Abstract
Background:
On the basis of clinical experience, it seems that sleep disturbances are common in children with cerebral palsy (CP); however, there is a lack of research and objective data to support this observation.
Aim of Work:
Our aim was to assess sleep of children with cerebral palsy, using validated sleep questionnaire.
Subjects and Methods:
one hundred children with diagnosis of CP were investigated via sleep questionnaires, with their ages from 2-12 years. The 100 children with CP were divided into two groups, pre-school group (52 children had a mean age 2.35 ± 1.04 years) and school ages group (48 children had a mean age 10.21 ± 3.75 years).
Results:
We found high incidence of sleep problem in both pre-school and school age groups. We found that pre-school children have more prevalence of early insomnia (46.2%, P value 0.028) and sleep bruxism (50%, P value 0.000), while school group suffer more sleep disordered breathing (SDB) (50%, P value 0.001), more nightmares (50%, P value 0.001), more sleep talking (12.5% P value 0.049), and more excessive daytime sleepiness (EDS) (62.5%, P value 0.001).
Conclusion:
Results of our study indicate that CP children have high incidence of sleep problem in both pre-school and school age groups.
Keywords: Cerebral palsy, children, sleep disorders, sleep questionnaire
Background
The prevalence of sleep disorders in school age children from general population varies in different studies from 10 to 40%.[1–3] Children with cerebral palsy (CP) are prone to sleep problems when compared to children without co-morbid chronic health problem.[4] Children with CP have a higher prevalence of sleep breathing problems than otherwise healthy children reported in community-based surveys.[5] The disruption of normal sleep patterns may have an enormous impact upon the interactive and cognitive skills of the child with CP. It adversely affects their quality of life and interferes with the normal sleeping patterns of siblings and parents. Indeed, sleep problems in children with CP are under-reported, under recognized, and under-treated.[6]
Aim of Work
Our aim was to assess sleep of children with cerebral palsy, using validated sleep questionnaire.
Subjects and Methods
Subjects
This was a cross-sectional study at pediatric neurology unit of Mansoura University Children`s Hospital (MUCH), where 100 children with diagnosis of CP were investigated via sleep questionnaires. Patients were recruited from our pediatric neurology outpatient clinic, at the period from June 2011 to January 2012. Our patients were cases with established diagnosis of cerebral palsy, with their ages from 2-12 years. The 100 children with CP were divided into two groups, pre-school group (52 children had a mean age 2.35 ± 1.04 years) and school ages group (48 children had a mean age 10.21 ± 3.75 years). Excluded from this study were children with co-morbid severe chronic health problems (renal, hepatic, and cardiac impairment), cases of specific genetic syndromes, and cases with hypognathia or any cephalometric craniofacial abnormality.
An informed consent was signed by all parents of children enrolled in this study, and the study design was approved by ethical committee of Mansoura University.
Methods
Sleep questionnaire
Our sleep questionnaire has been compiled from multiple sources[7–9] in orders to be applicable for assessment of pediatric patients sleep. It includes: 1. Demographic information like name, age, gender, school grade, residence, and contact information, 2. Current sleep problems, which consists of 19 questions and their answers giving information about night-time sleep disorders (like sleep disordered breathing, insomnia, parasomnias, and movement disorders), 3. Current daytime symptoms, which consist of 7 questions (their answers giving information about daytime sleep disorders like; difficult morning arousal, excessive daytime sleepiness, narcolepsy, and cataplexy), 4. General sleep information provides data about bed sharing, timing, and nap schedule, 5. There were also items about family history, associated medical or psychiatric problems, history of epilepsy, and drugs used for sleep or drug affecting sleep like anti-epileptic drugs.
Clinical examination
Full neurological assessment was done to determine the clinical subtype of CP (spastic diplegia, congenital hemiplegia, spastic quadriplegia, dystonic/dyskinesia, hypotonic and mixed CP).[10] Gross Motor Functional Classification System (GMFCS) level[11] were used for clinical classification of CP patients (I-ambulatory in all settings, II-walks without aids, but has limitations in community settings, III-walks with aids, IV-mobility requires wheelchair or adult assist, V-dependent for mobility). All neurological and functional assessments were performed by a single pediatric neurologist. All of our patients underwent full psychiatric evaluation by psychiatrist. Also, examination for associated visual or hearing impairment was done.
Statistical methods
IBM SPSS statistics (V. 19.0, IBM Corp., USA, 2010) was used for data analysis. Data were expressed as Mean ± SD for quantitative parametric measures, in addition to Median Percentiles for quantitative non-parametric measures and both number and percentage for categorized data. Chi-square test was used to study the association between each 2 variables or comparison between 2 independent groups as regards the categorized data. The probability of error at 0.05 was considered significant while at 0.01 and 0.001 are highly significant.
Results
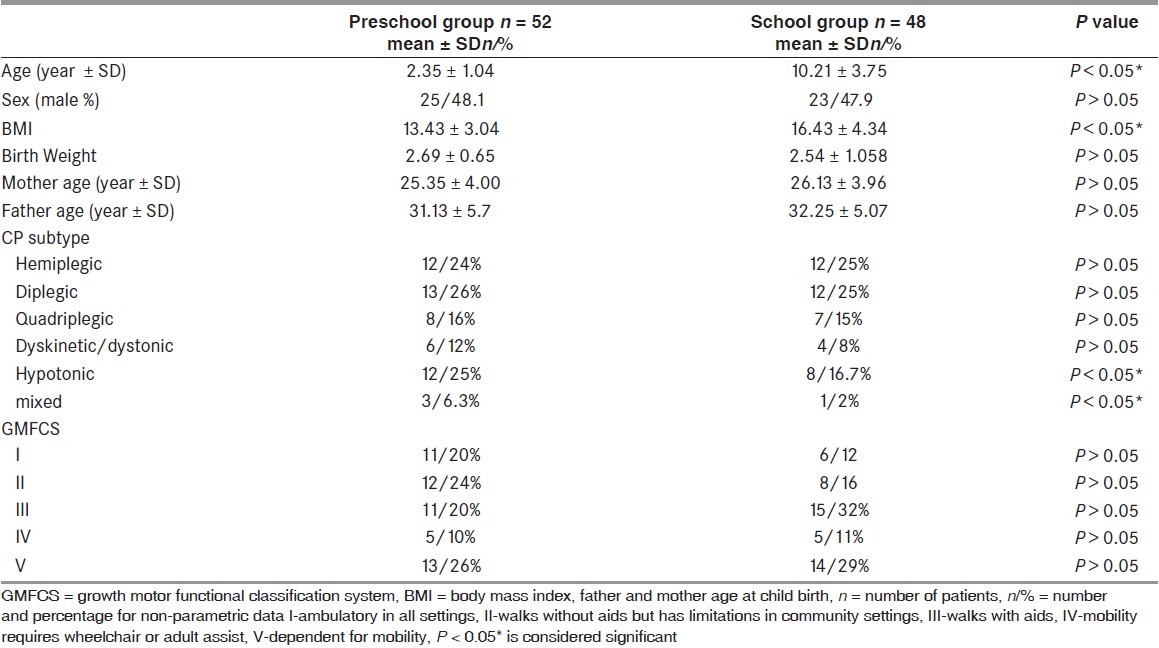
The study included 100 children with cerebral palsy that were subdivided divided into 2 groups: Pre-school age group and school age group. The characteristics of both groups were represented in Table 1.[1] The clinical characteristic of both groups were of no statistically significant differences, except the body mass index (BMI), which was higher at school age group, and also hypotonic and mixed clinical subtypes of CP children were more prevalent at pre-school group.
Table 1.
Clinical characteristics of CP children in both school and pre-school group
Sleep problems in CP children
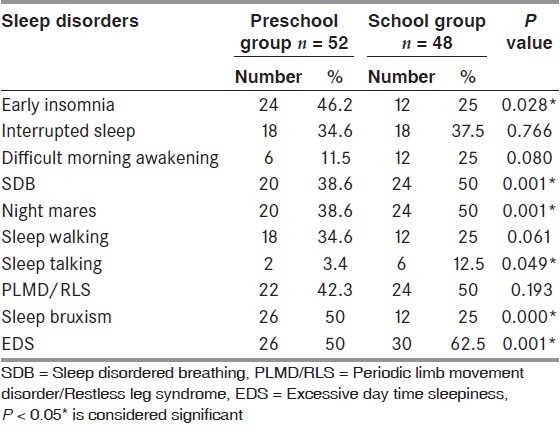
Frequency of sleep problems in CP children were represented in Table 2.[2] Our result revealed high incidence of sleep problem in both pre-school and school age groups. We found that pre-school children have more prevalence of early insomnia (46.2%, P value 0.028) and sleep bruxism (50%, P value 0.000) while school group suffer more sleep disordered breathing (SDB) (50%, P value 0.001), more nightmares (50%, P value 0.001), more sleep talking (12.5% P value 0.049), and more excessive daytime sleepiness (EDS) (62.5%, P value 0.001).
Table 2.
Frequency of sleep problems in pre-school and school age groups of CP children
Correlations of sleep problems to associated medical conditions
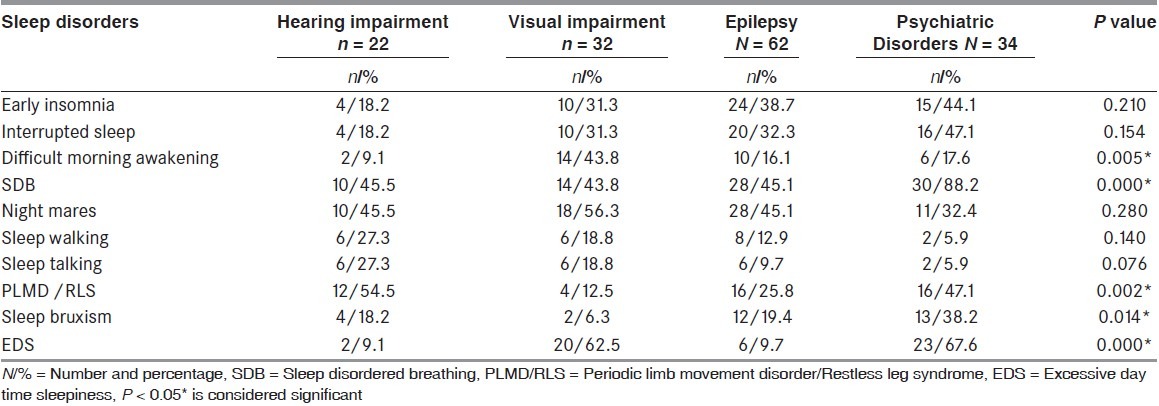
Correlations of sleep problems in CP children with associated medical conditions were represented at Table 3.[3] We studied the correlations between associated hearing, visual impairment, epilepsy, or psychiatric disorders with the prevalence of different sleep disorders. We found positive correlation between difficult morning awakening and visual impairment (P value 0.005), and also positive correlation between SDB and associated psychiatric problems. Periodic limb movement disorder (PLMD)/Restless leg syndrome (RLS) were correlated with hearing problems (P value 0.002), and there were positive correlation between sleep bruxism and psychiatric disorders (P value 0.014). We found also positive correlation between EDS and associated psychiatric problems (P value 0.000).
Table 3.
Correlation between sleep disorders and associated medical conditions
Correlations of sleep problems and clinical subtypes of CP
We studied the correlation between clinical subtypes of CP children and different types of sleep disorders; we found that sleep SDB was the most common complaint in all clinical subtypes.
Correlations of sleep problems and GMFSC
We studied the correlation between GMFSC of CP children and different types of sleep disorders. It was found that insomnia and SDB were more common with grade V and IV while sleep bruxism was more common in GMFSC grade III. However, nightmares and sleep walking were more common in GMFSC grade I and II.
Discussion
Children with CP are prone to sleep problems, with an incidence recently reported to be 23%.[4] These difficulties may include difficulty falling asleep, frequent night awakening, and sleep schedule that does not fit the needs of school or family.[12] Sleep problems in children with CP are under-reported, under recognized, and under-treated.[6] Studies regarding sleep in children with CP are rare due to absence of more simplified methods of assessment rather than polysomnography. The aim of our study was to assess quality of sleep in children with cerebral palsy, using validated sleep questionnaire. Validity of sleep questionnaire for screening of sleep disorders in CP children were studied at many studies.[7,9,13] We found high incidence of sleep problem in both pre-school and school age groups. We found that pre-school children have more prevalence of early insomnia (46.2%, P value 0.028) and sleep bruxism (50%, P value 0.000) while school group suffer more SDB (50%, P value 0.001), nightmares (50%, P value 0.001), sleep talking (12.5% P value 0.049), and EDS (62.5%, P value 0.001). Newman et al.[4] studied a group of 173 children of school age (6 y-11 mon) CP children using sleep disturbance scale[14] and they found that 23% had a pathological total sleep score. Also, they found that specific disorders of initiation and maintenance of sleep, sleep-wake transition of SBD, excessive daytime sleepiness, and arousal were all elevated. Zarowski et al.[15] studied 61 children and adolescents with diagnosis of CP via own questionnaires, and they found the most frequent reported sleep disorders were bruxism 32.8%; legs movement 29.5%; nocturnal enuresis 24.6%; and SBD symptoms like snoring 36.1% in CP group and breathing pauses 14.8%. We studied the correlations of different sleep disorders reported by CP children and the associations of medical problem (visual impairment, hearing impairment, epilepsy, and psychiatric disorders). We found positive correlation between difficult morning awakening and visual impairment (P value 0.005), also positive correlation was found between SDB and associated psychiatric problems. PLMD / RLS were correlated with hearing problems (P value 0.002), and there were positive correlation between sleep bruxism and psychiatric disorders (P value 0.014). Also, positive correlation was found between EDS and associated psychiatric problems (P value 0.000). Newman et al.[4] reported that the principal factor associated with a total sleep disturbance was the presence of active epilepsy, which was also associated with excessive daytime somnolence. However, in epileptic children who were seizure-free, there was neither increase in total sleep problems nor in any of the individual sleep disorders.[4] The interaction between epilepsy and sleep disorders is not well understood, but the most frequently reported problems are those of sleep fragmentation with reduced sleep efficiency and more frequent arousals from sleep.[16] Also, we studied the correlation between clinical subtypes of CP children. We found that sleep SDB was the most common complaint in all clinical subtypes. Newman et al.[4] found that disorders of initiation and maintenance of sleep were more frequent in children with spastic quadriplegia (OR = 12.9, 95% CI 1.9- 88.0), those with dyskinetic CP (OR = 20.6, 95% CI 3.1-135.0), and those with severe visual impairment (OR = 12.5, 95% CI 2.5-63.1). In the current study, we assess the correlation between GMFSC of CP children with sleep disorders, and we found that insomnia and SDB were more common with grade V and IV. Sleep bruxism was more common in GMFSC grade III. While, nightmares and sleep walking were more common in GMFSC grade I and II. In the study of Katanga et al.,[5] the all-night polysomnographic findings of 9 patients with spastic quadriparesis (mean age 36-7 months) were analyzed retrospectively and compared with those of 9 age-matched controls (mean age 37-4 months). The cerebral palsy group had significantly more respiratory disturbances per hour of sleep. Children with neuro-developmental disabilities, such as cerebral palsy, are considered to be a population at risk for the occurrence of sleep problems. It is well-known that the consequences of sleep disorders in children are broad and affect both the child and family.[17] Recent study examined between-group differences in the associations between sleep and quality of life (QOL) between children with CP and their typically developing peers. Insomnia, excessive daytime sleepiness, and functional motor abilities were associated with lower QOL in children with CP. Findings highlight the importance of considering sleep difficulties when addressing the needs of children with CP.[18]
In summary, results of our study indicate that CP children have high incidence of sleep problem in both pre-school and school age groups. Certain types of sleep problems were higher at pre-school group (early insomnia and sleep bruxism) while school group suffer more SDB, nightmares, sleep talking, and EDS. There was association between sleep disorders and associated medical problems like epilepsy, psychiatric disorders, visual and hearing impairment that necessitates more focusing on those special groups. Sleep disorders were found in all clinical subtypes, especially SDB. Also, sleep disorders were present in all GMFCS grades, with more prevalence of insomnia and SDB at severe cases (grade IV and V). Sleep questionnaire can be considered as simple screening method for sleep evaluation of children with CP, with many studies supporting its validity.
Acknowledgment
We would like to thank the children and families participated in this study, also I would like to extend our deepest thanks to my colleagues and professors at pediatric neurology unit of MUCH who helped to collect data of patients.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Blunden S, Lushington K, Lorenzen B, Ooi T, Fung F, Kennedy D. Are sleep problems under-recognized in general practice? Arch Dis Child. 2004;89:708–12. doi: 10.1136/adc.2003.027011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kahn A, Van de Merckt C, Rebuffat E, Mozin MJ, Sottiaux M, Blum D, et al. Sleep problems in healthy preadolescents. Pediatrics. 1989;84:542–6. [PubMed] [Google Scholar]
- 3.Stein MA, Mendelsohn J, Obermeyer WH, Amromin J, Benca R. Sleep and behavior problems in school-aged children. Pediatrics. 2001;107:E60. doi: 10.1542/peds.107.4.e60. [DOI] [PubMed] [Google Scholar]
- 4.Newman C, O'Regan M, Hensey O. Sleep disorders in children with cerebralpalsy. Dev Med Child Neurol. 2006;48:564–8. doi: 10.1017/S0012162206001198. [DOI] [PubMed] [Google Scholar]
- 5.Kotagal S, Gibbons VP, Stith JA. Sleep abnormalities in patients with severe cerebral palsy. Dev Med Child Neurol. 1994;36:304–11. doi: 10.1111/j.1469-8749.1994.tb11850.x. [DOI] [PubMed] [Google Scholar]
- 6.Dominic AF, Jennifer F, Peter PV. Assessing and managing lung disease and sleep disordered breathing in children with cerebral palsy. Paediatr Respir Rev. 2009;10:18–24. doi: 10.1016/j.prrv.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Drake C, Nickel C, Burduvali E, Roth T, Jefferson C, Pietro B. The pediatric day time sleepiness scale (PDSS): Sleep habits and school outcomes in middle school children. Sleep. 2003;15:455–8. [PubMed] [Google Scholar]
- 8.Sleep health centers. Pediatric Sleep Evaluation Questionnaire. http://www.sleephealth.com/existing-patients-questionnaire.htm .
- 9.Chervin RD, Hedger K, Dillon JE, Pituch KJ. Pediatric Sleep Questionnaire (PSQ): Validity and reliability of scale for assessment of sleep disordered breathing, snoring, sleepiness and behavioral problems. Sleep Med. 2000;1:21–32. doi: 10.1016/s1389-9457(99)00009-x. [DOI] [PubMed] [Google Scholar]
- 10.Nelson KB, Ellenberg JH. Children who “outgrew” cerebral palsy. Pediatrics. 1982;69:529–36. [PubMed] [Google Scholar]
- 11.Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Developmental and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–23. doi: 10.1111/j.1469-8749.1997.tb07414.x. [DOI] [PubMed] [Google Scholar]
- 12.Dodge NN. Cerebral palsy: Medical aspects. Pediatr Clin North Am. 2008;55:1189–207. doi: 10.1016/j.pcl.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 13.Chervin RD, Weatherly RA, Garetz SL, Ruzicka DL, Giordani BJ, Hodges EK, et al. Pediatric sleep questionnaire: Prediction of sleep apnea and outcomes. Arch Otolaryngol Head Neck Surg. 2007;133:216–22. doi: 10.1001/archotol.133.3.216. [DOI] [PubMed] [Google Scholar]
- 14.Bruni O, Ottaviano S, Guidetti V, Romoli M, Innocenzi M, Cortesi F, et al. The Sleep Disturbance Scale for Children (SDSC). Construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res. 1996;5:251–61. doi: 10.1111/j.1365-2869.1996.00251.x. [DOI] [PubMed] [Google Scholar]
- 15.Zarowski M, Mojs E, Gajewska E, Steinborn B, Samborski W. Prevalence of sleep problems in children with cerebral palsy.[Preliminary study] Ann Acad Med Stetin. 2008;54:59–64. [PubMed] [Google Scholar]
- 16.Bazil CW. Epilepsy and sleep disturbance. Epilepsy Behav. 2003;4:S39–45. doi: 10.1016/j.yebeh.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 17.Simard-Tremblay E, Constantin E, Gruber R, Brouillette RT, Shevell M. Sleep in children with cerebral palsy: A review. J Child Neurol. 2011;26:1303–10. doi: 10.1177/0883073811408902. [DOI] [PubMed] [Google Scholar]
- 18.Sandella DE, O'Brien LM, Shank LK, Warschausky SA. Sleep and quality of life in children with cerebral palsy. Sleep Med. 2011;12:252–6. doi: 10.1016/j.sleep.2010.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]


