Abstract
Background
This study examined stability of remission in patients who were abstainers and non-problem users at 1-year after entering private, outpatient alcohol and drug treatment. We examined: (a) How does risk of relapse change over time? (b) What was the risk of relapse for non-problem users versus abstainers? (c) What individual, treatment, and extra-treatment characteristics predicted time to relapse, and did these differ by non-problem use versus abstinence?
Methods
The sample consisted of 684 adults in remission (i.e., abstainers or non-problem users) 1 year following treatment intake. Participants were interviewed at intake, and 1, 5, 7, 9, and 11 years after intake. We used discrete-time survival analysis to examine when relapse is most likely to occur and predictors of relapse.
Results
Relapse was most likely at 5-year, and least likely at 11-year follow-up. Non-problem users had twice the odds of relapse compared to abstainers. Younger individuals and those with fewer 12-step meetings and shorter index treatment had higher odds of relapse than others. We found no significant interactions between non-problem use and the other covariates suggesting that significant predictors of outcome did not differ for non-problem users.
Conclusions
Non-problem use is not an optimal 1-year outcome for those in an abstinence-oriented, heterogeneous substance use treatment program. Future research should examine whether these results are found in harm reduction treatment and self-help models, or in those with less severe problems. Results suggest treatment retention and 12-step participation are prognostic markers of long-term positive outcomes for those achieving remission at 1 year.
Keywords: Remission, Abstinence, Longitudinal, Treatment
1. Introduction
In the U.S., abstinence has been the predominant goal of substance use (SU) treatment. At the same time, as with “improvement” outcomes for other health conditions (lowered blood pressure or cholesterol for cardiovascular outcomes) researchers have examined other more pragmatic outcomes, such as reduced use of substances and remission of dependence symptoms. A similar shift has occurred in treatment philosophy, stimulated by outcomes research and harm reduction approaches that consider other outcomes, such as fewer days of drinking or heavy drinking, or reduced drug use.
What is not known is whether long-term outcomes for individuals entering SU treatment are similar between those reducing use to light levels and having no alcohol or drug-related problems and those attaining abstinence after treatment. Studies on remission or decreased use have often examined general population samples and focused on alcohol only (Dawson et al., 2007; Ilgen et al., 2008; Moos and Moos, 2006; Rosenberg, 1993; Sobell and Sobell, 1995), or on durations of 3 years or less (Dawson et al., 2007). Further, most research has been substance-specific, not reflecting the heterogeneity of drug dependence found in today’s treatment programs. Because today’s public and private treatment populations most often use multiple substances (Institute of Medicine, 2006; Rounsaville et al., 2003; Stinson et al., 2005; Tsuang et al., 1994; Weisner et al., 2001a), examining stability and predictors of relapse versus sustained remission in a heterogeneous treatment sample can inform clinical interventions.
1.1. Stability of remission
Prior studies on stability and predictors of remission included general populations, individuals seeking help for alcohol problems, and those in alcohol treatment. Dawson and colleagues (Dawson et al., 2007) examined stability of drinking outcomes over 3 years among individuals remitted from alcohol use disorders in a national general population sample. Abstainers were more likely to maintain their status (77%) than asymptomatic risk drinkers or low risk drinkers (did not exceed NIAAA safe drinking amounts, and had no symptoms of alcohol use disorders). Yet, the large majority of low risk drinkers either maintained low risk drinking (48%) or moved to abstinence (18%) at 3 years. The odds of recurrence of alcohol use disorder symptoms did not differ between low-risk drinkers and abstainers for individuals younger than 35, and the odds of relapse to dependence was not higher for low-risk drinkers younger than 45 than for abstainers (though older non-abstaining individuals had higher odds of relapse than abstainers).
A study of help-seeking individuals (Ilgen et al., 2008) compared those at 1-year follow-up who were abstinent, drinking without problems, or drinking with at least one alcohol-related problem. Those abstinent had higher rates of stable remission at 8 and 16 years than those drinking without problems.
Using Project MATCH data from alcohol treatment outpatients, Maisto et al. (2007) compared 3-year outcomes of those abstinent at 1 year versus two drinking levels – “moderate drinking” (i.e., fewer than 6 heavy drinking days in past year) or “heavy drinking” (6 or more heavy drinking days – five or more drinks per day for men, four or more for women). Alcohol-related problems were not considered. One-year abstainers had the most abstinent days and the fewest average drinks per drinking day, followed by moderate drinkers.
No studies that we know of have examined moderate or controlled use in a sample of patients treated in a program for both alcohol and drug disorders.
1.2. Predictors of outcomes
The literature on predictors of better long-term outcomes in alcohol and drug treatment patients indicates that better substance use outcomes are predicted by individual characteristics, such as female gender, older age, dependence type, health problems, lower levels of alcohol and drug severity, lower levels of psychiatric problem severity, and abstinence goals (Charney et al., 2005; Klein et al., 2002; Mertens et al., 2008; Ray et al., 2005; Satre et al., 2007; Weisner et al., 2003); treatment characteristics, such as longer duration of treatment and readmission (Chi et al., 2006; Ghose, 2008; Gottheil et al., 1992; Green et al., 2004; Mertens et al., 2005; Weisner et al., 2003); and extra-treatment characteristics such as 12-step participation (Kaskutas et al., 2003-2004; Ray et al., 2005; Weisner et al., 2003; Zemore and Kaskutas, 2008).
More specifically, there is a literature examining predictors of remission among those with problems who reduced to moderate drinking, and related research on correlates of non-problem drinking in former problem drinkers. Rosenberg’s (Rosenberg, 1993) review found that a key characteristic related to a higher likelihood of relapsing among moderate or “controlled” drinkers included low severity of dependence (e.g., less baseline alcohol consumption, later onset of drinking and first intoxication, fewer dependence symptoms and fewer alcohol-related medical, social, and legal problems). These factors were related to becoming non-problem drinkers in former problem drinkers (Ilgen et al., 2008), as was having lower depression severity. In treatment samples, recent research has found that abstinence goals predicted better alcohol use outcomes (Adamson et al., 2010), with some support for better outcomes in those with lower psychiatric or depression severity and employment problem severity (Ilgen et al., 2008; Rosenberg, 1993).
Within this context, we studied remission in a diverse treatment population of a large private, not-for-profit integrated care health system. We examined remission over 10 years employing a conceptual model of individual (demographics, problem severity and dependence type, treatment goals and health status at baseline), treatment (length of stay), and extra-treatment (12-step meetings during treatment) factors as predictors of remission (Delucchi et al., 2004, 2008; Mertens et al., 2005; Weisner et al., 2003). Our main focus was to understand how non-problem use versus abstinence as an “end of treatment” (12-month) outcome was related to stability of remission over the following 10 years, and how factors measured at intake and during treatment (i.e., length of stay, 12-step meeting attendance) helped to predict relapse versus remission over this time span. We compared non-problem users to abstainers on odds of relapse over 10 years. Using repeated measures of outcome status, we addressed the following questions: (a) How did the risk of relapse change over time between 5 and 11 years post-treatment after achieving remission at 1 year? (b) What was the risk of relapse for non-problem users versus abstainers? (c) What individual (e.g., demographics, dependence type, years of regular use of alcohol and drugs, alcohol and drug problem severity, and severity in the related domains of employment, medical, legal, psychiatric and family/social, and treatment goals to abstain), treatment (e.g., duration of index episode, readmissions), and extra-treatment (e.g., 12-step attendance) characteristics predicted time to relapse over 11 years? We also examined whether predictors were moderated by abstinence status versus non-problem use status at 1 year following treatment entry. We hypothesized that non-problem users would have higher odds of relapse and different predictors than abstainers.
2. Methods
2.1. Setting, treatment programs, and procedures
The study was conducted in the Kaiser Permanente (KP) Sacramento Chemical Dependency Recovery Program. Northern California KP is a large (three million membership) integrated health care delivery system, which provides substance use services internally, rather than by referral to contracted programs.
The original study assigned research subjects to day hospital or a traditional outpatient program. The day hospital provided four times the intensity of the outpatient program during the first 3 weeks, but services and program length were the same: 3 weeks followed by 5 weeks of similar intensity treatment to constitute the 8-week rehabilitation program. Aftercare (one outpatient session weekly for 10 months) began the 9th week. Treatment philosophy was based on total abstinence (for more information on the study site, programs, and methods of the original study, see Weisner et al., 2000).
Research subjects for the original study were 1,204 men and women aged 18 and over admitted to treatment between April 1994 and April 1996. Patients were offered the choice of accepting random assignment to day treatment or to the less intensive outpatient program. Those not agreeing to be randomized (i.e., self-selected into either program) were also followed and included in the study. Participants were recruited at intake by licensed master’s level research associates from the Division of Research (DOR). Interviews at 6 months, 1, 5, 7, 9, and 11 years after treatment intake were administered by telephone from the DOR in Oakland, CA. Breath and urinalysis were used to validate self-report.
Participants for the current study were individuals who were either abstainers or non-problem users (defined below) in the past 30 days (N = 684) when interviewed at 1 year (response rate of 85%).
Institutional review board approval was obtained from the Kaiser Research Foundation Institute and the University of California, San Francisco. At the baseline recruitment we obtained written informed consent for 6- and 12-month interviews, and at 6 months we obtained permission to contact participants for future interviews. Specific verbal consent to conduct 5-year, 7-year, 9-year, and 11-year interviews was obtained from participants at the beginning of each interview (and permission to contact for future interviews was asked at the end of each interview). Response rates at 5, 7, 9, and 11 years for the surviving cohort were 80.2%, 75.1%, 73.7% and 72.2%, respectively.
2.2. Measures
Measures were drawn from intake and follow-up interviews and the Kaiser Permanente Northern California automated databases (Selby, 1997).
2.2.1. Individual characteristics
Demographic variables collected at intake included gender, age (50+, <50), marital status (married/living as married, other), education level (at least some college or more, no college), ethnicity (White, African American, Hispanic/Latino, other), annual income (<$40,000, at least $40,000) and employment status (employed, unemployed/suspended). Health status at baseline was recoded from a Likert scale to a dichotomous variable where 0 was good/very good/excellent health, 1 fair/poor health.
We assessed substance problem severity with three sets of variables from the baseline interview. First, type of substance dependence was based on questions from the Diagnostic Interview Schedule for Psychoactive Substance Dependence to provide a DSM-IV diagnosis for alcohol, marijuana, stimulant, painkiller, methadone, heroin, barbiturate, tranquilizer, inhalant, hallucinogen, and cocaine dependence and abuse (American Psychiatric Association, 2000). For each substance, we established presence or absence of three of seven dependence symptoms (or one of three abuse symptoms) during the previous 6 months (Mertens and Weisner, 2000; Weisner et al., 2000, 2001a), and then categorized respondents as having alcohol-only, drug-only, or alcohol and drug dependence, or abuse only (no dependence). Secondly, we measured severity of substance use and related problems at baseline with the alcohol, drug, medical, social, psychiatric, legal and employment composite scores of the Addiction Severity Index (ASI) instrument (McLellan et al., 1992). Composite scores ranged from zero (no problems in the relevant domain) to 1.0 (high severity). We included number of years of regular use based on self-report, recorded at baseline, for alcohol, pain killers, marijuana, stimulants and cocaine (the most prevalent substances of dependence in our sample). Regular use for alcohol was defined as five or more drinks 3 times a week per month or more; regular use for all other substances was defined as three times a week per month or more. We measured whether the patient identified abstinence as his/her goal of treatment at baseline (Mertens and Weisner, 2000; Weisner et al., 2001b).
2.2.2. Treatment characteristics
We included two variables from the initial treatment episode: (1) treatment type: day hospital versus traditional outpatient, and (2) the length of time in treatment without dropping out for 7 days during the 8-week rehabilitation phase, or dropping out for 30 days during the 10-month aftercare phase (Mertens and Weisner, 2000). We also measured treatment readmissions following the initial episode. We calculated length of time in treatment and readmissions from the health plan’s automated administrative data system. Readmission was defined as having at least three visits (and no more than 30 days between visits) to a chemical dependency program between 1 and 4 years after intake (Mertens et al., 2005). We do not equate readmissions with relapse; for example, readmissions can also measure visits of brief support to maintain abstinence.
2.2.3. Extra-treatment characteristic
The 12-month interview included a question on the number of 12-step meetings attended in the prior 6 months.
2.2.4. Abstinence and remission outcomes
Remitted individuals were those who either reported abstaining in the past year, or those who were non-problem users as follows: they (a) used alcohol, but had no days of drinking five or more drinks in a day, and drank only four times per month or less in the past year; or used marijuana, but not more than once per month in the past year; (b) had no other drug use in the past year; (c) had no problems with friends or family, violent behavior, or suicidal ideations in the month prior to interview; and (d) had not been arrested, in jail/prison, under electronic home surveillance, or been to a probation or parole officer in the year prior to interview. This definition is consistent with other “non-problem use” and “remission” definitions in the literature (Moos and Moos, 2003; Ouimette et al., 2000) and we have used it in our previous published work (Chi et al., 2011; Mertens et al., 2008; Parthasarathy et al., in press; Satre et al., 2012). At 1-year follow-up these definitions were the same except that we only measured past month substance use.
We define “stable remission” as having no relapses into problem use at any follow-up time point.
2.2.5. Outcome
Relapse into problem use was measured at each time point. Problem use was defined as being neither abstinent nor a non-problem user (defined above) in the past year at each follow-up.
2.3. Analysis
Standard summary statistics including percentages, means, and standard deviations, were used to describe the sample. Pearson chi-square analyses were used to compare the difference between relapsers and stably remitted individuals as well as status at 1 year (abstinent, non-problem user) for the categorical variables, and t-tests were used for continuous variables.
As our data has five predetermined follow-up times, we used discrete-time survival analysis to examine the odds of relapse at subsequent time points and to examine predictors of relapse. This method is well-suited to longitudinal data with repeated measures of a discrete time outcome and allows for censoring of missing data at follow-up points. The initial model in a set of nested models included only the time effect represented by four dummy variables (one each for years 5, 7, 9 and 11). The time-only model estimates the overall population profile of the risk across time and indicates when events are more likely to occur (Xie et al., 2003). Abstinence versus non-problem use at 1 year was our main variable of interest so it was added to the second model (which also included the time effect) to see whether the hazard functions differed between these two groups. In the third model we added demographic, treatment and extra treatment variables in that order, to determine a final model with a best fit in predicting relapse. After finding our best fit model, we ran additional models with interactions between status at 1 year and the other covariates to test for moderation by non-problem use. Effects of the initial treatment (day hospital versus outpatient) and randomization (randomized versus not) were also tested in each model. These two variables did not significantly (p < .05) predict relapse and their inclusion did not change the pattern of results, so they were not included in the final models.
We also used the discrete-time survival analysis method to estimate the survival function for remission and hazard function for relapse into problem use. The survival probability was based on the model including only the time indicators and illustrates the cumulative probability of remitting over time. Hazard function graphs were created for the full sample over time by remission status at 1 year, using the model with time indictors and remission status at 1 year (abstinent, non-problem user). This graph describes the probability of relapsing back into problem use over time.
3. Results
The sample (N = 684) was 36% female and 50% married/partnered, with a mean age of 38 years (SD = 10.7) (not shown). Ethnic composition was 76% white, 11% black, 9% Hispanic, and 5% other. A total of 43% were alcohol-only dependent, 27% were drug-only dependent, 16% were alcohol and drug dependent, and 4% had abuse diagnoses only.
A total of 103 (15%) of the remitted individuals were non-problem users at 1 year (not shown) (see Table 1). The highest percentage of participants for both abstainers and non-problem users had alcohol only or drug only dependence at baseline. More abstainers reported abstinence goals at intake (81%) compared to non-problem users (63%) (p < .0001). Fifty percent of abstainers and 33% of non-problem users were assigned to the day hospital treatment arm (p = .0011). Abstainers had longer stays in index treatment (mean = 88.8 days, SD = 121.1) than non-problem users (mean = 22.7 days, SD = 42.4) (p < .0001); they also had more 12-step meetings (mean = 38.2, SD = 50.1) than non-problem users (mean = 6.4, SD = 17.9; p < .0001). Income, education, ethnicity, employment status, health status, baseline measures of ASI severity in all seven domains, number of years of regular use of alcohol or other drugs, and number of readmissions did not differ significantly between abstainers and non-problem users by status at 1 year.
Table 1.
Individual, treatment and extra-treatment characteristics by remission status at year 1.
| Non-problem users (N = 103) | Abstainers (N = 581) | p | |
|---|---|---|---|
| Individual characteristics | |||
| Women | 32% | 37% | ns |
| Age group (51+) | 7% | 14% | <.05 |
| Married | 42% | 51% | ns |
| Education (at least some college) | 28% | 28% | ns |
| Ethnicity | |||
| White | 72% | 76% | |
| African-American | 16% | 10% | |
| Hispanic/Latino | 6% | 9% | |
| Other | 7% | 4% | ns |
| Annual income ($40,000+) | 50% | 49% | ns |
| Employed | 58% | 58% | ns |
| Self-reported health status (baseline) | |||
| Excellent/very good/good | 59% | 56% | ns |
| Dependence type | |||
| Abuse only (no dependence) | 14% | 15% | |
| Alcohol only | 31% | 45% | |
| Drugs only | 35% | 25% | |
| Alcohol and drugs | 19% | 15% | <.05 |
| Goal to stop using substance | 63% | 81% | <.001 |
| Day hospital treatment | 33% | 50% | <.001 |
| ASI alcohol problem severity (baseline), mean (SD) | 0.39 (0.30) | 0.45 (0.32) | ns |
| ASI drug problem severity (baseline), mean (SD) | 0.13 (0.10) | 0.11 (0.10) | ns |
| ASI family/social problem severity (baseline), mean (SD) | 0.41 (0.30) | 0.40 (0.30) | ns |
| ASI psychiatric problem severity (baseline), mean (SD) | 0.41 (0.27) | 0.40 (0.26) | ns |
| ASI legal problem severity (baseline), mean (SD) | 0.09 (0.19) | 0.10 (0.20) | ns |
| ASI employment problem severity (baseline), mean (SD) | 0.37 (0.25) | 0.37 (0.26) | ns |
| ASI medical problem severity (baseline), mean (SD) | 0.35 (0.37) | 0.39 (0.41) | ns |
| Number of years of regular use – alcohol, mean (SD) | 8.53 (9.63) | 10.33 (9.53) | ns |
| Number of years of regular use – painkiller, mean (SD) | 0.99 (1.17) | 1.17 (3.43) | ns |
| Number of years of regular use – marijuana, mean (SD) | 6.41 (8.01) | 6.47 (7.60) | ns |
| Number of years of regular use – stimulant, mean (SD) | 4.90 (6.85) | 3.96 (5.51) | ns |
| Number of years of regular use – cocaine, mean (SD) | 2.24 (4.48) | 2.55 (4.32) | ns |
| Treatment characteristics | |||
| Length of stay (days), mean (SD) | 22.7 (42.4) | 88.8 (121.1) | <.001 |
| Readmissions (from year 1 to year 4), mean (SD) | 0.13 (0.36) | 0.20 (0.57) | ns |
| Extra-treatment characteristics | |||
| Number of 12-step visits attended (year 1), mean (SD) | 6.4 (17.9) | 38.2 (50.1) | <.001 |
Note: Sample included only those abstinent or non-problem users at the year 1 follow up (N = 684).
ns: Not statistically significant p < .05.
A total of 330 participants were stably remitted from year 1 through year 11; 354 relapsed into problem use. Those stably remitted were less likely to be non-problem users at 1 year (8%) than were those who relapsed (22%, p < .0001; see Table 2). Fewer of the stably remitted were employed at baseline (53%; 63% of relapsed, p = .0098), however more were over 50 years old (19% stably remitted, 7% of relapsed; p < .0001. Eighty-four percent of stably remitted reported abstinence goals compared to 73% of relapsed (p = .0003). Stably remitted individuals had lower average ASI drug problem severity scores (mean = 0.11, SD = 0.1; relapsed: mean = 0.12, SD = 0.1; p = .0330) and a higher average years of regular use of alcohol (mean = 11.2, SD = 9.8; relapsers: mean = 9.0, SD = 9.2; p = .0045). Those stably remitted had longer stays in index treatment (mean = 97.6 days, SD = 126.9) than those who relapsed (mean = 61.5 days, SD = 100.3) (p < .0001); they also had more 12-step meetings (40.6 and 26.7, respectively; p = .0002).
Table 2.
Individual, treatment and extra-treatment characteristics by stable remission status through 11 years.
| Stably remitted (N = 330) | Relapsers (N = 354) | p-Value | |
|---|---|---|---|
| Individual characteristics | |||
| Women | 38% | 34% | ns |
| Age group (51+) | 19% | 7% | <.0001 |
| Married | 53% | 47% | ns |
| Education (at least some college) | 31% | 25% | ns |
| Ethnicity | |||
| White | 75% | 76% | ns |
| African-American | 11% | 11% | |
| Hispanic/Latino | 10% | 8% | |
| Other | 4% | 5% | |
| Annual income ($40,000+) | 50% | 50% | ns |
| Employed | 53% | 63% | .0098 |
| Self-reported health status (baseline) | |||
| Excellent/very good/good | 22% | 28% | ns |
| Status at year 1 | |||
| Abstinent | 92% | 78% | <.0001 |
| Non-problem use | 8% | 22% | |
| Dependence type | |||
| Abuse only (no dependence) | 16% | 12% | ns |
| Alcohol only | 45% | 41% | |
| Drugs only | 23% | 30% | |
| Alcohol and drugs | 15% | 16% | |
| Goal to stop using substance | 84% | 73% | .0003 |
| Day hospital treatment | 49% | 46% | ns |
| ASI Alcohol problem severity (baseline), mean (SD) | 0.46 (0.33) | 0.43 (0.30) | ns |
| ASI drug problem severity (baseline), mean (SD) | 0.10 (0.11) | 0.12 (0.11) | .0330 |
| ASI family/social problem severity (baseline), mean (SD) | 0.41 (0.29) | 0.39 (0.30) | ns |
| ASI psychiatric problem severity (baseline), mean (SD) | 0.40 (0.26) | 0.43 (0.27) | ns |
| ASI legal problem severity (baseline), mean (SD) | 0.10 (0.20) | 0.11 (0.20) | ns |
| ASI employment problem severity (baseline), mean (SD) | 0.39 (0.26) | 0.36 (0.25) | ns |
| ASI medical problem severity (baseline), mean (SD) | 0.39 (0.42) | 0.38 (0.39) | ns |
| Number of years of regular use – alcohol, mean (SD) | 11.18 (9.82) | 9.02 (9.21) | .0045 |
| Number of years of regular use – painkiller, mean (SD) | 1.19 (3.76) | 1.10 (3.07) | ns |
| Number of years of regular use – marijuana, mean (SD) | 6.38 (7.83) | 6.52 (7.55) | ns |
| Number of years of regular use – stimulant, mean (SD) | 4.44 (6.11) | 3.86 (5.45) | ns |
| Number of years of regular use – cocaine, mean (SD) | 2.75 (4.49) | 2.30 (4.23) | ns |
| Treatment characteristics | |||
| Length of stay (days), mean (SD) | 97.57 (126.94) | 61.48 (100.29) | <.0001 |
| Readmissions (from year 1 to year 4), mean (SD) | 0.22 (0.62) | 0.17 (0.46) | ns |
| extra-treatment characteristics | |||
| Number of 12-step visits attended (1 year), mean (SD) | 40.63 (50.36) | 26.69 (44.77) | .0002 |
Note: Sample included only those abstinent or non-problem users at the year 1 follow-up (N = 684).
ns: Not statistically significant p < .05.
Fig. 1 illustrates the probability of relapse for non-problem users versus abstainers. Non-problem users began with a higher probability of relapse at 5 years compared to abstainers and continued that trend over time. A time-only model was estimated to examine the probability of relapse at each follow-up. The probability of relapse was highest at 5 years and lowest at 11 years (Table 2). A second model was run adding only the abstinence versus non-problem status at 1 year variable to compare the probability of relapse between the two groups. Individuals who were non-problem users at 1 year had 2.93 times the odds of relapsing over time as those who were abstinent (Table 3).
Fig. 1.
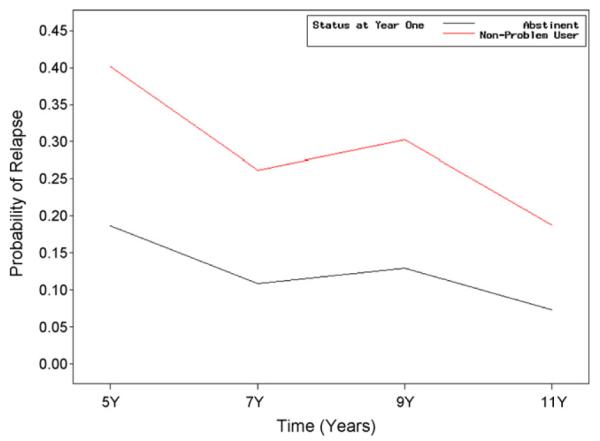
Hazard function for relapse into problem use for non-problem users at year 1 versus abstainers at year 1.
Table 3.
Hazard models presenting probability of relapse by time point, non-problem use status and other factors (N = 684).
| Model 1 |
Model 2 |
Model 3 |
||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CIs | Odds ratio | 95% CIs | Odds ratio | 95% CIs | |
| Time 1 (5 year) | 0.28*** | [0.23, 0.34] | 0.23*** | [0.19, 0.28] | 0.46*** | [0.29, 0.73] |
| Time 2 (7 year) | 0.14*** | [0.10, 0.19] | 0.12*** | [0.09, 0.17] | 0.24*** | [0.14, 0.42] |
| Time 3 (9 year) | 0.17*** | [0.12, 0.24] | 0.15*** | [0.10, 0.21] | 0.33*** | [0.19, 0.58] |
| Time 4 (11 year) | 0.09*** | [0.05, 0.14] | 0.08*** | [0.05, 0.13] | 0.17*** | [0.08, 0.33] |
| Non-problem use (vs. abstinence)a | 2.93*** | [2.04, 4.20] | 2.07*** | [1.40, 3.07] | ||
| Length of stay (in days) | 0.99* | [0.99, 1.00] | ||||
| # 12-Step meetings attended (past mo.)a | 0.99*** | [0.99, 1.00] | ||||
| Baseline variables | ||||||
| Age 50+ (vs. younger) | 0.63* | [0.37, 1.08] | ||||
| Gender | 0.88 | [0.65, 1.18] | ||||
| Dependence type | ||||||
| Alcohol-only (Ref.) | 1.00 | – | ||||
| Drug-only | 1.08 | [0.75, 1.56] | ||||
| Alcohol and drug | 1.02 | [0.67, 1.56] | ||||
| Abuse | 0.79 | [0.49, 1.27] | ||||
| Poor or fair health status | 0.86 | [0.64, 1.15] | ||||
| Goal to abstain | 0.78 | [0.55, 1.11] | ||||
| −2 Log L | 1305.15 | 1273.73 | 1207.44 | |||
Measured at 1-year follow-up.
p < .10.
p < .01.
The full model builds upon the previous two models adding individual, treatment, and extra-treatment covariates. Controlling for these potentially important predictors, non-problem users had twice the odds of relapse compared to abstainers (OR = 2.07, CI = (1.40, 3.07), p < .01). Attending more 12-step meetings in the past 30 days at 1 year decreased the odds of relapse (OR = 0.99, CI = (0.99, 1.00), p < .01). Longer stays in index treatment also decreased relapse odds (OR = 0.99 CI = (0.99,1.00), p < .01), but no other variables were related.
To examine whether non-problem users had different predictors of relapse than abstainers, we examined interactions between status at 1 year and each of the other covariates in separate models. None of the interactions were significant.
4. Discussion
4.1. Relapse risk for non-problem users versus abstainers by follow-up time point
In this private treatment sample of patients with substance use disorders, only 15% of patients in remission at 1 year after treatment intake were non-problem users rather than abstinent. Compared to those abstinent at 1 year, non-problem users were more likely alcohol than drug dependent. They also attended fewer 12-step meetings, which is consistent with the practice of 12-step members being told that membership requires a “sincere desire to stop” substance use. Consistent with prior research (Adamson et al., 2010), non-problem users were less likely to have goals to abstain at treatment entry. About 40% of non-problem users reported at intake that they had no plans for abstinence. Yet 60% did plan for abstinence and still used substances at 12 months, even if non-problematically.
Among individuals remitted at 1 year after outpatient treatment, 75% of non-problem users relapsed at some point over the 10 subsequent years versus 48% of abstainers. Even when controlling for age, gender, dependence type, health status, abstinence goals at intake, length of index treatment, and 12-step involvement, non-problem users had twice the odds of relapse over the 10 subsequent years than abstainers. This is consistent with prior alcohol research which found better outcomes for abstainers than low-risk or moderate drinkers (Dawson et al., 2007; Ilgen et al., 2008; Maisto et al., 2007). However, the current findings must be understood in the context of the treatment setting – 1 year after intake to an abstinence-oriented treatment program. These results may not generalize to a harm reduction model of treatment or among less severe, untreated individuals. There is evidence that some non-abstinence-oriented alcohol treatment approaches can be effective, particularly Behavioral Self-Control Training (Saladin and Santa Ana, 2004). Moreover, it may be that those able to maintain abstinent recovery for some significant period of time (e.g., 5 years or more) may successfully “step-down” to controlled or moderate, non-problematic use (Dennis et al., 2003).
Of note, risk of relapse was highest in the earliest follow-up period and least at 11 years, and this was particularly true for non-problem users, given their more dramatic decrease in hazard for relapse. Future longitudinal research should examine the ideal length of time for which individuals in abstinence treatment need to remain abstinent before successfully moving to long-term non-problem use, and how this differs by patient, treatment, and extra-treatment characteristics.
4.2. Individual, treatment, and extra-treatment predictors of time to relapse
Of the individual, treatment, and extra-treatment characteristics examined, only shorter lengths of stay, and less 12-step involvement predicted subsequent relapse. Research is needed on how time-varying versions of these factors (e.g., goals to abstain or reduce use) are related to longitudinal outcomes. It may be that early involvement in 12-step (at 1 year) and length of stay also reinforce the value of 12-step facilitation, and that treatment retention may have effects on long-term outcomes. On the other hand, these findings could also suggest that an unmeasured factor, such as a strong goal-orientation, is related to use of treatment and 12-step and better outcomes, despite efforts to control for confounders. In either case, the results suggest that longer stays in treatment and 12-step attendance are prognostic markers for better outcomes in those who remit at 1-year.
In contrast with some prior research in alcohol samples which found that abstinence goals predicted better 12-month outcomes (Adamson et al., 2010), we did not find that baseline abstinence goals were independently predictive of the probability of relapse through 9 years. That our findings differed is likely due to the longer time frame studied here. Intentions to abstain on treatment entry may fade over time, particularly when not reinforced by support such as longer treatment stays and 12-step participation, both of which predicted better outcomes here.
This study of initially remitted patients (at 1 year after index treatment entry) found that predictors of relapse were not moderated by non-problem versus abstinence at 1 year after intake. Thus in this treatment sample we did not find evidence that predictors of relapse were unique for non-problem users versus abstainers.
4.3. Non-problem users: relapse versus remission
Like previous studies, a small number of individuals with non-problem use in this study (N = 26) were able to successfully sustain remission. As discussed above, we did not find any unique predictors of outcome for non-problem users. We found no significant differences by dependence type (i.e., alcohol-only versus drug-only versus drug and alcohol dependence) in this sample of heterogeneous substance dependence. It appears that no factors in this sample of non-problem users were uniquely associated with outcomes. It is particularly of note that there was no interaction between non-problem use at year 1 and 12-step attendance, an abstinence-oriented program. Thus, 12-step was not differentially useful for those who had abstained at year 1. It may be that 12-step attendance, and more broadly, abstinence oriented philosophies, are useful for preventing relapse into problematic use because they do reinforce the danger of complete relapse. Qualitative work and studies with larger numbers of such individuals are needed to understand how they differ from non-problem users who relapse.
The current study had several limitations. One is the relatively small group of non-problem users (N = 103). However, this is the first study that we know of that has examined relapse by non-problem use versus abstinence status in treatment clients which includes drugs other than alcohol. Another limitation is that this study uses observational data so we are unable to attribute causality to the significant covariates. We note that the relationship of longer treatment stays and 12-step participation may be partially due to higher levels of an unmeasured factor such as motivation, despite attempts to control for potential confounders including measures of motivation (i.e., abstinence goals) and alcohol and drug severity. We were also limited by our available data for our measure of remission which incorporates measurement of substance-related problems including problems with friends or family, violent behavior, or suicidal ideations; we had only a past-month measurement for these aspects of remission. Moreover, our measurement of non-problem use versus abstinence at 1-year post-treatment was limited to past month alcohol and drug use. Yet, we did examine agreement between the past-month and past-year measures of remitted versus problem use at the 5 through 11-year follow-ups and found agreement between the two measures of 85% and above for each of the follow-ups.
5. Conclusions
In this treatment sample, using data from 11 years after treatment entry we found that non-problem use is not an optimal 1 year outcome for those in abstinence-oriented treatment. Future research should examine whether these results are found in harm reduction treatment and self-help models, or in those with less severe problems. Longitudinal research examining new theories for how some non-problem drinkers maintain remission is also needed. Possible explanations to explore may address how these individuals cope with life events that others have more difficulty negotiating, or how motivation is maintained over time.
Our findings on predictors of relapse suggest that risk for relapse in remitted individuals becomes lower over time. Of note, we did not find that predictors of relapse differed for the non-problem users (versus abstainers). Overall, the lack of unique predictors for non-problem users suggests that among those treated in abstinence-oriented treatment, there may be no need to develop different treatment approaches for such individuals’ long term care, and that 12-step and longer initial treatments could be beneficial for them as well. Moreover, even if a subgroup of patients can resume non-problematic use, clinicians are not able to easily identify them in advance. Abstinence as a goal at the very least allows patients to choose something that may be unattainable over the longer term but encourages efforts that would not otherwise be present. Thus, the number of relapsers may have been even higher if abstinence was minimized as a desirable endpoint. The results also suggest that treatment retention and 12-step participation are prognostic markers of long-term positive outcomes for those who achieve remission at 1 year.
Acknowledgements
The Drug and Alcohol Research Team at the Kaiser Permanente Division of Research provided valuable assistance in the development of this study. We thank Barbara Pichotto, Cynthia Perry-Baker, Diane Lott Garcia, Gina Smith-Anderson, Lynda Tish, Melanie Jackson, and Virginia Browning for interviewing and participant tracking, Stacy Sterling for project management, and Agatha Hinman for editorial assistance. We also thank the study participants and the clinicians of the Kaiser Permanente Sacramento Chemical Dependency Recovery Program.
Role of funding source This study was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (R01 AA010359). The contents of this paper are solely the responsibility of the authors and do not necessarily represent the views of any of the funding agencies. Funding sources had no further role in study design, in the collection, analysis and interpretation of data, in the writing of the report, or in the decision to submit the paper for publication.
Footnotes
Contributors Dr. Mertens conceived the current study questions, conducted the literature review, and drafted the introduction and discussion sections of the manuscript. She is the Principal Investigator of the study providing the data. Dr. Delucchi and Ms. Kline-Simon directed the choice of analytic techniques, and they and Drs. Mertens and Weisner conceived the study design. Ms. Kline-Simon conducted the analyses and drafted the methodology and results sections. In addition, Ms. Andrea H. Kline-Simon and Drs. Delucchi, Moore, and Weisner contributed to data interpretation, provided critical revisions, and gave final approval of the manuscript.
Conflict of interest All other authors declare that they have no conflicts of interest.
References
- Adamson SJ, Heather N, Morton V, Raistrick D. Initial preference for drinking goal in the treatment of alcohol problems. II. Treatment outcomes. Alcohol Alcohol. 2010;45:136–142. doi: 10.1093/alcalc/agq005. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Text Revision. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Charney DA, Palacios-Boix J, Negrete JC, Dobkin PL, Gill KJ. Association between concurrent depression and anxiety and six-month outcome of addiction treatment. Psychiatr. Serv. 2005;56:927–933. doi: 10.1176/appi.ps.56.8.927. [DOI] [PubMed] [Google Scholar]
- Chi FW, Parthasarathy S, Mertens JR, Weisner CM. Continuing care and long-term substance use outcomes in managed care: initial evidence for a primary care based model. Psychiatr. Serv. 2011;62:1194–2000. doi: 10.1176/appi.ps.62.10.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi FW, Satre DD, Weisner C. Chemical dependency patients with cooccurring psychiatric diagnoses: service patterns and 1-year outcomes. Alcohol. Clin. Exp. Res. 2006;30:851–859. doi: 10.1111/j.1530-0277.2006.00100.x. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Grant BF. Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: a 3-year follow-up. Alcohol. Clin. Exp. Res. 2007;31:2036–2045. doi: 10.1111/j.1530-0277.2007.00536.x. [DOI] [PubMed] [Google Scholar]
- Delucchi KL, Matzger H, Weisner C. Dependent and problem drinking over 5 years: a latent class growth analysis. Drug Alcohol Depend. 2004;74:235–244. doi: 10.1016/j.drugalcdep.2003.12.014. [DOI] [PubMed] [Google Scholar]
- Delucchi KL, Matzger H, Weisner C. Alcohol in emerging adulthood: 7-year study of problem and dependent drinkers. Addict. Behav. 2008;33:134–142. doi: 10.1016/j.addbeh.2007.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Scott CK, Funk R. An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Eval. Program. Plann. 2003;26:339–352. doi: 10.1016/S0149-7189(03)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghose T. Organizational- and individual-level correlates of posttreatment substance use: a multilevel analysis. J. Subst. Abuse Treat. 2008;34:249–262. doi: 10.1016/j.jsat.2007.04.007. [DOI] [PubMed] [Google Scholar]
- Gottheil E, McLellan AT, Druley KA. Length of stay, patient severity and treatment outcome: sample data from the field of alcoholism. J. Stud. Alcohol. 1992;53:69–75. doi: 10.15288/jsa.1992.53.69. [DOI] [PubMed] [Google Scholar]
- Green CA, Perrin NA, Polen MR. Gender differences in the relationships between multiple measures of alcohol consumption and physical and mental health. Alcohol. Clin. Exp. Res. 2004;28:754–764. doi: 10.1097/01.alc.0000125342.28367.a1. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Wilbourne PL, Moos BS, Moos RH. Problem-free drinking over 16 years among individuals with alcohol use disorders. Drug Alcohol Depend. 2008;92:116–122. doi: 10.1016/j.drugalcdep.2007.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine . Improving the Quality of Health Care for Mental and Substance-Use Conditions: Quality Chasm Series. National Academies Press; Washington, DC: 2006. [PubMed] [Google Scholar]
- Kaskutas LA, Ammon L, Weisner C. A naturalistic comparison of out-comes at social and clinical model substance abuse treatment programs. Int. J. Self-Help Self-Care. 2003-2004;2:111–133. [Google Scholar]
- Klein C, di Menza S, Arfken C, Schuster CR. Interaction effects of treatment setting and client characteristics on retention and completion. J. Psychoactive Drugs. 2002;34:39–50. doi: 10.1080/02791072.2002.10399935. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Clifford PR, Stout RL, Davis CM. Moderate drinking in the first year after treatment as a predictor of three-year outcomes. J. Stud. Alcohol Drugs. 2007;68:419–427. doi: 10.15288/jsad.2007.68.419. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The Fifth Edition of the Addiction Severity Index. J. Subst. Abuse Treat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Mertens JR, Flisher AJ, Satre DD, Weisner CM. The role of medical conditions and primary care services in 5-year substance use outcomes among chemical dependency treatment patients. Drug Alcohol Depend. 2008;98:45–53. doi: 10.1016/j.drugalcdep.2008.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens JR, Weisner C, Ray GT. Readmission among chemical dependency patients in private, outpatient treatment: patterns, correlates and role in long-term outcome. J. Stud. Alcohol. 2005;66:842–847. doi: 10.15288/jsa.2005.66.842. [DOI] [PubMed] [Google Scholar]
- Mertens JR, Weisner CM. Predictors of substance abuse treatment retention among women and men in an HMO. Alcohol. Clin. Exp. Res. 2000;24:1525–1533. [PubMed] [Google Scholar]
- Moos RH, Moos BS. Risk factors for nonremission among initially untreated individuals with alcohol use disorders. J. Stud. Alcohol. 2003;64:555–563. doi: 10.15288/jsa.2003.64.555. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction. 2006;101:212–222. doi: 10.1111/j.1360-0443.2006.01310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouimette PC, Moos RH, Finney JW. Two-year mental health service use and course of remission in patients with substance use and posttraumatic stress disorders. J. Stud. Alcohol. 2000;61:247–253. doi: 10.15288/jsa.2000.61.247. [DOI] [PubMed] [Google Scholar]
- Parthasarathy S, Chi FW, Mertens JR, Weisner C. The role of continuing care on 9-year cost trajectories of patients with intakes into an outpatient alcohol and drug treatment program. Med. Care. doi: 10.1097/MLR.0b013e318245a66b. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray GT, Weisner CM, Mertens JR. Relationship between use of psychiatric services and five-year alcohol and drug treatment outcomes. Psychiatr. Serv. 2005;56:164–171. doi: 10.1176/appi.ps.56.2.164. [DOI] [PubMed] [Google Scholar]
- Rosenberg H. Prediction of controlled drinking by alcoholics and problem drinkers. Psychol. Bull. 1993;113:129–139. doi: 10.1037/0033-2909.113.1.129. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Petry NM, Carroll KM. Single versus multiple drug focus in substance abuse clinical trials research. Drug Alcohol Depend. 2003;70:117–125. doi: 10.1016/s0376-8716(03)00033-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saladin ME, Santa Ana EJ. Controlled drinking: more than just a controversy. Curr. Opin. Psychiatry. 2004;17:175–187. [Google Scholar]
- Satre DD, Blow FC, Chi FW, Weisner C. Gender differences in seven-year alcohol and drug treatment outcomes among older adults. Am. J. Addict. 2007;16:216–221. doi: 10.1080/10550490701375673. [DOI] [PubMed] [Google Scholar]
- Satre DD, Chi FW, Mertens JR, Weisner C. Effects of age and life transitions on alcohol and drug treatment outcome over nine years. J. Stud. Alcohol Drugs. 2012;73(3):459–468. doi: 10.15288/jsad.2012.73.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby JV. Linking automated databases for research in managed care settings. Ann. Intern. Med. 1997;127:719–724. doi: 10.7326/0003-4819-127-8_part_2-199710151-00056. [DOI] [PubMed] [Google Scholar]
- Sobell MB, Sobell LC. Controlled drinking after 25 years: how important was the great debate? Addiction. 1995;90:1149–1154. [PubMed] [Google Scholar]
- Stinson FS, Grant BF, Dawson DA, Ruan WJ, Huang B, Saha T. Comorbidity between DSM-IV alcohol and specific drug use disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2005;80:105–116. doi: 10.1016/j.drugalcdep.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Tsuang JW, Shapiro E, Smith TL, Schuckit MA. Drug use among primary alcoholic veterans. Am. J. Drug Alcohol Abuse. 1994;20:483–493. doi: 10.3109/00952999409109185. [DOI] [PubMed] [Google Scholar]
- Weisner C, Mertens J, Parthasarathy S, Moore C, Hunkeler EM, Hu T, Selby JV. The outcome and cost of alcohol and drug treatment in an HMO: day hospital versus traditional outpatient regimens. Health Serv. Res. 2000;35:791–812. [PMC free article] [PubMed] [Google Scholar]
- Weisner C, Mertens J, Parthasarathy S, Moore C, Lu Y. Integrating primary medical care with addiction treatment: a randomized controlled trial. J. Am. Med. Assoc. 2001a;286:1715–1723. doi: 10.1001/jama.286.14.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisner C, Mertens J, Tam T, Moore C. Factors affecting the initiation of substance abuse treatment in managed care. Addiction. 2001b;96:705–716. doi: 10.1046/j.1360-0443.2001.9657056.x. [DOI] [PubMed] [Google Scholar]
- Weisner C, Ray GT, Mertens J, Satre DD, Moore C. Short-term alcohol and drug treatment outcomes predict long-term outcome. Drug Alcohol Depend. 2003;71:281–294. doi: 10.1016/s0376-8716(03)00167-4. [DOI] [PubMed] [Google Scholar]
- Xie H, McHugo G, Drake R, Sengupta A. Using discrete-time survival analysis to examine patterns of remission from substance use disorder among persons with severe mental illness. Ment. Health Serv. Res. 2003;5:55–64. doi: 10.1023/a:1021759509176. [DOI] [PubMed] [Google Scholar]
- Zemore SE, Kaskutas LA. Services received and treatment outcomes in day-hospital and residential programs. J. Subst. Abuse Treat. 2008;35:232–244. doi: 10.1016/j.jsat.2007.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]


