Abstract
Background
There are problems of quality in maternity services at primary health care level in South Africa. Many of these problems can be traced to non-adherence to the maternity care guidelines and lack of tools to support clinic staff and managers in their roles. Objective: The aim of this research was to investigate the utility of e-health (computerized) decision support systems at addressing the problem of compliance of health workers to the maternity care guidelines at primary health care in South Africa. At present there are no documented studies on e-health clinical decision support systems for primary health care in South Africa, though clinical decision support systems for primary health care are listed as part of the e-health strategy of the National Department of Health. Methods: An e-health decision support system named the Bacis (Basic Antenatal Care Information System) Program was developed, then implemented and evaluated at a primary health care clinic. The duration of the study was two years: this includes development, implementation and evaluation.
Results and Conclusion
There was an overall improvement in compliance from 85.1 % to 89.3%. This result was not statistically significant. However when results were stratified into specific categories, the Bacis Program showed statistically significant improvement in compliance over the checklist system in three out of nine important categories. These are compliance at booking, patients younger than 18 years and patients booking after week 20. Further, insights and experience were also gained on development and implementation of clinical information systems at resource strained environments such as primary health care in South Africa. These results, insights and experience are invaluable for the implementation of the proposed e-health strategy in South Africa.
Keywords: Clinical decision support systems, maternal health care, guideline adherence, primary health care
1. Introduction
There are problems of quality in maternity services at primary health care in South Africa [1, 2]. Many of these problems can be traced to non-adherence to the maternity care guidelines and lack of tools to support clinic managers and staff in their roles at the clinics [3]. The Guidelines for Maternity Care in South Africa and the BANC (Basic Antenatal Care Checklist) checklist are the main guidelines for the nurses at primary health care clinics in South Africa [4, 5]. The Bacis (Basic Antenatal Care Information System) Program, which is the computerized decision support system reported in this paper, was created to address problems of compliance with these guidelines.
The reasons for selecting a computerized decision support system to address the problems of compliance to guidelines and quality of maternity services are the following: Firstly in other countries, studies have shown that computerized decision support systems can be used successfully to improve compliance to clinical practice guidelines [6, 7, 8]. Secondly, currently primary health care facilities in South Africa do not have detailed electronic information to routinely use for decision making, and the paper-based systems do not meet the needs and requirements of the health system in the country [9]. The one computerized information system in routine use at primary health care level in South Africa is the District Health Information System (DHIS), which is an administrative and management information system that collects aggregate data on patient encounters and is intended for use by managers higher up in the health system [10]. For example, the District Health Information Systems has only three items on maternity care: though it may be adequate for higher level managers at the district and provincial level, it offers little information for decision-making at the primary health care level.
Further, an e-health architecture and strategy is under development in South Africa by the National Department of Health [9]. The National Department of Health considers e-health vital to the implementation of the National Health Insurance (NHI) which is a key project intended to overhaul and improve health care delivery in South Africa [11]. The e-health strategy makes provision for information systems support and clinical decision support at primary health care level in South Africa. However, at present there are no e-health decision support systems initiatives at primary health care level that have been documented in South Africa. The Bacis Program study, addresses this gap.
The main objectives of the study were the following: (i) To examine the extent to which a computerised, protocol-based, decision-support system can be used to improve compliance of primary health care staff in the use of the maternity care protocols and the BANC checklist; (ii) to investigate the reasons for non-compliance to maternity care protocols at primary health care clinics in South Africa (this objective is however not reported in this paper but is reported elsewhere [3]); (iii) to conduct a usability review of the Bacis Program and to gain insights on its acceptability as a decision aid for nurses; (iv) to use the electronic record feature of the Bacis Program to report on patient outcomes (this objective is also not reported in this paper but is reported elsewhere [3]); (iii) and finally to assess the broader utility of the computerised, protocol-based, decision-support system in quality assurance at the clinic level in South Africa.
2. Materials and Methods
The study methodology was divided into two phases. Phase one was on the development of the Bacis Program, and documenting this development experience. Phase two involved the field testing of the Bacis Program with the aim of measuring the extent to which it could be used for improving compliance of nurses at primary health care to the maternal health protocols.
2.1 Phase I Development of the Bacis Program
The Bacis Program is an e-Health clinical information system. It was developed at the South African Medical Research Council by the researcher (V. Horner), with the assistance of medical experts. It was conceptualised by the researcher (V. Horner, abbreviated as VH) and the study obstetrician (TJ.
Mashamba, abbreviated as TJM) as a tool that could be used at primary health care clinics to improve compliance to maternal health protocols and the BANC checklist.
The researcher (VH) played the role of the knowledge engineer and software developer, and the study obstetrician (TJM) acted as the domain expert. A project implementation team was formed which consisted of the researcher (VH); the study obstetrician (TJM) who is the chief consultant on obstetrics and gynaecology at the tertiary hospital in the district; the manager for maternal and child health in the district; the sub-district manager on maternal and child health; and the chief director of the Department of Health in Tshwane Health District.
The implementation team was composed so as to involve the main stakeholders in order that permissions for implementing the Bacis Program at the clinics and permissions for data collection would be expedited.
It was possible to bring these people together because improving dissemination and compliance with the maternity care guidelines is one of the major goals of the Department of Health in South Africa. The project utilised a budget of 160000 USD, which was sourced from the National Research Foundation (NRF) of South Africa. The main items in the budget were the purchase of six computers and scanners for use at the antenatal care sections of three clinics that had initially been selected as study sites; software licenses for Microsoft Office and Microsoft Access which are needed for the Bacis Program; the salary for the researcher (VH) and an assistant; and finally project operational costs such as travel expenses and project stationery. The Bacis Program was initially deployed at three clinics in Tshwane Health District though data from one clinic only is reported in the study due to administrative problems that occurred at the other two clinics during the course of the study. The problems experienced by the two clinics are elaborated on further in Section 2.2.4 under study sample and participants.
The Bacis Program uses patient specific information entered during an antenatal visit in order to perform: risk classification, identification of patients for referral and scheduling of maternity care interventions. To perform these tasks the Bacis Program uses its rule base and knowledge base that have been developed in collaboration with medical experts. However, the final decision is taken by the nursing sister. The Bacis Program is only intended as an aid in the decision making process i.e. it is a decision-support system. ►Figure 1 and ►Figure 2 are screenshots of the user interface of the Bacis Program, which show some of its risk assessment items. The extended list of features of the Bacis Program is the following:
Fig. 1.
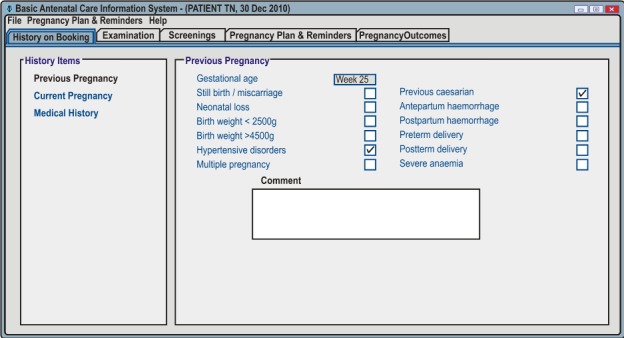
Screenshot of patient history menu
Fig. 2.
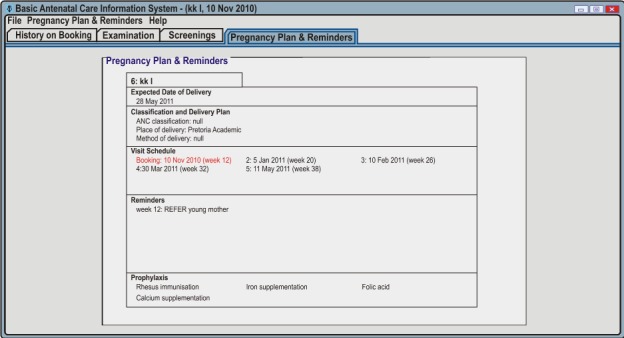
Screenshot of pregnancy plan and reminders menu
-
•
referral criteria and a rule base of antenatal and maternal health care protocols;
-
•
a date function for calculation of expected date of delivery and visit schedule;
-
•
reminders and popup alerts for abnormal screening values;
-
•
system created reminders and user defined reminders;
-
•
data entry and data validation prompts as wells as data completeness checks;
-
•
an electronic antenatal care record consisting of all the fields contained in the antenatal card of the Department of Health which is implemented in Microsoft Access.
As noted in the last point of the features, the Bacis Program also acts as an electronic antenatal record in addition to its clinical decision-support system function. Therefore the Bacis Program is much more comprehensive as a maternity system, having many more features than the District Health Information System, and it satisfies many of the points in the e-health strategy of the National Department of Health for clinical decision support at primary health care [9].
2.2 Phase II Field Evaluation
2.2.1 Research Design: Field Evaluation
The aim of the field evaluation of the Bacis Program was to measure improvements in nurse compliance with the maternity care guidelines as well as a usability review and acceptability of the Bacis Program as a decision aid for nurses at primary health care.
A before and after design consisting of two cohorts at the study clinic was employed in order to compare and measure improvements in compliance. The retrospective cohort (before wing) consisted of patients who were treated before introduction of the Bacis Program. The prospective cohort (after wing) consisted of patients who were treated after introduction of the Bacis Program. The method of assessing compliance was a record review.
The review measured compliance to the guidelines for eighteen (18) antenatal protocol items corresponding to the main tasks that nurses are expected to carry out at the clinics [4, 5]. These are: Previous pregnancy history; Current pregnancy history; General medical history; General examination; SFH (symphysis fundal height); Fetal heart rate; Fetal lie and presentations; Severe symptoms (these are: severe headache, abdominal pain or discomfort, reduced fetal movement, abdominal bleeding and liquor drainage); Pregnancy infections; Blood pressure; Proteinuria; Maternal weight and height; Rh (rhesus blood group) screening; Syphilis screening (this is also called RPR screening – Rapid Plasma Reagin test); Haemoglobin screening; HIV screening and implementation of Prevention of Mother To Child Transmission of HIV – which is abbreviated as PMTCT; Glycosuria; and Prophylaxis (these are calcium, iron and folic acid).
A professional nurse from the study clinic was enlisted as the study nurse. She used the Bacis Program to conduct antenatal patient visits.
A qualitative component was also introduced in order to document the reasons for non-compliance with the maternity care guidelines at the study clinics. However, the results of the qualitative interviews on reasons for non-compliance are reported elsewhere [3].
2.2.2 Methods Measuring Compliance
Compliance was measured as a combination of completion and response. Completion the first part of compliance checked whether the protocol item (i.e. antenatal care task) was carried out when due. Response checked whether the medical response to risk factors or abnormal values was adequate. This is sometimes called interpretation and decision making [5, 12]. For example a check was done whether a value for haemoglobin was entered at the first visit (at booking). If yes, then a tick for completion, otherwise it was marked as not completed. There is however the possibility that an item may have been done, but not recorded in the patient card. But based on review of the cards there was no way of ascertaining this. Hence missing information was scored as not completed. For response: if for example the value recorded in the card for haemoglobin was 6 g/dL, then the nurse was expected to refer this patient, otherwise the response was marked as inadequate by the reviewer. Information for the response was also taken from the cards, and missing information was also judged as response not adequate. For compliance to be satisfied the item had be completed (recorded in the patient card), and the response to any abnormal values had to be adequate.
The response adequacy is computed as the number of times that the response was adequate divided by the number of risk factors identified in the review. Similarly the percentage for completion is the number of times the item was actually carried out, divided by the number of times it was due.
2.2.3 Methods Usability Review
The Bacis Program was also subjected to a usability evaluation in order to examine how the nurses interacted with it and whether they found it to be an acceptable aid. The method for evaluating usability was to measure data input accuracy of the study nurses and to carry out qualitative interviews with them in order to understand whether they considered the Bacis Program an acceptable aid. The themes covered by the usability interviews are the following: Relevance of the clinical content of the Bacis Program. This theme required the nurses to compare the content and process of the Bacis Program with actual practice; The usability and cognitive aspects of the Bacis Program, such as, the time needed to learn the Bacis Program as well as the time taken to complete the tasks of the Bacis Program; The last theme was usefulness of the reminders and alerts of the Bacis Program as well as the method used for issuing them.
Finally, as part of the field evaluation, the antenatal record feature of the Bacis Program was used to report on patient outcomes. These patient outcomes are however also reported elsewhere [3].
2.2.4 Study Setting, Sample Size and Participants
The study clinic is located in a semi-rural township about 45 kilometers from the Pretoria central business district. The population of the township is estimated at about 80000. The township consists of formal dwellings as well as shacks, with many backroom dwellings. It has high unemployment (40%) and HIV prevalence (22%) [13]. Its profile fits that of a typical underserved area in South Africa, with a high burden of health issues. The characteristics of the study clinic are shown in ►Table 1. The Bacis Program was created with the goal of helping to improve health care services in under-serviced areas such as Winterveldt.
Table 1.
Characteristics of the study clinic.
| Characteristic | Value |
|---|---|
| 1. General Monthly Patient Load: (Primary Health Care, Chronic Diseases, Child Health and Maternity Care) |
13 000 patients per month |
| 2. Antenatal Care: average number of new bookings per month |
210 patients |
| 3. Average number of referrals in labour per month (ODI and DGMH) |
78 patients |
| 4. Average number of deliveries per month | 104 patients |
| 5. Staffing: advanced midwives at clinic |
1 nurse |
| 6. Staffing: professional nurses with midwifery |
36 nurses |
| 7. Estimated unemployment levels in Winterveldt | 40%* |
| 8. Estimated average household income per month in Winterveldt | R500* |
*Taken from: Profile of the North West Province: demographics, poverty, income, inequality and unemployment [13]
Although three clinics were enrolled initially in the study, only the data from Kgabo Community Health Centre in Winterveldt was included in the results. The data from the other two clinics, Temba Community Health Centre and Soshanguve III Community Health Centre was not included. This is because their data was not complete due to administrative problems that occurred during the study. Firstly, at one clinic, two nurses were found initially who used the Bacis Program faithfully. These two nurses managed to enroll 300 patients and captured all their first visits (booking) faithfully. However, they were not able to remain in the study for nine months due to staffing constraints at their clinic and as a result only completed about four months of the total nine months of data collection. The patients enrolled at this clinic were thus not included in the results because they were not tracked for the full duration of their pregnancies. At the second clinic, also due to staffing constraints, a nurse could not be found who could use the Bacis Program. As an alternative, a data capturing clerk was enlisted. The Bacis Program, however, is intended for use by professional nurses. Hence, the results from the second clinic were also not included in the compliance review.
Compliance is reported for 100 patients of the 319 patients in the prospective cohort. ►Table 2 shows the place of delivery of the prospective cohort including the 100 patients reviewed for compliance. The 100 patients in the compliance review are those whose antenatal cards could be found and who delivered at the clinic between January 2011 and June 2011. As the women delivered their babies, the researcher, assisted by the study nurses, made copies of study patient files. Of the 144 patients who delivered at the clinic, cards could only be found for 100 of them. The 25 patients in the before wing (retrospective cohort) were chosen for logistic reasons of doing a thorough review. For example the time taken to review a card by the researcher was about three hours, this includes creating an entry in the data collections system and entering the review data for the patient. The effort expanded in the review was similar to doing a case study. The researcher often had to do multiple rounds of review of the cards when discrepancies in the criteria were picked up and needed correction. Hence fine tuning of review criteria also consumed much time. The review effort also applied to the 100 patients of the prospective cohort. As described in the results section statistical calculations were however possible with these sample sizes.
Table 2.
Delivery information of the prospective cohort (n = 319 patients)
| Place of Delivery | % |
|---|---|
| 1. Delivered at clinic | 45.1% (144) |
| 2. Delivered at home | 3.4% (11) |
| 3. Delivered at referral hospitals (*Odi or **DGMH) |
41.1% (131) |
| 4. Delivery information not found at clinic or referral hospitals (ODI and DGMH) |
10.3% (33) |
* Odi Hospital
** Dr. George Mkhari Hospital
The duration of the field evaluation was nine months: patient enrolment was four months, and the remaining five months were used to track follow up antenatal visits and patient deliveries. All patients reporting their pregnancies during the study were enrolled in the prospective cohort. The retrospective cohort was selected from 115 cards that were available of women who delivered between November and December of 2010 before the Bacis Program was introduced at the study clinic. The clinics only keep patient cards for six weeks post delivery, hence there are never more than 160 cards of patients post delivery at the clinics. From an unordered collection of files for November and December 2012, and after shuffling them, the researcher selected the first twenty five files. For data analysis basic descriptive statistics were used.
3. Results
3.1 Study Setting and Sample Size
The results for compliance are for a community health center in Tshwane Health District. Though initially three clinics were enrolled in the study, the results of only one clinic are reported due to logistics problems that have been elaborated in the methods section above. A total of 25 patients were enrolled in the retrospective review and 100 in the prospective review. The duration of data collection in the field evaluation was nine months.
3.2 Results: Compliance Review
The results of compliance for the 18 antenatal protocols are shown in ►Table 3. Although 18 protocol items were considered in the review, severe symptoms and pregnancy infections were not included in the results column for ‘completion’ because there are no fields for them in the antenatal cards. This made it difficult to determine whether they were done (completed) or not done based on the record review only.
Table 3.
Results of compliance overall for the 18 antenatal protocol items
| Item | Completion (%) | Response Adequate (%) | Compliance (%) | |||
|---|---|---|---|---|---|---|
| Before | After | Before | After | Before | After | |
| 1. previous pregnancy history | 100.0 | 99.0 | 0.0 | 30.1 | 84.0 | 90.0 |
| 2. current pregnancy history | 96.0 | 100.0 | 100.0 | 0.0 | 96.0 | 95.0 |
| 3. general medical history | 100.0 | 99.0 | 100.0 | 100.0 | 100.0 | 99.0 |
| 4. general examination | 67.4 | 85.4 | 50.0 | 25.0 | 67.4 | 83.4 |
| 5. SFH | 87.0 | 93.4 | * | * | 87.0 | 93.4 |
| 6. Foetal heart rate, gestational age >28 weeks | 100.0 | 92.1 | * | * | 100.0 | 92.1 |
| 7. Foetal lie and presentation, gestational age >34 weeks | 87.0 | 86.1 | * | * | 87.0 | 86.1 |
| 8. Severe symptoms | * | * | 66.6 | 100.0 | 97.8 | 100.0 |
| 9. Pregnancy infections | * | * | 66.6 | 74.0 | 95.7 | 95.4 |
| 10. Blood pressure | 100.0 | 100.0 | 0.0 | 25.0 | 95.7 | 98.0 |
| 11. Proteinuria | 95.7 | 100.0 | * | * | 95.7 | 100.0 |
| 12. Maternal weight and height | 58.7 | 94.0 | * | * | 58.7 | 94.0 |
| 13. Rh | 88.0 | 84.0 | 0.0 | 0.0 | 84.0 | 82.0 |
| 14. RPR | 84.0 | 84.0 | 100.0 | 100.0 | 84.0 | 84.0 |
| 15. HIV | 100.0 | 100.0 | 50.0 | 0.0 | 92.0 | 89.0 |
| 16. Haemoglobin | 84.0 | 84.0 | 100.0 | 50.0 | 84.0 | 83.0 |
| 17. Glycosuria | 93.5 | 98.0 | * | * | 93.5 | 98.0 |
| 18. Prophylaxis | 30.4 | 45.0 | * | * | 30.4 | 45.0 |
| Mean values | 85.7 | 90.3 | 57.6 | 45.8 | 85.1 | 89.3 |
* This means that the item was not included in the column measure. The reasons for this are explained in the body text in Section 3.2
Further for the ‘response’ column only those items where serious issues arose in the study were included. Proteinuria, and maternal weight and height both had minor issues arising in the study and were therefore not included for ‘response’. Foetal heart rate, foetal lie and presentation, and glycosuria had no issues arising in the study and were therefore not included for ‘response’. Prophylaxis was only considered under completion; it is not a risk factor.
Though protocols exist for assessing the response to SFH, they could not be consistently applied in the record review because of missing information and some inconsistencies that were identified. Hence, of the eighteen (18) protocol items, only eleven (11) were evaluated for response.
In view of the samples sizes for the two groups, the T-test statistic was used to test for significant differences between the before and after wings of the compliance review at the 5% (α = 0.05) level of significance. In terms of overall compliance there was an improvement from 85.1 % to 89.3% in the compliance of nurses when using the Bacis Program (p-value = 0.14 at 95% confidence). This result was not statistically significant, but when results were stratified into specific antenatal categories, the compliance of the nurses using the Bacis Program showed statistically significant improvement over the paper-based checklist system in three categories out of nine: compliance at booking (p-value = 0.016 at 95% confidence), patients younger than 18 years (p-value = 0.0023 at 95% confidence) and patients booking after week 20 (p-value = 0.040 at 95% confidence). ►Table 4 shows the results of compliance for the nine categories as well as their p-values.
Table 4.
Compliance by maternal and antenatal patient category
| Item | Before Intervention (%) |
After Intervention (%) |
P-values at 95% confidence |
|---|---|---|---|
| 1. Compliance overall | 85.1 | 89.3 | 0.14 |
| 2. Compliance at booking (1st visit) | 82.7 | 90.2 | 0.016 ** |
| 3. Compliance at follow up visits | 87.4 | 86.6 | 0.87 |
| 4. Compliance for patients booking before week 20 | 89.9 | 89.7 | 0.96 |
| 5. Compliance for patients booking after week 20 | 82.8 | 89.2 | 0.040 ** |
| 6. Compliance for patients younger than 18 years | 78.7 | 92.0 | 0.0023 ** |
| 7. Compliance for patient older than 18 years | 85.6 | 89.0 | 0.27 |
| 8. Compliance for primigravida patients | 87.3 | 91.9 | 0.18 |
| 9. Compliance for multi-gravida patients | 83.7 | 88.1 | 0.16 |
** The double star indicates that result is statistically significant.
3.3 Results: Usability Review
The first measure in the usability review of the Bacis Program was the overall data input error rate of the study nurses, which was at 13.2%. This was better than the error rate of 25% for the District Health Information System [10]. With regards to acceptability of the Bacis Program as a decision aid for nurses, the results of the interviews of study nurses were optimistic. Even though older nurses tended to be poor in computer literacy, the younger nurses entering the system are computer literate and the Bacis Program will find a welcome audience with them. Some additional uses of the Bacis Program were also identified by the nurses, such as use of its electronic record feature in surveys on maternity care which have to be carried out at the clinics from time to time.
4. Discussion and Conclusion
The sample sizes were small. As elaborated in the methods section this was due to the time required to carry out the review, as well as time spent in refinement of review criteria. With review criteria having been established in this study, future research using these criteria should have a better method of estimating sample size and be able to work faster. In the compliance review proteinuria, maternal weight and height, foetal heart rate, foetal lie and presentation, and glycosuria all had minor issues or no issues arising in the study and were therefore not included for ‘response’. Including these items with minor issues or no issues in the study would have inflated the response. In general these items do have serious issues, however serious issues were not found for them among the study sample.
However there were problems of completion for many of them indicating quality problems. Perhaps a study needs to be done which uses a convenience sample in order to find patients that have serious issues for these items in order to judge response for them. For these five items a random sample yields few or no patients with serious issues. Although protocols exist for assessing response to SFH, they could not be applied consistently in the record review because of missing information and some inconsistencies that were identified. Hence the criteria for assessing response for SFH need to be refined by the guideline authors so that it can be consistently applied in a record review. However, the rate of completion for SFH is a useful start in assessing compliance for SFH. In fact there were problems in completion of SFH, pointing to quality problems. These problems on response to SFH are discussed in the qualitative review for compliance which is reported elsewhere [3].
Though overall the results for compliance were not statistically significant, when compliance was stratified into various antenatal care categories the results were significant for three categories out of nine (refer to Table 4). The nine categories that were used are all important in maternal and antenatal care. For example booking is considered the most important antenatal visit as the patient history is taken here and most screenings are also done at booking. Booking refers to the first antenatal visit of a pregnancy. The category of patients younger than 18 years measures how well the nurses had treated young antenatal patients. Young mothers (pregnant women younger than 18 years) are many in South Africa. Ideally women younger than eighteen years should be at school. It is important to consider young mothers because they have some subsets of protocols dedicated to them and they are also considered high risk pregnancies. The third category of women booking after gestation week 20 is for women who have their first visit (booking) after week 20. The BANC checklist recommends that women should begin antenatal care at gestation week 12. In fact in South Africa most women begin antenatal care after week 24 (six months) which is considered late [5]. Since the performance of the Bacis Program was statistically significant for three antenatal categories out of nine, including the most important category of booking, it can be concluded that the Bacis Program performed well.
In the compliance review there were no statistically significant improvements in response. In fact it dropped, though this was also not statistically significant. Even though it is harder to improve response than completion [12], an improvement in response had been expected. This is a gap for future study. It was also not possible to distinguish between improvements in actual care and improvements in recording of information. In other words it may be the case that some tasks are carried out by the nurses and their response to issues is adequate but this information is poorly recorded. Distinguishing between poor recording on the one hand and omissions in care on the other hand, is another gap for a future study.
The Bacis Program has further benefits in that it can assist with research at clinic level as well as be used for the compilation of clinic statistics for inclusion in reports and to carry out medical audit. These results have thus also contributed to the topic of the content and quality of antenatal care at primary health care level in South Africa, which was one of the goals of the study. This was an important goal because most studies on maternity care in South Africa, report on attendance of antenatal care by women, but none report on the detailed care activities that are carried out for antenatal patients. For example they may report that 94% of women attend antenatal care, but few report on how well haemoglobin screening is done or compliance with the PMTCT (Prevention of Mother to Child Transmission of HIV) protocols. The Bacis Program study was able to report on the detailed activities carried out at antenatal care by showing compliance for 18 antenatal items, which include HIV and PMTCT.
With regards to usability the results were optimistic. The Bacis Program was found to have a better data input error rate than the District Health Information System. However the data input errors need to be categorised between serious, intermediate and minor. This is because even if the data input error rate is low, if it affects crucial or serious instances then this is a big problem. From the qualitative interviews the study nurses also reported that the Bacis Program is an acceptable tool to them. One of the strengths of the Bacis Program is that its data is intended for use by the nurses rather than for reporting to higher levels in the health system hierarchy. This problem can be explained as follows: For example the data gathered at the clinics by the District Health Information System, which is an administrative computer system currently in routine use at clinics in South Africa, is aggregate data meant for managers at the district level. Nurses on the other hand need data on specific patients in carrying out their duties. It is hoped that since the data of the Bacis Program is meant for the nurses at the clinics rather than managers higher up in the hierarchy, this will motivate the nurses to use it.
When used faithfully, no major safety problems are expected as the Bacis Program uses the BANC checklist process and the maternity care guidelines which are relatively safe. The rate of inappropriate referrals due to false positive diagnoses is also not expected to be high because the Bacis Program uses the BANC checklist process and the national maternity care guidelines. However this assumption needs qualification because, in the study, a number of guideline recommendations have been highlighted for review because they resulted in a high number of referrals judged to be inappropriate by the hospitals to which the patients were referred [3].
There are however resource implications to implementation of the Bacis Program. Firstly, training of nurses in its utilisation will be a challenge, as this will involve many nurses, and the training requires a substantial commitment in time from the participating nurses. Time is a big problem at the clinics in South Africa. Secondly integration of the Bacis Program with the clinics’ workflow also needs further attention. Currently patient held paper records have to be completed, which are used for the duration of a woman's pregnancy. The patient-held paper records are important because there is no electronic record system in South Africa. In this scenario the Bacis Program becomes an extra item in the duties of the nurses. This may explain the difficulty in finding a nurse at one of the clinics and in retaining the two study nurses in the second one. However the benefits of using the Bacis Program can outweigh the extra effort that is needed for it. Thus integration of the Bacis Program into the clinics’ workflow is another gap in the study which needs to be explored. Thirdly implementation of the Bacis Program depends on availability of computers at the clinics. Currently this is not the case in South Africa. However the e-Health Strategy of the Department of Health [9] makes provisions for computers and software such as Microsoft Access. At present though, most clinic managers have computers; either desktops or laptops. So perhaps in the beginning the Bacis Program can be used as an audit tool by clinic managers, then be phased in for the general nursing staff as computers are introduced generally at the clinics.
One last point here in the discussion pertains to the use of patient cards in the compliance review for the prospective wing rather than data in the Bacis Program. The patient cards were used for the review because the current standard of care in South Africa requires that the paper cards be completed, and that the pregnant women carry this card with them. If a system is supposed to bring improvements, it must also bring improvements on how patient cards are completed, and of course must also improve actual care. The data input error rate of 13% recorded for the Bacis Program in the usability review in fact measured the discrepancy between information in the patient cards and information in the Bacis Program. In this review sometimes information was: (1) present in the patient cards but not in the system, or (2) sometimes present on the system but not in the cards, and (3) values recorded in the cards and on the system were sometimes different. Whether the system or the patient cards record information better needs to be investigated further. In the current study the cards were assumed to hold better information as they are the current standard used by the health system.
The results of this first study on the Bacis Program have been optimistic, and as such have paved the way for future studies on the Bacis Program which should employ larger samples as well as review its other aspects that were not covered by this first study.
Clinical Relevance
The aim of this research was to investigate the utility of e-health (computerized) decision support systems at addressing problems of compliance of health workers to the maternity care guidelines at primary health care in South Africa. Maternity services are one of the priority areas in South Africa.
Conflict of Interest
The authors declare that they have no conflict of interest in the research.
Protection of Human and Animal Subjects
The study was health services research measuring improvements in compliance to practice guidelines after implementation of a computerized decision support system at a primary health care clinic. Ethics approval for the study was obtained from the University of Limpopo Medunsa Research Ethics Committee. Consent was obtained from the nurses and patients to participate in the study and consent forms were also signed by them. The study was performed in compliance with the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects.
Acknowledgements
The authors would like to acknowledge and thank the National Research Foundation, South Africa, and the Research Capacity Development division of the South African Medical Research Council for sponsoring the project.
References
- 1.Pattinson RC. Chapter 7: Maternal Health [report, health systems research agency]. In: South African Health Review 2003/2004. Durban(South Africa): Health Systems Trust, South Africa; 2004; p. 89-99 [Google Scholar]
- 2.Department of Health. Confidential Enquiry into Maternal Deaths 2007 [report on enquiry into maternal deaths] Pretoria (South Africa): Department of Health, South Africa; 2008 [Google Scholar]
- 3.Horner V. The Utilisation of a Decision Support System for Increasing Levels of Compliance of Health Workers to the Maternity Care Protocols and Improving Maternity Outcomes in Gauteng Province South Africa [PhD thesis] Garankua (South Africa): University of Limpopo, Medunsa Medical Campus; Department of Community Health; 2012 [Google Scholar]
- 4.Department of Health. Guidelines for Maternity Care in South Africa [national guidelines on maternity care] third ed. Pretoria(South Africa): Department of Health, South Africa; 2007 [Google Scholar]
- 5.Pattinson RC. Basic Antenatal Care (BANC) Handbook [training manual] Pretoria (South Africa): University of Pretoria, South Africa; 2007 [Google Scholar]
- 6.Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al. Effectiveness and Effeciency of Guideline Dissemination and Implementation Strategies [technical report, performance agency] Health Technology Assessment 2004; 8(6). [DOI] [PubMed] [Google Scholar]
- 7.Zielstorff RD. Online practice guidelines: issues, obstacles, and future prospects. J Am Med Inform Assoc 1998; 5: 227-236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lobach DF, Hammond WE. Computerized decision support based on a clinical practice guideline improves compliance with care standards. Am J Med 1997; 102: 89-98 [DOI] [PubMed] [Google Scholar]
- 9.Department of Health. e-Health Strategy, 2012. – 2016[policy document] Pretoria (South Africa): Department of Health, South Africa; 2012 [Google Scholar]
- 10.Rohde J, Shaw V, Hedberg C, Stoops N, Venter S, Venter K, et al. Chapter 13: Information for Primary Health Care [report, health systems research agency] : South African Health Review 2008. Durban(South Africa): Health Systems Trust, South Africa; 2008 [Google Scholar]
- 11.Department of Health. NHI Policy Document [policy document] Pretoria(South Africa): Department of Health, South Africa; 2011 [Google Scholar]
- 12.Yoong AFE, Lim J, Hudson CN, Chard T. Audit of Compliance with Antenatal Care Protocols. British Medical Journal 1992; 305: 184-186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacobs E, Punt C, Bothloko C. A profile of the North West Province: demographics, poverty, income, inequality and unemployment [technical report; Internet] PROVIDE Project; North West Provincial Government, South Africa; 2009. [cited 2012 June] Available from: http://ideas.repec.org/p/provbp/58056.html [Google Scholar]


