Abstract
Objectives
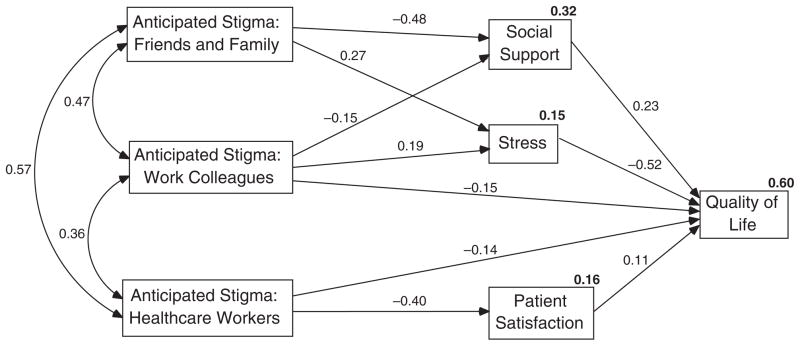
We examined the process by which anticipated stigma relates to quality of life among people living with chronic illnesses. We hypothesized that stress, social support and patient satisfaction mediate the relationships between three sources of anticipated stigma and quality of life.
Methods
Data were collected from adults living with chronic illnesses recruited from support groups and online communities, and were analysed with path analysis.
Results
Results demonstrated that stress mediated the relationships between anticipated stigma from friends and family, and work colleagues with quality of life; social support mediated the relationships between anticipated stigma from friends and family, and work colleagues with quality of life; and patient satisfaction mediated the relationship between anticipated stigma from healthcare providers with quality of life. The final path model fit the data well (χ2 (8)=8.66, p=0.37; RMSEA=0.02; CFI=0.99; SRMR=0.03), and accounted for 60% of the variance in participants’ quality of life.
Discussion
This work highlights potential points of intervention to improve quality of life. It calls attention to the importance of differentiating between sources of anticipated stigma in clinical settings, interventions and research involving people living with chronic illnesses.
Keywords: Chronic illness, anticipated stigma, quality of life, stress, social support
Introduction
Chronic illnesses such as epilepsy, multiple sclerosis and inflammatory bowel disease carry social stigma.1 People diagnosed with chronic illnesses report experiencing social rejection,2 workplace termination3 and poor healthcare4 due to their chronic illness. Importantly, people living with chronic illnesses may come to anticipate stigma. Anticipated stigma is the belief that prejudice, discrimination and stereotyping will be directed at the self from others in the future.5,6 People living with chronic illnesses who anticipate stigma expect that others will devalue them based on their chronic illness. Although research has demonstrated that anticipated stigma undermines the physical and mental well-being of people living with chronic illnesses,6–9 critical gaps remain in understanding the process whereby anticipated stigma contributes to well-being. Illuminating this process may identify points of intervention to improve the well-being of people living with chronic illnesses. In previous work we examined the association between stigma mechanisms (i.e. internalized, experienced and anticipated stigma) and quality of life in healthcare contexts specifically.10 We now extend this work to other social contexts by examining the association between anticipated stigma from multiple sources – friends and family, work colleagues and healthcare workers – and quality of life. Additionally, we examine three mediators of the relationships between anticipated stigma and quality of life: stress, social support and patient satisfaction.
Stress results from a discrepancy between the demands of a situation and the resources that an individual possesses to meet those demands.11 In the case of anticipated stigma, expected experiences of prejudice, discrimination and stereotyping place demands on people living with chronic illness. People living with chronic illness who do not have adequate psychological, physical, economic and/or social resources to handle these demands will experience increased stress. Stress may be associated with anticipated stigma from multiple sources or different people. For example, people living with chronic illnesses may perceive social rejection from friends and family, discrimination from work colleagues and poor caregiving from healthcare workers as demands that they do not have the resources to handle. Stress, in turn, is related to decreased mental and physical health among people living with chronic illness.12–14
Anticipated stigma may also be associated with decreased social support experienced by people living with chronic illness. Social support involves comfort, assistance and/or information that individuals receive from others.15 People living with concealable stigmatized identities who experience stigma are more likely to socially isolate themselves, and this social isolation is associated with decreased social support.16 Although not all chronic illnesses are concealable, people living with chronic illnesses who anticipate stigma may likewise be more likely to socially isolate themselves and therefore receive less social support. Because friends, family and work colleagues represent critical sources of social support,17 people living with chronic illnesses who anticipate stigma from friends and family as well as work colleagues may be particularly likely to experience decreased social support. Among people living with chronic illness, decreased social support is related to poorer mental and physical health.17–20
Finally, anticipated stigma from healthcare providers may be associated with decreased patient satisfaction among people living with chronic illness. People living with chronic illness who anticipate stigma from their healthcare providers may be less open about their symptoms and illness-related concerns with their healthcare providers. This decreased openness may impede the ability of healthcare providers to offer satisfactory care. Patient satisfaction, in turn, is related to well-being. People living with chronic illness who are less satisfied with their healthcare suffer poor health-related outcomes.21
In the current work, we hypothesize that stress mediates the relationship between anticipated stigma from friends and family, work colleagues and healthcare workers with quality of life; social support mediates the relationship between anticipated stigma from friends and family, and work colleagues and quality of life; and patient satisfaction mediates the relationship between anticipated stigma from healthcare providers and quality of life.
Method
Procedure and participants
The current study was approved by the University of Connecticut Institutional Review Board. The recruitment method was multipronged to reach a diverse sample. Adults living with chronic illnesses were recruited for participation in person from support groups and events for people living with chronic illnesses as well as online from websites that serve people living with chronic illnesses. Participants recruited in person completed a paper version of the study whereas participants recruited from websites completed an online version. Of the 172 people living with chronic illnesses who ultimately completed the study, 53 completed it in person and 119 completed it online. All participants provided consent via an information sheet. The study involved completion of a series of questionnaires.
Measures
Demographics and chronic illness description
Participants reported their age, gender, race/ethnicity, relationship status and family income. They also listed their chronic illnesses and indicated the chronic illness that impacts their life the most. Participants were then instructed to answer the remaining questions with respect to the illness that impacts their life the most. Next, participants indicated how long they had been living with their chronic illness. This number was divided by their age to create a variable representing the proportion of their life that they had lived with their chronic illness. Participants provided information about the extent to which their chronic illness affects their life by answering the question ‘How much does your chronic illness affect your life?’ on a scale from 1 (not at all) to 4 (very much). They also provided information about their health by answering the question ‘How would you describe your health in general?’ on a scale from 1 (poor) to 5 (excellent).
Anticipated stigma
Anticipated stigma was measured using the Chronic Illness Anticipated Stigma Scale (CIASS).22 The CIASS includes three subscales, measuring the extent to which participants anticipate stigma from friends and family members, work colleagues and healthcare workers. Items included ‘A friend or family member will blame you for not getting better’ (friends and family subscale), ‘Someone at work will discriminate against you’ (work colleagues subscale) and ‘A healthcare worker will give you poor care’ (healthcare subscale). Participants responded to items on a scale from 1 (very unlikely) to 5 (very likely). Items from the three subscales were averaged to create an anticipated stigma from friends and family score (α=0.91), work colleagues score (α=0.91) and health-care workers score (α=0.92).
Stress
The 10-item Perceived Stress Scale (PSS)23 assessed how unpredictable, uncontrollable and overloaded participants feel that their lives are. Participants were asked to indicate how often they have felt or thought a certain way in the past month on a scale from 1 (never) to 5 (very often). Items included ‘In the last month, how often have you felt that you were unable to control the important things in your life?’ A stress score was derived by averaging scale items (α=0.91).
Social support
The Multidimensional Scale of Perceived Social Support24 assessed participants’ perceptions of the amount of emotional and instrumental support that they receive from others. Because the study was not focused on significant others, items referring to significant others were not used. Participants were asked whether they agree with 8 statements on a scale from 1 (strongly disagree) to 5 (strongly agree). Items included ‘My family really tries to help me’ and ‘I can talk about my problems with my friends.’ A social support score was derived by averaging scale items (α=0.90).
Patient satisfaction
Patient satisfaction was measured using the overall satisfaction subscale of the Primary Care Provider Questionnaire.25 Participants were asked to indicate their agreement with four items describing their satisfaction with the care given by the doctor who treats their chronic illness on a scale from 1 (strongly disagree) to 5 (strongly agree). Items included ‘I am very satisfied with the medical care I receive from this doctor.’ A patient satisfaction score was created by averaging subscale items (α=0.91).
Quality of life
Quality of life was evaluated using the brief version of the World Health Organization’s Quality of Life Scale,26 which includes 26 items. Responses are measured on a 5-point scale with anchors tailored to each item. Items included ‘Do you have enough energy for everyday life?’ The anchors for this item included 1 (not at all), 2 (a little), 3 (moderately), 4 (mostly) and 5 (completely). A quality of life score was derived by averaging all scale items (α=0.93).
Results
Sample characteristics
Participant demographics and illness characteristics are presented in Table 1. Participants ranged in age from 18 to 78 years old, with a mean age in the mid-40s. The majority of participants identified as female, White or European-American and married. Family income was fairly evenly distributed. Participants reported living with between 1 and 8 chronic illnesses (Mdn=1). The most common illnesses in the sample included inflammatory bowel disease, multiple sclerosis, fibromyalgia, epilepsy and lupus. Participants with these five diseases comprised 78.6% of the total sample. Participants reported living with their chronic illnesses between less than 1 year and 66 years (M=10.20, SD=11.76). On average, participants reported living with their chronic illness for 23% of their lives, that their health condition ‘somewhat’ to ‘very much’ affected their lives, and that their health in general was ‘fair.’
Table 1.
Participant demographic and illness characteristics (N=172)
| N | % | M | SD | |
|---|---|---|---|---|
| Age | 43.68 | 13.29 | ||
| Gender | ||||
| Female | 133 | 77.3 | ||
| Male | 38 | 22.1 | ||
| Race/Ethnicity | ||||
| White/European-American | 154 | 89.5 | ||
| Black/African-American | 5 | 2.9 | ||
| Latino(a)/Hispanic-American | 4 | 2.3 | ||
| Asian/Asian-American | 3 | 1.7 | ||
| Native American | 3 | 1.7 | ||
| Multi-racial | 2 | 1.2 | ||
| Relationship Status | ||||
| Married | 97 | 56.4 | ||
| Single | 27 | 15.7 | ||
| Living as married | 14 | 8.1 | ||
| Divorced | 14 | 8.1 | ||
| Dating | 13 | 7.6 | ||
| Separated | 5 | 2.9 | ||
| Widowed | 2 | 1.2 | ||
| Family Income | ||||
| <$49,000 | 54 | 31.4 | ||
| $50,000–$99,999 | 61 | 35.5 | ||
| >$100,000 | 45 | 26.2 | ||
| Number of Chronic Illnesses | 1.88 | 1.36 | ||
| Most Common Chronic Illnesses | ||||
| Inflammatory bowel disease | 55 | 32.0 | ||
| Multiple sclerosis | 28 | 16.3 | ||
| Fibromyalgia | 26 | 15.1 | ||
| Epilepsy | 13 | 7.6 | ||
| Lupus | 13 | 7.6 | ||
| Proportion of Life with Illness | 0.23 | 0.18 | ||
| Illness Affects Life | 3.65 | 0.64 | ||
| General Health | 2.70 | 0.93 | ||
Note: Illness affects life was measured on a 4-point Likert scale, while general health was measured on a 5-point Likert scale.
Path model
Descriptive statistics are included in Table 2. Participants reported that it was unlikely to somewhat likely that they would experience stigma from their friends and family, work colleagues and healthcare workers. A repeated measures ANOVA revealed a multivariate effect of source, F (2, 156)=37.18, p<0.001, ηp2=0.32, demonstrating that participants anticipated different amounts of stigma from different sources. Bonferonni adjusted post hoc tests demonstrated that participants anticipated greater stigma from work colleagues than from friends and family or healthcare workers (all ps<0.001). Additionally, participants reported high levels of social support, and moderate levels of stress, patient satisfaction and quality of life.
Table 2.
Descriptive statistics and correlations between variables
| Mean (SD) | CIASS: Friends and Family | CIASS: Work Colleagues | CIASS: Healthcare | Social Support | Stress | Patient Satisfaction | |
|---|---|---|---|---|---|---|---|
| Anticipated stigma: Friends and family | 2.22 (1.12) | — | |||||
| Anticipated stigma: Work colleagues | 3.08 (1.19) | 0.46** | — | ||||
| Anticipated stigma: Healthcare | 2.35 (1.10) | 0.57** | 0.34** | — | |||
| Social support | 3.93 (0.84) | −0.55** | −0.38** | −0.24* | — | ||
| Stress | 3.12 (0.75) | 0.35** | 0.30** | 0.22* | −0.30** | — | |
| Patient satisfaction | 3.32 (1.06) | −0.23* | −0.18*** | −0.41** | 0.15*** | −0.20* | — |
| Quality of life | 3.27 (0.66) | −0.47** | −0.45** | −0.40** | 0.48** | −0.67** | 0.33** |
Note:
p<0.01,
p<0.001,
p<0.05.
The data were analysed using path analysis in AMOS 17.0. Anticipated stigma from friends and family, work colleagues and healthcare workers were included in the model as exogenous variables and social support, stress and patient satisfaction were endogenous variables. First, the saturated model was examined. Next, non-statistically significant paths were trimmed.27 Figure 1 presents the final path model. The figure includes the correlation statistics for the exogenous variables, the standardized regression weights for all non-trimmed paths, and the squared multiple correlation statistics for all endogenous variables. Model fit indices revealed that the model is a good fit for the data, χ2 (8)=8.66, p=0.37; RMSEA=0.02 (CI=0.00–0.09); CFI=0.99; SRMR= 0.03. The entire model accounted for 60% of the variance in participants’ quality of life.
Figure 1.
Final path model.
As shown in the model, anticipated stigma from friends and family members, work colleagues and healthcare workers were all positively correlated (all ps<0.001), indicating that greater anticipated stigma from one source was associated with greater anticipated stigma from other sources. The majority of the hypothesized relationships were supported by the model. Participants who anticipated greater stigma from friends and family members as well as work colleagues experienced greater stress, and participants who experienced greater stress had a lower quality of life. The model did not support the hypothesized relationship between anticipated stigma from healthcare workers and stress. Next, participants who anticipated greater stigma from friends and family members and from work colleagues perceived less social support, and participants who perceived less social support had a lower quality of life. Finally, participants who anticipated greater stigma from healthcare workers reported lower patient satisfaction, and participants who were less satisfied with their healthcare reported a lower quality of life.
The direct and indirect effects were examined next to evaluate potential mediation within the model. The path analysis was performed with bootstrapping to acquire tests of statistical significance of the direct and indirect effects. Anticipated stigma from friends and family members had an indirect effect on quality of life of −0.25 (p=0.02) and no direct effect, suggesting that stress and social support fully mediated the relationship between anticipated stigma from friends and family and quality of life. Anticipated stigma from work colleagues had an indirect effect on quality of life of −0.13 (p=0.01) and a direct effect of −0.15 (p=0.06), suggesting that stress and social support partially mediated the relationship between anticipated stigma from work colleagues and quality of life. Finally, anticipated stigma from healthcare workers had an indirect effect on quality of life of −0.05 (p=0.02) and a direct effect of −0.14 (p=0.02), suggesting that patient satisfaction partially mediated the relationship between anticipated stigma from healthcare workers and quality of life.
Discussion
Summary of main findings
We examined the process whereby anticipated stigma undermines the quality of life of people living with chronic illnesses. Similar to past work demonstrating the negative impact of anticipated stigma,6–9 we found that anticipated stigma from friends and family, work colleagues and healthcare workers was associated with lower quality of life. Supporting our hypotheses, stress mediated the relationship between anticipated stigma from friends and family, and work colleagues with quality of life. However, stress did not mediate the relationship between anticipated stigma from healthcare workers and quality of life. Social support mediated the relationship between anticipated stigma from friends and family, and work colleagues with quality of life. Patient satisfaction mediated the relationship between anticipated stigma from healthcare workers and quality of life. Therefore, people living with chronic illnesses who anticipate greater stigma experience lower quality of life; and this relationship is explained, in part, by higher stress, lower social support and lower patient satisfaction associated with anticipated stigma. Importantly, this work suggests that people living with chronic illnesses do not have to actually experience enacted stigma (i.e. experiences of prejudice, stereotyping and discrimination directed at the self from others5) to suffer negative outcomes associated with stigma. They merely have to believe that it may occur to them in the future.
Further, the model accounted for 60% of the variance in participants’ quality of life. This suggests that the variables in the model – including anticipated stigma, stress, social support and patient satisfaction – play a significant role in the well-being of people living with chronic illnesses.
Strengths and limitations of work
The main strength of the current work is its nuanced approach to studying the relationship between stigma and well-being among people living with chronic illnesses. First, the work explores mediators of the relationship between anticipated stigma and quality of life. In doing so, it illuminates the process whereby anticipated stigma ultimately impacts the well-being of people living with chronic illnesses. Second, the work differentiates sources of anticipated stigma, including friends and family, work colleagues, and healthcare workers, improving on past research7,28 that examined anticipated stigma from others in general only. This work contributes to recent research demonstrating that people living with stigmatized identities experience different amounts of stigma from different sources and that stigma from different sources impacts people living with stigmatized identities in different ways.29 Future work should continue to differentiate between sources of stigma to best understand how to reduce the impact of stigma for people living with chronic illnesses.
The cross-sectional design of the current study limits our ability to form firm conclusions regarding causality. Therefore, we tested several alternative models representing the addition of control variables and different configurations of the variables; none offered a better fit for the data.a Although this strengthens our confidence in the model presented, future work should validate this model with experimental and longitudinal study designs. An additional limitation is the sampling method. Perhaps as a result of recruiting from support groups and online communities, participants were primarily female, White/European-American and fairly wealthy. Further, some highly prevalent chronic illnesses (e.g. heart disease) were under-represented in the current sample. Finally, participants may be particularly high or low in the psychosocial variables measured. For example, they may anticipate greater stigma than other people living with chronic illnesses who do not utilize support groups and online communities. Therefore, the current sample may not represent people living with chronic illnesses in general. This may explain, for example, why anticipated stigma from healthcare providers was not associated with stress. Participants in this sample who anticipate stigma from healthcare workers may be able to afford to switch doctors. Future work should examine the relationships between these variables among more diverse samples of participants recruited from different settings, including clinic lists.
Implications of this Work
By exploring the process by which anticipated stigma relates to quality of life, this study highlights potential points of intervention to improve the well-being of people living with chronic illnesses. Among these, it may be particularly important to reduce stress associated with anticipated stigma. Results suggest that stress was associated with two out of three sources of anticipated stigma, and that stress had the strongest relationship with quality of life. Stress interventions with proven efficacy, such as cognitive behavioural stress management, 11,30,31 may prove especially helpful for people living with chronic illnesses who anticipate a great deal of stigma from friends and family and work colleagues. Such interventions may be adapted to address stress associated with anticipated stigma. Similarly, interventions that target increasing social support and patient satisfaction among people living with chronic illnesses may benefit those who anticipate stigma.
Further, the current study highlights the importance of taking sources of stigma into account. People living with chronic illnesses may anticipate different amounts of stigma from different sources, and the consequences of anticipated stigma may differ depending on the source. Both clinicians and interventionists should differentiate between sources of stigma when addressing anticipated stigma among people living with chronic illnesses. Additionally, research that differentiates between sources of stigma may provide stronger understandings of the stigma that people living with chronic illnesses anticipate, how this stigma impacts them, and how interventions can best address stigma and improve their well-being. Research that continues to attempt to understand and disrupt the relationship between chronic illness stigma and negative health outcomes among people living with chronic illnesses has the potential to improve the health of a substantial number of individuals.
Acknowledgments
Funding
The project described was supported by Award Numbers T32MH074387 and T32MH020031 from the National Institute of Mental Health.
Footnotes
First, a path analysis was performed including the controls of proportion of life with illness, illness affects life, and general health as exogenous variables. Controlling for these variables, all paths included in the original model remained statistically significant. However, the model did not represent a good fit for the data, χ2 (20)=102.52, p<0.001; RMSEA=.16 (CI=0.13–0.19); CFI=0.84. This model may represent a worse fit for the data because the addition of the control variables places extra constraints on the model (i.e. variables and paths) that reduces the power available to attain fit.24 Despite the lack of fit, the fact that the paths remain statistically significant suggests that the control variables pertaining to health and illness do not explain the relationships between anticipated stigma, the mediating variables, and quality of life. Second, a path analysis was performed to evaluate the alternative hypothesis that the process works in reverse. That is, quality of life impacts stress, social support, and patient satisfaction, which in turn impact anticipated stigma from friends and family, work colleagues and healthcare workers. To evaluate this model, the paths within the original model were reversed. This alternative model did not represent a good fit for the data, χ2 (11)=73.32, p<0.001; RMSEA=0.18 (CI=0.14–0.22); CFI=0.84, suggesting that the directionality represented in the hypothesized model is correct.
Reprints and permissions: sagepub.co.uk/journalsPermissions.nav
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
References
- 1.Goffman E. Stigma: notes on the management of spoiled identity. 1. New York: Simon & Schuster; 1986. [Google Scholar]
- 2.Chapple A. Stigma, shame, and blame experienced by patients with lung cancer: qualitative study. BMJ. 2004;328:1470–1474. doi: 10.1136/bmj.38111.639734.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.West M, Dye A, Mcmahon B. Epilepsy and workplace discrimination: population characteristics and trends. Epilepsy Beh. 2006;9:101–105. doi: 10.1016/j.yebeh.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 4.Sayles JN, Ryan GW, Silver JS, Sarkisian CA, Cunningham WE. Experiences of social stigma and implications for healthcare among a diverse population of HIV positive adults. J Urban Health. 2007;84:814–828. doi: 10.1007/s11524-007-9220-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13:1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quinn DM, Chaudoir SR. Living with a concealable stigmatized identity: the impact of anticipated stigma, centrality, salience, and cultural stigma on psychological distress and health. J Pers Soc Psychol. 2009;97:634–651. doi: 10.1037/a0015815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24:518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 8.Sayles JN, Hays RD, Sarkisian CA, Mahajan AP, Spritzer KL, Cunningham WE. Development and psychometric assessment of a multidimensional measure of internalized HIV stigma in a sample of HIV-positive adults. AIDS Behav. 2008;12:748–758. doi: 10.1007/s10461-008-9375-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Visser MJ, Kershaw T, Makin JD, Forsyth BWC. Development of parallel scales to measure HIV-related stigma. AIDS Behav. 2008;12:759–771. doi: 10.1007/s10461-008-9363-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Earnshaw VA, Quinn DM. The impact of stigma in healthcare on people living with chronic illnesses. [accessed 1 October 2011];J Health Psychol. 2011 :1–12. doi: 10.1177/1359105311414952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lazarus RS, DeLongis A, Folkman S, Gruen R. Stress and adaptational outcomes: the problem of confounded measures. Am Psychol. 1985;40:770–779. [PubMed] [Google Scholar]
- 12.Antoni MH, Cruess S, Cruess DG, Kumar M, Lutgendorf S, Ironson G, et al. Cognitive-behavioral stress management reduces distress and 24-hour urinary free cortisol output among symptomatic HIV-infected gay men. Ann Behav Med. 2000;22:29–37. doi: 10.1007/BF02895165. [DOI] [PubMed] [Google Scholar]
- 13.Ironson G. Psychosocial factors predict CD4 and viral load change in men and women with human immunodeficiency virus in the era of highly active antiretroviral treatment. Psychosom Med. 2005;67:1013–1021. doi: 10.1097/01.psy.0000188569.58998.c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spirito A, Ruggiero L, Bowen A, McGarvey S, Bond A, Coustan D. Stress, coping, and social support as mediators of the emotional status of women with gestational diabetes. Psych Health. 1991;5:111–120. [Google Scholar]
- 15.Wallston BS, Alagna SW, DeVellis BM, DeVellis RF. Social support and physical health. Health Psychol. 1983;2:367–391. [Google Scholar]
- 16.Hatzenbuehler ML, Nolen-Hoeksema S, Dovidio J. How does stigma “get under the skin”? : the mediating role of emotion regulation. Psychol Science. 2009;20:1282–1289. doi: 10.1111/j.1467-9280.2009.02441.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holahan CJ, Moos RH. Social support and psychological distress: a longitudinal analysis. J Abnorm Psychol. 1981;90:365–370. doi: 10.1037//0021-843x.90.4.365. [DOI] [PubMed] [Google Scholar]
- 18.Mohr DC, Classen C, Barrera M. The relationship between social support, depression and treatment for depression in people with multiple sclerosis. Psychol Med. 2004;34:533–541. doi: 10.1017/s0033291703001235. [DOI] [PubMed] [Google Scholar]
- 19.Sacco WP, Yanover T. Diabetes and depression: the role of social support and medical symptoms. J Behav Med. 2006;29:523–531. doi: 10.1007/s10865-006-9072-5. [DOI] [PubMed] [Google Scholar]
- 20.Symister P, Friend R. The influence of social support and problematic support on optimism and depression in chronic illness: a prospective study evaluating self-esteem as a mediator. Health Psychol. 2003;22:123–129. doi: 10.1037//0278-6133.22.2.123. [DOI] [PubMed] [Google Scholar]
- 21.Heszen-Klemens I, Lapińska E. Doctor-patient interaction, patients’ health behavior and effects of treatment. Soc Sci Med. 1984;19:9–18. doi: 10.1016/0277-9536(84)90132-1. [DOI] [PubMed] [Google Scholar]
- 22.Earnshaw VA, Quinn DM. Development and evaluation of the chronic illness anticipated stigma scale. The Annual Convention of the Association for Psychological Science; Boston, MA. 2010. [Google Scholar]
- 23.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 24.Zimet G, Dahlem N, Zimet S, Farley G. The multidimensional scale of perceived social support. J Pers Ass. 1988;52:30–41. [Google Scholar]
- 25.Bidaut-Russell M, Gabriel SE, Scott CG, Zinsmeister AR, Luthra HS, Yawn B. Determinants of patient satisfaction in chronic illness. Arthritis Rheum. 2002;47:494–500. doi: 10.1002/art.10667. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. WHOQOL User Manual. Geneva: Switzerland: 1998. Programme on Mental Health. [Google Scholar]
- 27.Kline R. Principles and practice of structural equation modeling. 3. New York: Guilford Press; 2011. [Google Scholar]
- 28.Fife BL, Wright ER. The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancer. J Health Soc Behav. 2000;41:50–67. [PubMed] [Google Scholar]
- 29.Stutterheim SE, Pryor JB, Bos AER, Hoogendijk R, Muris P, Schaalma HP. HIV-related stigma and psychological distress: the harmful effects of specific stigma manifestations in various social settings. AIDS. 2009;23:2353–2357. doi: 10.1097/QAD.0b013e3283320dce. [DOI] [PubMed] [Google Scholar]
- 30.Henry JL, Wilson PH, Bruce DG, Chisholm DJ, Rawling PJ. Cognitive-behavioural stress management for patients with non-insulin dependent diabetes mellitus. Psychol Health Med. 1997;2:109–118. [Google Scholar]
- 31.Penedo FJ, Traeger L, Dahn J, Molton I, Gonzalez JS, Schneiderman N, et al. Cognitive behavioral stress management intervention improves quality of life in Spanish monolingual hispanic men treated for localized prostate cancer: results of a randomized controlled trial. Int J Behav Med. 2007;14:164–172. doi: 10.1007/BF03000188. [DOI] [PubMed] [Google Scholar]