Abstract
Headache is the most common symptom of cerebral venous thrombosis (CVT); however, the detailed underlying mechanisms and characteristics of headache in CVT have not been well described. Here, we report two cases of CVT whose primary and lasting presentation was orthostatic headache, suggestive of decreased intracranial pressure. Contrary to our expectations, the headaches were associated with elevated cerebrospinal fluid (CSF) pressure. Magnetic resonance imaging and magnetic resonance venography showed characteristic voiding defects consistent with CVT. We suggest that orthostatic headache can be developed in a condition of decreased intracranial CSF volume in both intracranial hypotensive and intracranial hypertensive states. In these cases, orthostatic headache in CVT might be caused by decreased intracranial CSF volume that leads to the inferior displacement of the brain and traction on pain-sensitive intracranial vessels, despite increased CSF pressure on measurement. CVT should be considered in the differential diagnosis when a patient complains of orthostatic headache.
Keywords: Cerebral venous thrombosis, cerebrospinal fluid, intracranial pressure, orthostatic headache
Introduction
The severity and clinical manifestations of cerebral venous thrombosis (CVT) are highly variable, and may include headache, seizure, altered mentality and aphasia.[1,2] Because of its potential morbidity, the timely diagnosis of CVT is crucial. Various types of headache are the most common symptoms of CVT, and elevated intracranial pressure resulting from CVT is the most reasonable explanation so far.[3–5] However, because of its heterogeneous presentation, the underlying mechanisms of each headache type in CVT remain poorly understood. Here, we describe two patients who presented with orthostatic headaches as the main clinical manifestation that were associated with intracranial hypertension as a manifestation of CVT. Although CVT secondary to spontaneous intracranial hypotension (SIH) and secondary orthostatic headache in CVT after an epidural patch have been reported previously, orthostatic headache as the primary manifestation of CVT has not been described.[6,7] We suggest a possible underlying mechanism for orthostatic headache in CVT.
Case Reports
Case 1
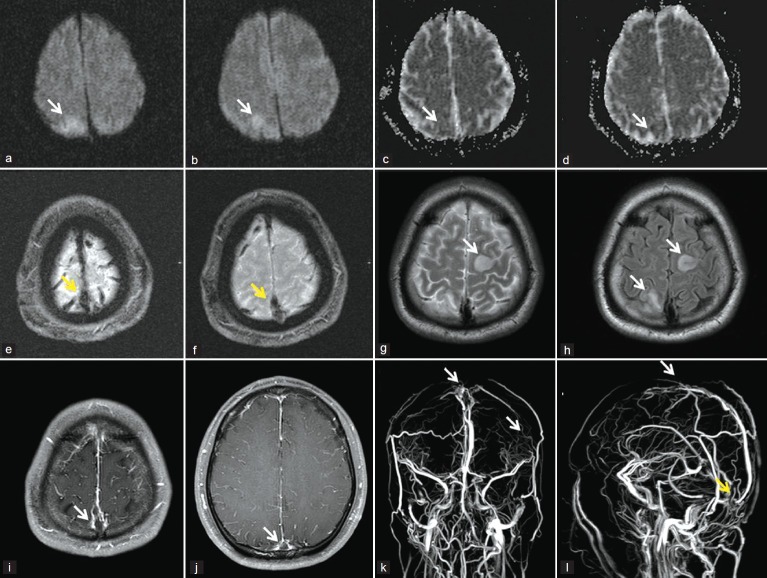
A previously healthy 19-year-old man admitted with a 2-day history of headache. The headache was localized to the occipital area, severe in intensity and throbbing in nature. Typically, the headache in this patient was position-dependent, and developed with orthostatic posture, leading to severe intensity in the upright position (visual analogue scale [VAS] 9–10/10), and was relieved when the patient was in the recumbent position. Routine neurologic examination and laboratory findings were normal. Initial computerized tomography (CT) of the brain showed no abnormalities. Cerebrospinal fluid (CSF) tapping was done under the suspicion of SIH, but the opening pressure was over 40 cmH2O (normal range: 8-18 cmH2O), indicating increased intracranial pressure (IICP). After admission, the patient developed left upper extremity monoparesis with intermittent clonic movement, followed by generalized tonic movement. Diffusion-weighted magnetic resonance imaging (MRI) (DWI) of the brain was performed immediately after the episode. The b-value of 1000 s/mm2 and apparent diffusion coefficient (ADC) image of the DWI showed high signal intensity in the right parietal cortex, suggesting vasogenic edema [Figure 1a-b]. Gradient-echo imaging (GRE) identified superior sagittal sinus (SSS) and cortical vein dilatation [Figure 1e and f]. Subsequent MRI revealed right parietal, left frontal cortex high-signal intensity on T2-weighted and fluid-attenuated inversion recovery images, with an empty delta sign on gadolinium-enhanced T1-weighted images [Figure 1g-j]. There was no evidence to suggest SIH on MRI, such as pachymeningeal enhancement or downward brain displacement. Brain MR venography (MRV) revealed the absence of the SSS, straight sinus and right transverse sinus [Figure 1k and l]. We made a diagnosis of CVT with venous infarction according to the established criteria[5] to which the patient's headache and seizure were attributed. Further laboratory tests for causative medical conditions showed deficiencies in protein C (16%, normal range: 70- 130%) and protein S (33%, normal range: 74- 146%). The headache and seizure completely subsided after intravenous anticoagulation treatment. He remained asymptomatic without any neurological sequelae after 10 months of follow-up.
Figure 1.
Diffusion-weighted MRI showed diffusion restriction with high signal intensity (HI) of the right parietal cortex on ADC map (arrows), suggesting vasogenic edema (a-d). Dilatation of cortical veins and superior sagittal sinus on gradient echo images (arrows) (e, f). T2- and FLAIR MRI showed HI over the left frontal and right parietal cortex (arrows) (g, h). Gadolinium-enhanced T1-weighted MRI showed the “empty delta sign” (arrows) (i, j). MRV revealed the absence of the superior sagittal sinus, straight sinus, and right transverse sinus, indicating cerebral venous thrombosis (k, l)
Case 2
A previously healthy 29-year-old man visited the hospital complaining of headache for the past day. The headache was localized to the bifrontal–temporal area with moderate to severe intensity (VAS 7–8/10), and was squeezing in nature. The symptoms developed only when the patient stood up, and were partially relieved when lying down (VAS 2-3/10). We performed CSF tapping and checked intracranial pressure under suspicion of SIH. However, the CSF opening pressure was 36 cmH2O (normal range: 8-18 cmH2O). MRI of the brain showed no definite parenchymal lesion, but gadolinium-enhanced T1-weighted images revealed the empty delta sign with enhancement of the collateral veins in the SSS walls surrounding a non-enhanced thrombus in the sinus. Also, there were no findings suggesting SIH. MRV revealed a voiding defect in the SSS, right transverse sinus and right sigmoid sinus. Diagnosis of CVT according to the clinical presentation and imaging findings was made. The patient's headache near completely subsided after intravenous anticoagulation treatment. He remained asymptomatic after 13 months of follow-up.
Discussion
Diverse presentation of headaches and other neurological symptoms complicate the diagnosis of CVT.[4,7] Although still not thoroughly understood, intracranial hypertension, venous distension and abnormal cerebral venous circulation, individually or in combination, are the possible pathogenic mechanisms of headache in CVT patients.[3,4] In the present two cases, initial complaint of position-dependent orthostatic headache was associated with intracranial hypertension, which was contrary to our expectations. We had suspected that the orthostatic headaches in these patients arose from SIH or headache secondary to CSF leakage.
We excluded secondary CVT as a complication of SIH using several criteria. The orthostatic nature of the headache throughout the morbid period did not change. Furthermore, the time interval from headache development to examining the CSF pressure was just 2 days and 1 day, respectively. The orthostatic headache also persisted during lumbar puncture, and there were no imaging findings suggestive of SIH. We suspected orthostatic headache associated with CVT in both patients based on the “Monro-Kellie Doctrine.”[8,9]
Intracranial constituents (blood, CSF and brain tissues) normally create a state of volume equilibrium. In CVT patients, blood volume increases due to insufficient venous drainage and CSF volume consequently decreases in the intracranial portion of the brain to maintain equilibrium. Intracranial CSF hypovolemia shifts the brain tissue downward and increases traction on the pain-sensitive intracerebral vessels that might be aggravated in the upright posture and relieved in the supine position, as in SIH. Under this hypothesis, posture-dependent headache in two patients with CVT can be expected to worsen when patients are standing or sitting upright despite the presence of significantly increased intracranial pressure.[10] Paradoxically, this hypothesis can also be applied to the pathogenesis of headaches in SIH. In SIH-related headaches, CSF hypovolemia directly causes downward displacement of brain tissue followed by traction of the pain-sensitive blood vessels. The contrary conditions of intracranial hypertension and hypotension may result in the same clinical symptoms through a common mechanism. In our cases, the nature of the headache sustained constant through clinical courses from symptom onset, and orthostatic headache still persisted when we measured the increased CSF pressure with the presence of CVT. These findings might be one of the possible evidences of CVT; in our cases, they are not secondary to SIH.
In summary, we suggest that decreased intracranial CSF volume could be the underlying mechanism of orthostatic headache in CVT patients. CVT should also be considered in the differential diagnosis of patients with posture-dependent headache, given that orthostatic headache can develop in conditions of either increased or decreased intracranial pressure.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.English JD, Fields JD, Le S, Singh V. Clinical Presentation and long-term outcome of cerebral venous thrombosis. Neurocrit Care. 2009;11:330–7. doi: 10.1007/s12028-009-9234-8. [DOI] [PubMed] [Google Scholar]
- 2.Ferro JM, Canhao P, Stam J, Bousser MG, Barinagarrementeria F. Prognosis of cerebral vein and dural sinus thrombosis: Results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT) Stroke. 2004;35:664–70. doi: 10.1161/01.STR.0000117571.76197.26. [DOI] [PubMed] [Google Scholar]
- 3.Agostoni E, Aliprandi A. Alterations in the cerebral venous circulation as a cause of headache. Neurol Sci. 2009;30:S7–10. doi: 10.1007/s10072-009-0052-8. [DOI] [PubMed] [Google Scholar]
- 4.Alberti A, Venti M, Biagini S. Headache and cerebral vein and sinus thrombosis. Front Neurol Neurosci. 2008;23:89–95. doi: 10.1159/000111263. [DOI] [PubMed] [Google Scholar]
- 5.Saposnik G, Barinagarrementeria F, Brown RD, Jr, Bushnell CD, Cucchiara B, Cushman M, et al. Diagnosis and management of cerebral venous thrombosis: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:1158–92. doi: 10.1161/STR.0b013e31820a8364. [DOI] [PubMed] [Google Scholar]
- 6.Ravindran RS, Zandstra GC, Viegas OJ. Postpartum headache following regional analgesia; a symptom of cerebral venous thrombosis. Can J Anaesth. 1989;36:705–7. doi: 10.1007/BF03005426. [DOI] [PubMed] [Google Scholar]
- 7.Bousser MG, Ferro JM. Cerebral venous thrombosis: An update. Lancet Neurol. 2007;6:162–70. doi: 10.1016/S1474-4422(07)70029-7. [DOI] [PubMed] [Google Scholar]
- 8.Mokri B. The Monro-Kellie hypothesis: Applications in CSF volume depletion. Neurology. 2001;56:1746–8. doi: 10.1212/wnl.56.12.1746. [DOI] [PubMed] [Google Scholar]
- 9.Neff S, Subramaniam RP. Monro-Kellie doctrine. J Neurosurg. 1996;85:1195. [PubMed] [Google Scholar]
- 10.Miyazawa K, Shiga Y, Hasegawa T, Endoh M, Okita N, Higano S, et al. CSF hypovolemia vs intracranial hypotension in “spontaneous intracranial hypotension syndrome. Neurology. 2003;60:941–7. doi: 10.1212/01.wnl.0000049933.51044.81. [DOI] [PubMed] [Google Scholar]