Abstract
Background:
Effectiveness of intermittent short course chemotherapy for tuberculous meningitis (TBM) has not been well studied. There are scarce reported studies on this issue in the world literature. Neurologists all over India are reluctant to accept Directly Observed Treatment Short course (DOTS) for TBM since its introduction in India.
Aim:
We did a prospective study to assess effectiveness of Revised National TB Control Program (RNTCP-DOTS) regimes among TBM patients.
Materials and Methods:
In this study we include the TBM patients admitted from September 2008 to March 2011. All were referred to RNTCP for treatment. Diagnostic Algorithm as per RNTCP guidelines was strictly followed and treatment outcome and follow-up status were recorded. We exclude HIV and pediatric age group.
Results:
A total of 42 cases registered for DOTS regimen were included in the study, of which 35 completed the treatment (83%). All the patients were started with DOTS but finally 78% received actual DOTS. All patients were given 9 months intermitted regimen as per RNTCP guidelines. Seven patients died during the treatment (16%).
Conclusion:
We found intermitted short course chemotherapy was effective in TBM.
Keywords: Directly observed treatment short, Intermitted therapy, tuberculous meningitis
Introduction
Tuberculous meningitis (TBM) is the most serious form of neurotuberculosis. TBM is a common neurological condition causing high mortality and morbidity in developing countries like India.[1] It needs more intensive and prolonged therapy. The central nervous system (CNS) tuberculosis may be in the form of meningitis, intracranial tuberculoma and spinal tubercular arachnoidits and rarely tuberculous encephalopathy. Diagnosis of TBM is a challenge because of manifold clinical presentations and poor sensitivity and specificity of various diagnostic tests.
With the introduction of Revised National TB Control Program (RNTCP), TBM is categorized among extra-pulmonary seriously ill, recommending 2 (HREZ)3 /4 (HR)3 with extension of continuation phase for three more months (total 9 months). But neurologist and physicians are reluctant to accept the intermittent regimen, considering the seriousness of the condition and lack of published studies to prove the effectiveness of intermittent regimen in this situation.[2]
There are only few studies in the literature proving the efficacy of intermitted short course therapy in TBM. Thus the present study was planned to evaluate directly observed treatment, short course in TBM.
Aim
To evaluate effectiveness of RNTCP- Directly Observed Treatment Short course (DOTS) regimen among TBM patients in this study.
Materials and Methods
This is a prospective study of patients with TBM diagnosed in our department. The study period was from September 2008 to March 2011. We diagnosed TBM when patients with meningitis (cerebrospinal fluid [CSF] pleocytosis) were admitted with symptoms lasting 1 week or more, with negative Gram's stain and India ink stains and sterile bacterial cultures, plus one or more of the followings: Cranial computed tomography (CT) scan consistent with TBM (hydrocephalus, basal meningeal enhancement, ring enhancing lesion), chest X-ray consistent with active pulmonary tuberculosis, and good response to antituberculous chemotherapy. The duration of symptoms was calculated as the period from the onset of first symptom to presentation in our center. All patients fulfilled the clinical criteria for TBM.[3] We staged patients according to the Medical Research Council stage.[4]
Category 1 DOTS therapy[5] was given as per RNTCP guidelines for 9 months to all patients, along with corticosteroids for the first 6 weeks. Diagnostic algorithm and follow up of RNTCP were followed. HIV positive cases and bacterial meningitis were excluded.
Results
A total of 42 cases were registered during September 2008 to March 2011. Of the patients enrolled in the study, 23 were males and 19 females. The age distribution was from 16 to 78 years. The majority of case (60%) belonged to the age group 23–47 years.
Majority of them presented with symptoms of headache, vomiting, fever, and altered sensorium. CSF study was abnormal in 40 and 2 of our patients had polymorph dominant (> 40% polymorph) pleocytosis, the duration of illness was < 10 days. The total leukocyte count varied from 52 to 590 with the mean value of 250. A low sugar value below 40% was seen in three patients (7%). Chest X-ray was abnormal in nine cases (21%). Two cases had histologically proven caseous granulomatous axillary lymphadenitis. Fifty percent of patients had Medical Research Council (MRC) stage 3. We did CSF adenosine deaminase (ADA) levels estimated in 29 patients and all showed values > 10 μ/l. Polymerase chain reaction (PCR) was done in two samples and was negative. Four cases (9%) was CSF acid-fast bacillus (AFB) stain positive.
Of the 42 patients, 30 had done CT scan after admission. Fourteen of 35 (40%) showed abnormalities in form of multiple lacunar infarct, hydrocephalus, basal meningeal enhancement. MRI was performed late in 11 patients, out of whom 4 showed additional granuloma and 2 leptomeningeal enhancement. Patients were followed up monthly for 6 months and there was no relapse.
Seven patients died, one patients due to drug-induced hepatitis, four patients due to ventriculoperitoneal shunt-related surgical procedures, infection, aspiration pneumonia, and raised intracranial pressure. One patient due to unrelated gastroenteritis within first week of starting the treatment and one patient after 3 months of treatment had multiple granulomas and was very sick. Two patients were converted to daily regimen later on due to clinical jaundice and persistent vomiting. Six patients had sequel of hemi paresis, seizures, vision impairment (due to bilateral optic atrophy).
Discussion
India is among the nations with high incidence of TB. Usually there are 20% of extra pulmonary cases of whom 15% will be neuro tuberculosis.[6] Standardized treatment means that all patients in a defined group receive the same treatment regimen. Standard regimens have the following advantages over individualized prescription of drugs:
Errors in prescription—and thus the risk of development of drug resistance—are reduced;
estimating drug needs, purchasing, distribution, and monitoring are facilitated;
Staff training is facilitated;
costs are reduced;
maintaining a regular drug supply when patients move from one area to another is made easier; and
Outcome evaluation is convenient and results are comparable.
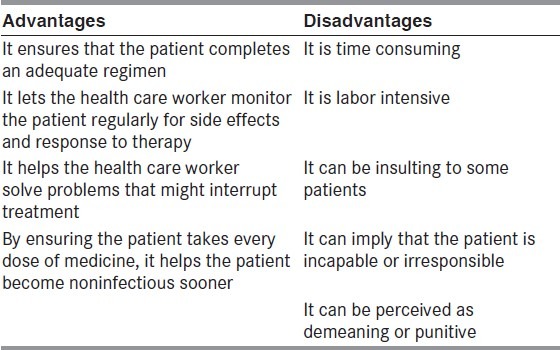
Advantages and Disadvantages of DOT [Table 1]
Table 1.
Advantages and Disadvantages of DOT
On above background lype et al. did retrospective analysis of DOTS in TBM to look at the presentation, management, and outcome in 11 patients. One died following hepatitis and another patient died of unrelated gastroenteritis. They found DOTS to be effective in TBM (90.9%)[1]
Venugopal et al. registered 32 cases of neuro tuberculosis for DOTS regimen in their study, of whom 29 completed treatment and all were asymptomatic at the end of treatment (85%). All patients in their study were given 9 months intermittent regimen as per RNTCP guidelines. Five patients (14%) died during treatment. Their result shows that intermittent short course chemotherapy under field program conditions was efficient in curing neuro tuberculosis.[2]
Most of our patients presented to us in MRC stage 3. We found DOTS to be effective in TBM (83%). We had good follow up through the RNTCP network and there were no drop out from our study. This could probably be due to easy availability of drugs, seriousness of disease, and supervision of drug intake.[7–9] The mortality was 16%, one of known variables, that is, 50% MRC stage 3 at the time of initiation of treatment.
In the present study, the survival with sequele is 17% due to most of our patients had advanced disease. When comparing with previously published studies which shows mortality up to 75% and sequele up to 85%, this data seems to be significant.[10,11]
In our series, there was a high prevalence of extra cranial tuberculosis, which gave a clue to the diagnosis. This emphasizes the importance of a thorough search for tuberculosis anywhere in patients with suspected TBM. TB PCR had a low yield in our series.
Use of DOTS and steroids was favorable in our study; still this recommendation needs verification in large sample study. The high sensitivity of CSF ADA test that was seen in this study is consistent with the literature available showing that ADA can have sensitivity and specificity as high as 83% and 95%, respectively.[12] Contrast enhanced MRI is more likely than Contrast enhanced CT scan to reveal abnormalities in TBM. Hence MRI with Contrast should be part of the work up of suspected cases of TBM.
With the intermittent short course regimen, total drug consumed by the patient is almost half than that with the conventional daily regimen. The toxicity is less and cost of therapy is considerably low. Hence, this regimen can be universally recommended for all cases of tuberculosis including TBM, especially in developing countries like India. A large sample prospective study should be undertaken to support this. MRI scan with contrast study is an important tool in the diagnosis of TBM and can pick up findings that can be missed in a CT scan. CSF ADA estimation in the CSF is more rewarding than CSF PCR. Looking for evidence of extra cranial tuberculosis is very fruitful.
Conclusions
DOTS regimen for TBM is an effective regimen under program conditions.
Default rate is negligible for this intermittent short course chemotherapy.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Iype T, Chacko S, Raghavan S, Mathew R, Mohan M. Preliminary report of directly observed treatment, short course in tuberculous Meningitis. Ann Indian Acad Neurol. 2010;13:57–60. doi: 10.4103/0972-2327.61279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Venugopal K, Sreelatha PR, Philip S, Kumar V. Treatment outcome of neuro tuberculosis patients put on dots- An observation study from the field. Indian J Tuberc. 2008;55:199–202. [PubMed] [Google Scholar]
- 3.Ahuja GK, Mohan KK, Prasad K, Behari M. Diagnostic criteria for tuberculous and their validation. Tuber Lung Dis. 1994;75:149–52. doi: 10.1016/0962-8479(94)90045-0. [DOI] [PubMed] [Google Scholar]
- 4.Medical Research Council Streptomycin in tuberculous trials committee. Streptomycin treatment of tuberculous meningitis. Lancet. 1948;75:582–96. [Google Scholar]
- 5.Gothi D, Joshi JM. Clinical and laboratory observations of tuberculosis at a Mumbai (India) clinic. Postgrad Med J. 2004;80:97–100. doi: 10.1136/pmj.2003.008185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prabhakar S, Thussu A. CNS Tuberculosis. Neurology India. 1997;45:132–40. [PubMed] [Google Scholar]
- 7.Fallon RJ, Kennedy DH. Treatment and prognosis in tuberculous meningitis. J Infect. 1981;3:39–44. doi: 10.1016/s0163-4453(81)80007-2. [DOI] [PubMed] [Google Scholar]
- 8.Wang JT, Hung CC, Sheng WH, Wang JY, Chang SC, Luh KT. Prognosis of tuberculous meningitis in adults in the era of modern antituberculous chemotherapy. J Microbiol Immunol Infect. 2002;35:215–22. [PubMed] [Google Scholar]
- 9.Ramachandran P, Duraipandian M, Nagarajan M, Prabhakar R, Ramakrishnan CV, Tripathy SP. Three chemotherapy studies of tuberculous meningitis in children. Tubercle. 1986;67:17–29. doi: 10.1016/0041-3879(86)90028-0. [DOI] [PubMed] [Google Scholar]
- 10.Karande S, Gupta V, Kulkarni M, Joshi A. Prognostic clinical variables in childhood tuberculous meningitis: An experience from Mumbai, India. Neurol India. 2005;53:191–5. doi: 10.4103/0028-3886.16407. discussion 195-6. [DOI] [PubMed] [Google Scholar]
- 11.Satya G, Kamlesh C. Tuberculosis Meningitis in Children. Indian J Tuberculosis. 1981;28:3–11. [Google Scholar]
- 12.Choi SH, Kim YS, BaeI G, Chung JW, Kang JM, et al. The possible role of cerebrospinal fluid adenosine deaminase activity in the diagnosis of meningitis in adults. Clin Neurosurg. 2002;104:10–5. doi: 10.1016/s0303-8467(01)00159-7. [DOI] [PubMed] [Google Scholar]


