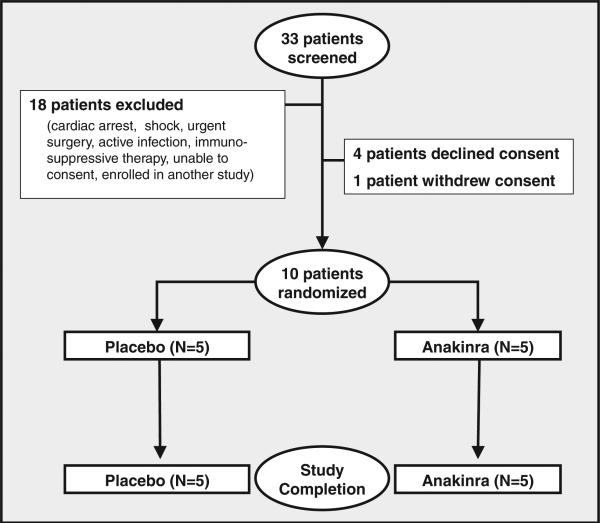
Enrollment started in November 2008. During the first 4 months, 33 patients were admitted with ST-segment elevation AMI and screened, and 10 patients were enrolled (Figure 2). One patient withdrew consent to the study on day 2 before all assessments had been completed and was excluded. The institutional review board then approved enroll ment of an additional patient, who was enrolled in May 2009. The demographic and clinical characteristics of the patients are summarized in Table 1. No significant differences in age, gender, ethnicity, risk factors, or clinical characteristics were present between the 2 groups. The interval from admission to the CMR study was not signficantly different statistically between the 2 groups (47 hours, range 41 to 85, vs 54 hours, range 50 to 77) for anakinra and placebo, respectively (p = 0.8). The infarct size at late gadolinium enhancement on CMR imaging was 15.4% in the anakinra group and 14.3% in the placebo group (p = 0.39), and the size of no-reflow was small in both groups (0% and 1.3% for the anakinra and placebo groups, respectively; p = 0.44). All patients were discharged with aspirin 325 mg/day, clopidogrel 75 mg/day, metoprolol 25 to 150 mg/day (or equivalent), fosinopril 2.5 to 40 mg/day (or equivalent), atorvastatin 10 to 80 mg/day (or equivalent), with no significant differences in the dosages between the 2 groups.
Figure 2.
Schematic diagram of enrollment process.
Table 1.
Demographic and clinical characteristics
| Pt. No. | Age (yrs) | Gender | Ethnicity | Hypertension | Diabetes | Time From Chest Pain to PCI (min) |
Time From Chest Pain to Drug (min) |
Thrombolysis (Before PCI) |
CAD (culprit) |
CAD (other) |
TIMI Flow (Initial) |
TIMI Flow (Final) |
Coronary Stenting |
Infarct Size (%) |
Adverse Clinical Events | LVESVi (Admission) |
LVESVi (Follow-Up) |
Change in LVESVi (ml/m2) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Placebo | ||||||||||||||||||
| 1 | 60 | M | W | Y | N | 75 | 289 | N | RCA | N | 1 | 3 | Y | 5.0 | Acute coronary syndrome; Femoral artery pseudoaneurysm | 12.0 | 23.5 | + 11.5 |
| 3 | 28 | M | W | N | N | 664 | 1020 | Y | RCA | N | 2 | 3 | Y | 14.3 | None | 21.0 | 23.0 | +2.0 |
| 5 | 65 | M | B | Y | Y | 264 | 515 | Y | LAD | RCA | 0 | 3 | Y | 25.8 | Heart failure | 29.0 | 28.5 | –0.5 |
| 6 | 53 | M | W | N | N | 115 | 480 | N | RCA | LCX | 1 | 3 | Y | 7.1 | Unstable angina | 41.5 | 42.5 | +1.0 |
| 8 | 45 | M | B | Y | N | 139 | 390 | N | LCX | RCA | 0 | 3 | Y | 19.4 | Heart failure, atypical chest pain | 41.5 | 61.5 | +20.0 |
| Anakinra | ||||||||||||||||||
| 2 | 59 | M | W | Y | Y | 64 | 453 | N | LCX | LAD RCA | 0 | 3 | Y | 12.1 | None | 42.5 | 34.5 | –8.0 |
| 7 | 35 | F | W | Y | Y | 415 | 732 | N | LCX | N | 1 | 3 | N | 27.0 | None | 48.5 | 47.0 | –1.5 |
| 9 | 59 | M | W | Y | N | 192 | 470 | N | RCA | LAD | 1 | 3 | Y | 13.7 | None | 24.5 | 21.5 | –3.0 |
| 10 | 40 | M | W | Y | N | 267 | 472 | Y | RCA | N | 3 | 3 | Y | 25.8 | Injection site pain | 52.5 | 48.0 | –4.5 |
| 11 | 34 | F | W | Y | N | 140 | 583 | N | LAD | LCX | 0 | 3 | Y | 15.4 | Acute coronary syndrome, injection site pain | 31.0 | 29.5 | –1.5 |
B = black; W = white; CAD = coronary artery disease; F = female; LAD = left anterior descending (artery); LCX = left circumflex (artery); M = male; N = no; PCI = percutaneous coronary intervention; RCA = right coronary artery; TIMI = Thrombolysis In Myocardial Infarction; Y = yes.
All patients were alive at the 10- to 14-week follow-up visit. Adverse clinical events are listed in Table 1. Two patients (both in the anakinra group) reported injection site pain; one of whom required analgesics and topical steroids. No patients experienced systemic side effects. At follow-up, a +2.0 ml/m2 median increase (interquartile range +1.0 to +11.5) was seen in the LVESVi in the placebo group and a –3.2 ml/m2 median decrease (interquartile range –4.5 to –1.6) in the anakinra group (p = 0.033), with a median difference of 5.2 ml/m2 in the LVESVi change between the 2 groups (primary end point, Figure 3; Table 1 and Table 2). The LVESVi measurements by echocardiography correlated highly with the measurements by CMR imaging (R = +0.91, p <0.001), with a relative underestimation of volumes with echocardiography. By echocardiography, anakinra-treated patients had a –2.7 ml/m2 (interquartile range –4.5 to –1.8) decrease in LVESVi compared to a +10.7 ml/m2 (interquartile range +4.2 to +11.2) increase in the placebo group (p = 0.006), leading to a median difference of 13.4 ml/m2 between the 2 groups (Figure 3 and Table 1). Similar trends were noted in the LV end-diastolic volume index by CMR imaging (median difference 7.6 ml/m2, p = 0.033) and echocardiography (median difference 9.4 ml/m2, p = 0.008; Figure 3 and Table 1). The LV ejection fraction remained unchanged over time by CMR (median change 0% in both groups). In contrast, by echocardiography, a trend was seen toward a mild LV ejection fraction reduction in the placebo group (–3%, interquartile range –3 to –10), with no change in the anakinra group (0%, interquartile range 0 to +6, p = 0.070). No significant changes in LV mass were noted in either group. The infarct size at late gadolinium enhancement was reduced in both groups by approximately 20%, without any difference between the 2 groups. However, a trend was seen toward a more favorable change in the wall motion score index in the anakinra group (–0.25, interquartile range –0.27 to –0.06) compared to the placebo group (0, interquartile range –0.06 to +0.06, p = 0.068). No significant differences were seen in the changes in transmitral Doppler spectra and/or tissue Doppler spectra between the 2 groups. A significant difference in the changes in the cardiac index was noted, with a –0.5 L/min/m2 (interquartile range –0.4 to –0.7) reduction in the placebo-treated group and a –0.1 L/min/m2 (interquartile range 0 to –0.1) reduction in the anakinra-treated group (p = 0.029). The blood pressure values were not significantly different statistically between the 2 groups and were unaffected by treatment (data not shown).
Figure 3.
LV remodeling. (A,B) Median interval changes in LVESVi in placebo and anakinra groups assessed by CMR imaging and echocardiography, respectively. (C,D) Median interval changes in LV end-diastolic volume index (LVEDVi) in placebo and anakinra groups as assessed by CMR imaging and echocardiography, respectively.
Table 2.
Cardiac dimensions and function
| Variable | Placebo |
Anakinra |
Median Difference (vs Placebo) | p Value | ||
|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Baseline | Follow-Up | |||
| Cardiac magnetic resonance imaging | ||||||
| Left ventricular end-systolic volume index (ml/m2) | 29.0 (21.0–41.4) | 28.5 (23.5–42.4) | 42.5 (31.1–48.5) | 34.5 (29.5–47.0) | –5.2 | 0.033* |
| Left ventricular end-diastolic volume index (ml/m2) | 64.5 (61.0–73.8) | 69.5 (66.0–81.0) | 73.0 (61.0–85.9) | 68.4 (67.5–75.5) | –7.6 | 0.033* |
| Left ventricular ejection fraction (%) | 53.0 (45.0–66.0) | 56.0 (48.0–57.0) | 49.0 (39.0–53.0) | 53.0 (47.0–55.0) | 0.0 | 0.26 |
| Left ventricular mass (g) | 182.0 (162.0–183.0) | 155.0 (152.0–176.0) | 130.0 (94.0–148.0) | 132.0 (100.0–146.0) | +14.0 | 0.17 |
| Echocardiography | ||||||
| Left ventricular end-systolic volume index (ml/m2) | 20.0 (10.5–27.0) | 26.0 (20.2–30.7) | 26.2 (22.6–27.3) | 24.5 (15.8–27.3) | –13.4 | 0.006* |
| Left ventricular end-diastolic volume index (ml/m2) | 44.0 (31.2–46.0) | 46.8 (39.8–55.5) | 49.5 (31.2–54.0) | 49.5 (37.4–49.8) | –9.4 | 0.008* |
| Left ventricular ejection fraction (%) | 55.0 (41.0–66.0) | 45.0 (44.0–48.0) | 45.0 (36.0–51.0) | 51.0 (45.0–58.0) | +3.0 | 0.07 |
| Wall motion score index | 1.19 (1.13–1.38) | 1.25 (1.25–1.38) | 1.47 (1.44–1.67) | 1.40 (1.19–1.47) | –0.25 | 0.07 |
| Cardiac index (L/min/m2) | 2.32 (2.28–2.65) | 1.70 (1.65–2.30) | 2.12 (1.86–2.40) | 2.07 (2.03–2.08) | +0.42 | 0.03* |
Data are presented as median (interquartile range).
Statistically significant.
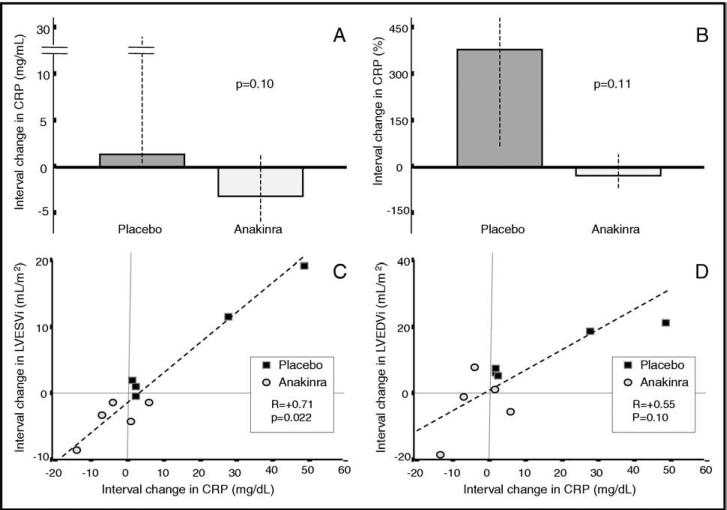
Although the white blood cell counts were not significantly different statistically between the 2 groups at baseline, the anakinra-treated patients had significantly lower counts 24 hours after the first injection compared to the placebo-treated patients (5,500/mm3, range 5,100 to 7,200, vs 8,900/mm3, range 8,300 to 10,400; p = 0.025). Similarly, the absolute neutrophil counts at 24 hours after the first injection were lower in the anakinra-treated patients (3,800/mm3, range 3,520 to 4,970, vs 6,150/mm3, range 5,730 to 7,180; p = 0.025). The C-reactive protein levels were significantly greater at admission in the patients who were then randomized to anakinra (15.4 mg/dl, range 13.0 to 16.6) compared to those randomized to placebo (2.3 mg/dl, range 1.9 to 2.7; p = 0.036). The interval change in C-reactive protein levels between admission and 72 hours showed a trend toward a decrease in the anakinra-treated patients (–21%) and an increase in the placebo group (+373%), although this difference was not statistically significant (p = 0.11; Figure 4). Nevertheless, the change in C-reactive protein levels during the 72 hours correlated with the change in the LVESVi (R = +0.71, p = 0.022) and the LV end-diastolic volume index (R = +0.55, p = 0.10) by CMR at 10 to 14 weeks (Figure 4). All but 2 patients (both in the anakinra group) had brain-type natriuretic peptide levels <200 pg/ml at admission, and all patients had brain-type natriuretic peptide levels <200 pg/ml at 14 days of follow-up. No difference was found in the changes in brain-type natriuretic peptide levels between the 2 groups.
Figure 4.
C-reactive protein changes and LV remodeling. (A,B) Median interval changes in C-reactive protein plasma levels 72 hours after admission, expressed as absolute change (mg/dl) or percentage, respectively. (C,D) Correlation between interval change in C-reactive protein plasma levels 72 hours after admission and interval change in LVESVi and LV end-diastolic volume index (LVEDVi) by CMR imaging, respectively.
Discussion
The present study has demonstrated, for the first time, that IL-1 blockade with anakinra is safe and ameliorates LV remodeling in patients with ST-segment elevation AMI. AMI is the leading cause of heart failure in the United States, and the prevention of adverse cardiac remodeling after AMI is among the major challenges.2–3,11–12 Clinical trials in the past 30 years have shown that adverse cardiac remodeling and mortality can be reduced using reperfusion or neurohormonal blockade.13–19 The inflammatory response during AMI is another major determinant of adverse cardiac remodeling, heart failure, and death.6 The complexity of the inflammatory cascade and the lack of specific intervention, however, have delayed the use of effective anti-inflammatory treatment in ST-segment elevation AMI. IL-1 plays a central role in the interplay among different cell types and soluble mediators, because the cytokine amplifies the local and systemic inflammatory response by orders of magnitude.4 Early in AMI, IL-1 can be released from activated platelets and resident macrophages, exerting direct inflammatory effects on the endothelium and myocardium.6,20 The IL-1 receptor antagonist is a naturally occurring IL-1 antagonist secreted by the same cells that produces IL-1.4 Mice lacking the gene coding for the IL-1 receptor antagonist experience greater damage during experimental AMI.9 In contrast, overexpression of the IL-1 receptor antagonist in a transgenic mouse will lead to increased resistance to myocardial ischemic injury.21 In the mouse and rat, we have reported that the administration of anakinra reduced the enlargement of the left ventricle after AMI.7 In addition, we observed a survival benefit, without any indication of impaired infarct healing.7 From these results, we designed the current Virginia Commonwealth University Anakinra Remodeling Trial (VCU-ART) pilot study.
Despite the small number of patients studied and the need for validation in larger cohorts, the data from the present pilot study have indicated that IL-1 blockade with anakinra is safe and can favorably affect cardiac remodeling (LVESVi) after ST-segment elevation AMI, without affecting the infarct size or infarct healing. LVESVi is a strong and independent surrogate end point for heart failure mortality.22,23 The median difference in LVESVi change, 5 ml/m2 by CMR imaging and 12 ml/m2 by echocardiography, was comparable to the effects noted with other treatments associated with clear survival benefits, such as reper-fusion,13 angiotensin-converting enzyme inhibition,14 and β-adrenergic blockade.15 The beneficial effects on LVESVi were paralleled by a similar effect in the changes in the LV end-diastolic volume index and cardiac index, and were evident despite concomitant therapy with angiotensin-converting enzyme inhibitors, β-adrenergic blockers, and hydroxyl-methyl-co-enzyme A-reductase inhibitors in all patients. These observations also indicate that the myocardium in patients after ST-segment elevation AMI is exquisitely sensitive to the inflammatory and suppressive properties of IL-1. Given a dose of 100 mg of anakinra, the maximum daily blood level was <1 μg/ml, likely leading to incomplete IL-1 receptor blockade.
The present study had several potential drawbacks. First, it included a small number of patients. Second, we lacked true baseline acquisition of the imaging studies, which were obtained 24 to 96 hours (median 49) after admission and, therefore, did not account for early changes in size and contractility. Third, although no statistically significant differences were found in the baseline characteristics between the 2 groups, the statistical power was limited to determine differences. Therefore, an effect of prerandomization imbalance between the 2 groups could not be excluded. Finally, a small number of patients were enrolled, which did not allow us to detect effects on clinical outcome. A larger clinical study of anakinra versus placebo in patients with non–ST-segment elevation AMI is currently ongoing in the United Kingdom.24
From a safety standpoint, the study results have been reassuring and in keeping with the data on anakinra use.25 Two patients experienced injection site reactions during the last few days of treatment, but both were able to complete the 14-day course. The reactions resolved within few days, without long-term consequences.
A recent study of patients with rheumatoid arthritis showed that anakinra increased the coronary flow reserve parallel with a significant reduction in C-reactive protein.26 Owing to the small number of patients or perhaps because of a different inciting event, we did not observe a significant reduction in C-reactive protein. Nevertheless, a significant correlation was seen between the C-reactive protein changes and LV remodeling.27 Finally, variability exists in the inflammatory response among patients. Hence, in terms of reducing IL-1 activity, “a one size fits all” approach might be less than ideal, and the individual patient might require a tailored dose and duration of IL-1 blockade.
Acknowledgments
This study was funded by a Virginia Commonwealth University “A.D. Williams Fund” grant to Dr. Abbate and a Virginia Commonwealth University General Clinical Research Center Funds for Pilot Clinical Research to Dr. Abbate, and by the VCU Pauley Heart Center funds (Richmond, Virginia).
Appendix
VCU-ART Investigators: Principal Investigator: A. Abbate, MD, PhD; Research coordinators: L. M. Roach, RN, A. Dziekonski, RN, D. W. Spillman, RN; Clinical Investigators: M. C. Kontos, MD, J. D. Grizzard, MD, R. Arena, MD, J. K. Fredenberger, RDCS, C. C. Gelwix, MD, B. Grant, RDCS, C. Guard, RDCS, E. Goudreau, MD, A. Hastillo, MD, K. Lotun, MD, V. Marwaha, MD, R. Robati, MD, C. S. Roberts, NP, B. W. Van Tassell, PharmD, A. Varma, MD, G. W. Vetrovec, MD, M. Zacharias, CS; Clinical consultants: C. A. Dinarello, MD, M. A. Peberdy, MD, L. M. Buckley, MD, C. E. Grossman, MD, G. Kalahasty, MD, J. T. Kushinka, MD, R. Mannino, MD, W. N. Roberts; Nursing Staff: Nurse Practitioners—S. H. Alexander, NP, C. M. Bateman, NP, V. Green, NP, E. K. Grubbs, NP, D. Hannah, NP, M. K. Jarrett, NP, P. M. McMahon, NP, A. P. Rusnak, NP, D. Yuskis, NP; Coronary Intensive Care Unit—M. Altman, RN, C. Baron, RN, D. Baldwin, RN, J. Battista, RN, D. Bull, RN, K. Casey, RN, E. Criswell, RN, S. Dettbarn, RN, D. Finck, RN, R. Gunn, RN, B. Hall, RN, J. Hutton, RN, J. Jackson, RN, D. Javier, RN, L. Keilholtz, RN, D. Legg, RN, E. Lute, RN, A. McRae, RN, B. Molchan, RN, K. Mullin, RN, L. Nelson, RN, H. Noble, RN, H. Olson, RN, T. Onyenweaku, RN, K. Patterson, RN, S. Phillips, RN, J. Powers, RN, M. Ragsdale, RN, C. Ray, RN, J. Rice, RN, R. Robertson, RN, L. Seek, RN, L. Snodgrass, RN, A. Spradlin, RN, J. Thomas, RN, M. Urmaza, RN, J. Walker, RN, C. Wheeler, RN, C. Wright, RN, A. Wise, RN; Step Down Unit—C. Eriksson, RN, E. Anderson, RN, L. Anderson, RN, J. Arledge, RN, E. Banton, RN, A. Barrett, RN, T. Bowman, RN, C. Buck, RN, C. Burrell, RN, K. Burrow, RN, M. Cohan, RN, C. DeWilde, RN, R. Diehl, RN, C. Fleshman, RN, L. Franklin, RN, T. Guyton, RN, K. Harris, RN, A. Hill, RN, E. Hulburt, RN, D. Hunt, RN, P. Kaur, RN, A. Knapstein, RN, A. Lackey, RN, M. Langford, RN, R. Lavine, RN, K. Lee, RN, J. Lemmons, RN, D. McCormick, RN, A. McMillan, RN, T. Moseley, RN, B. Neville, RN, A. Petrohovich, RN, J. Poarch, RN, Y. Salih, RN, S. Snider, RN, C. Solomon, RN, I. Tarasova, RN, M. Taylor, RN, E. Vick, RN, K. Wells, RN, A. Wildrick, RN, K. Williams, RN, M. Williamson, RN, C. Yi, RN; Investigational Pharmacy: R. Sculthorpe, PharmD, N. Ntabazi, PharmD; Study Design and Statistical Consultant: G. G. L. Biondi-Zoccai, MD, L. R. Thacker, PhD; Research Laboratory Personnel: F. N. Salloum, PhD, I. M. Seropian, MD, M. Smith, BS, S. Toldo, PhD.
References
- 1.Frangogiannis N. The immune system and cardiac repair. Pharmacol Rev. 2008;58:88–111. doi: 10.1016/j.phrs.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Velagaleti R, Pencina M, Murabito J, Wang T, Parikh N, D'Agostino R, Levy D, Kannel W, Vasan R. Long-term trends in the incidence of heart failure after myocardial infarction. Circulation. 2008;118:2057–2062. doi: 10.1161/CIRCULATIONAHA.108.784215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldberg R, Spencer F, Yarzebski J, Lessard D, Gore J, Alpert J, Dalen JA. 25-Year perspective into the changing landscape of patients hospitalized with acute myocardial infarction (the Worcester Heart Attack Study). Am J Cardiol. 2004;94:1373–1378. doi: 10.1016/j.amjcard.2004.07.142. [DOI] [PubMed] [Google Scholar]
- 4.Dinarello C. Immunological and inflammatory functions of the interleukin-1 family. Annu Rev Immunol. 2009;27:519–550. doi: 10.1146/annurev.immunol.021908.132612. [DOI] [PubMed] [Google Scholar]
- 5.Pomerantz BJ, Reznikov LL, Harken AH, Dinarello CA. Inhibition of caspase 1 reduces human myocardial ischemic dysfunction via inhibition of IL-18 and IL-1beta. Proc Natl Acad Sci U S A. 2001;98:2871–2876. doi: 10.1073/pnas.041611398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bujak M, Frangogiannis N. The role of IL-1 in the pathogenesis of heart disease. Arch Immunol Ther Exp. 2009;57:165–176. doi: 10.1007/s00005-009-0024-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abbate A, Salloum F, Vecile E, Das A, Hoke N, Straino S, Biondi-Zoccai GGL, Houser J, Qureshi I, Ownby E, Gustini E, Biasucci L, Severino A, Capogrossi M, Vetrovec G, Crea F, Baldi A, Kukreja R, Dobrina A. Anakinra, a recombinant human interleukin-1 receptor antagonist, inhibits apoptosis in experimental acute myocardial infarction. Circulation. 2008;117:2670–2683. doi: 10.1161/CIRCULATIONAHA.107.740233. [DOI] [PubMed] [Google Scholar]
- 8.Bujak M, Dobaczewski M, Chatila K, Mendoza LH, Li N, Reddy A, Frangogiannis NG. Interleukin-1 receptor type I signaling critically regulates infarct healing and cardiac remodeling. Am J Pathol. 2008;173:57–67. doi: 10.2353/ajpath.2008.070974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saraste A, Nekolla S, Schwaiger M. Contrast-enhanced magnetic resonance imaging in the assessment of myocardial infarction and viability. J Nucl Cardiol. 2008;15:105–117. doi: 10.1007/BF02976902. [DOI] [PubMed] [Google Scholar]
- 10.Gardin J, Adams D, Douglas P, Feigenbaum H, Forst D, Fraser A, Grayburn P, Katz A, Keller A, Kerber R, Khandheria B, Klein A, Lang R, Pierard L, Quinones M, Schnittger I. Recommendations for a standardized report for adult transthoracic echocardiography: a report from the American Society of Echocardiography's Nomenclature and Standards Committee and Task Force for a Standardized Echocardiography Report. J Am Soc Echocardiogr. 2002;15:275–290. doi: 10.1067/mje.2002.121536. [DOI] [PubMed] [Google Scholar]
- 11.Braunwald E. Shattuck lecture—cardiovascular medicine at the turn of the millennium: triumphs, concerns, and opportunities. N Engl J Med. 1997;337:1360–1369. doi: 10.1056/NEJM199711063371906. [DOI] [PubMed] [Google Scholar]
- 12.Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lloyd-Jones D, McDermott M, Meigs J, Moy C, Nichol G, O'Donnell C, Roger V, Sorlie P, Steinberger J, Thom T, Wilson M, Hong Y. Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25–e146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 13.Marino P, Zanolla L, Zardini P. Effect of streptokinase on left ventricular modeling and function after myocardial infarction: the GISSI (Gruppo Italiano per lo Studio della Streptochinasi nell`Infarto Miocardico) trial. J Am Coll Cardiol. 1989;14:1149–1158. doi: 10.1016/0735-1097(89)90409-9. [DOI] [PubMed] [Google Scholar]
- 14.St John Sutton M, Pfeffer MA, Plappert T, Rouleau JL, Moyé LA, Dagenais GR, Lamas GE, Klein M, Sussex B, Goldman S, the SAVE investigators Quantitative two-dimensional echocardiographic measurements are major predictors of adverse cardiovascular events after acute myocardial infarction: the protective effects of captopril. Circulation. 1994;89:68–75. doi: 10.1161/01.cir.89.1.68. [DOI] [PubMed] [Google Scholar]
- 15.Doughty RN, Whalley GA, Walsh HA, Gamble GD, Lopez-Sendon J, Sharpe N, the CAPRICORN ECHO Substudy Investigators Effects of carvedilol on left ventricular remodeling after acute myocardial infarction. Circulation. 2004;109:201–206. doi: 10.1161/01.CIR.0000108928.25690.94. [DOI] [PubMed] [Google Scholar]
- 16.GISSI Group Long-term effects of intravenous thrombolysis in acute myocardial infarction: final report of the GISSI study. Gruppo Italiano per lo studio della Streptochinasi nell'Infarto Miocardico (GISSI). Lancet. 1987;2:871–874. [PubMed] [Google Scholar]
- 17.Pfeffer MA, Lamas GE, Vaughan DE, Parisi AF, Braunwald E. Effect of captopril on progressive ventricular dilatation after anterior myocardial infarction. N Engl J Med. 1988;319:80–86. doi: 10.1056/NEJM198807143190204. [DOI] [PubMed] [Google Scholar]
- 18.Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico (GISSI) Group GISSI 3: effects of lisinopril and transdermal glyceryl trinitrate singly and together on 6-week mortality and ventricular function after acute myocardial infarction. Lancet. 1994;343:1115–1122. [PubMed] [Google Scholar]
- 19.CAPRICORN Investigators Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet. 2001;357:1385–1390. doi: 10.1016/s0140-6736(00)04560-8. [DOI] [PubMed] [Google Scholar]
- 20.Kaplanski G, Porat R, Aiura K, Erban Jk, Gelfand JA, Dinarello CA. Activated platelets induce endothelial secretion of interleukin-8 in vitro via an interleukin-1-mediated event. Blood. 1993;81:2492–2495. [PubMed] [Google Scholar]
- 21.Suzuki k, Murtuza B, Smolenski RT, Sammut IA, Suzuki N, Kaneda Y, Yacoub MH. Overexpression of interleukin-1 receptor antagonist provides cardioprotection against ischemia-reperfusion injury associated with reduction of apoptosis. Circulation. 2001;104(Suppl I):I308–I313. doi: 10.1161/hc37t1.094871. [DOI] [PubMed] [Google Scholar]
- 22.Anand I, Florea V, Fisher L. Surrogate end points in heart failure. J Am Coll Cardiol. 2002;39:1414–1421. doi: 10.1016/s0735-1097(02)01773-4. [DOI] [PubMed] [Google Scholar]
- 23.White HD, Norris RM, Brown MA, Brandt PW, Whitlock RN, Wild CJ. Left ventricular end-systolic volume as the major determinant of survival after recovery from myocardial infarction. Circulation. 1987;76:44–51. doi: 10.1161/01.cir.76.1.44. [DOI] [PubMed] [Google Scholar]
- 24.Crossman D, Morton A, Gunn J, Greenwood J, Hall A, Fox K, Lucking A, Flather M, Lees B, Foley C. Investigation of the effect of interleukin-1 receptor antagonist (IL-1RA) on markers of inflammation in non-ST elevation acute coronary syndromes (the MRC-ILA-HEART Study). Trials. 2008;9:8–14. doi: 10.1186/1745-6215-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Furst D. Anakinra: review of recombinant human interleukin-I receptor antagonist in the treatment of rheumatoid arthritis. Clin Ther. 2004;26:1960–1975. doi: 10.1016/j.clinthera.2004.12.019. [DOI] [PubMed] [Google Scholar]
- 26.Ikonomidis I, Lekakis JP, Nikolau M, Paraskevaidis I, Andreaudou I, Kaplanoglou T, Katsimbri P, Skarantavous G, Soucacos PN, Kremastinos DT. Inhibition of interleukin-1 by anakinra improves vascular and left ventricular function in patients with rheumatoid arthritis. Circulation. 2008;117:2662–2669. doi: 10.1161/CIRCULATIONAHA.107.731877. [DOI] [PubMed] [Google Scholar]
- 27.Orn S, Manhenke C, Ueland T, Dams J, Mollnes T, Edvardsen T, Aukrust P, Dickstein K. C-reactive protein, infarct size, microvascular obstruction, and left-ventricular remodelling following acute myocardial infarction. Eur Heart J. 2009;30:1180–1186. doi: 10.1093/eurheartj/ehp070. [DOI] [PubMed] [Google Scholar]