Abstract
Background
Most patients cannot remember their entire medication regimen and occasionally forget to take their medication.
Objectives
The objective of the study was to design, develop, and demonstrate the feasibility of a new type of medication self-management system using smartphones with real-time medication monitoring.
Methods
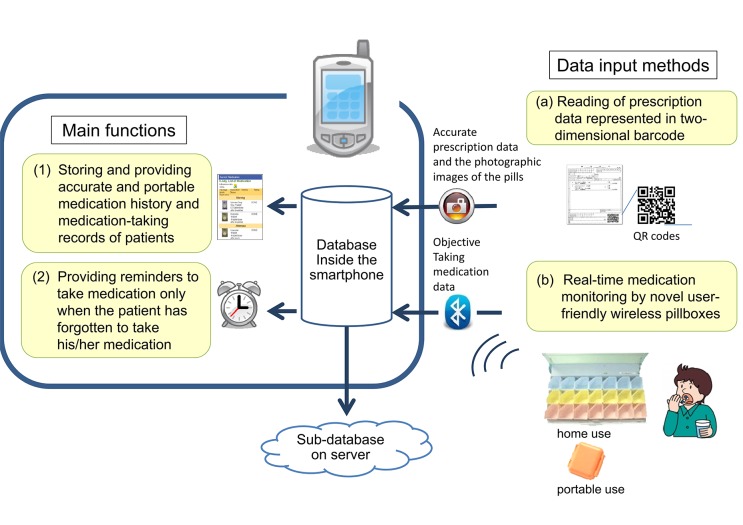
We designed and developed a smartphone-based medication self-management system (SMSS) based on interviews of 116 patients. The system offered patients two main functions by means of smartphones: (1) storage and provision of an accurate, portable medication history and medication-taking records of patients; and (2) provision of a reminder to take medication only when the patient has forgotten to take his/her medication. These functions were realized by two data input methods: (a) reading of prescription data represented in two-dimensional barcodes using the smartphone camera and getting the photographic images of the pills; and (b) real-time medication monitoring by novel user-friendly wireless pillboxes.
Results
Interviews suggested that a pocket-sized pillbox was demanded to support patient’s medication-taking outside the home and pillboxes for home use should be adaptable to the different means of pillbox storage. In accordance with the result, we designed and developed SMSS. Ten patients participated in the feasibility study. In 17 out of 47 cases (36.2%), patients took their medication upon being presented with reminders by the system. Correct medication-taking occurrence was improved using this system.
Conclusions
The SMSS is acceptable to patients and has the advantage of supporting ubiquitous medication self-management using a smartphone. We believe that the proposed system is feasible and provides an innovative solution to encourage medication self-management.
Keywords: Self-management, mobile phone, medication adherence, physiologic monitoring, eHealth systems
1. Background
Most patients do not remember their entire medication regimen and they also occasionally forget to take their medication [1]. Outpatients with chronic diseases, particularly those who have to manage more than one medication or take medication more than once a day, may not take their medications properly. The rate of medication adherence, defined as “the extent to which the patient follows medical instructions”, has been reported to be approximately 50–80% [2-4]. Patient adherence to medication is clinically crucial in reducing mortality of serious disease and total health care costs. Nevertheless, the above-described problems have defied a solution for a long time [5, 6].
The most common patient-related factor resulting in non-adherence include ‘simply forgot’, although medication adherence is a multidimensional phenomenon [2, 3, 7]. The rate of ‘simply forgot’ was 66% in HIV/AIDS clinical trials and 30% in other clinical trials [3, 7]. Recent studies have suggested that prospective memory, which describes one’s ability to remember to do something at a later time, is an important component in medication adherence [8]. Consequently, helping patients remember to take their medication is a simple and effective way to improve adherence.
As information and communication technology (ICT) develops, a system using mobile phones to support medication-taking will become increasingly necessary as a part of the mHealth (mobile health) system [9, 10], because mobile phones are easy for patients to carry even in the event of an emergency or a disaster. Recent studies have shown that reminder-based interventions using a short message service from mobile phones improved medication adherence [11-13]. Not only mHealth systems, but also a number of other types of self-management tools for medication have been published, i.e., reminder packaging, electronic medication monitors, and smartphone software for medication management [11-18]. Their features are shown in ►Table 1 for comparison. Though all are effective to some degree, the authors believe that there is currently no overall, feasible, validated solution for patients to carry their medication history with them, and to receive reminders for taking their medication anywhere.
Table 1.
Tools for medication self-management
| Electronic medication functions | Pillbox | Typical tools | ||||||
|---|---|---|---|---|---|---|---|---|
| Portable Medication history | Remind to take medication | Record of medication-taking | Alert not to take wrong medication | Ubiquity | Portability | Handles many medications | Brand name or category name [reference] | |
| Reminder packing | - | - | - | - | - | Yes/No1 | Yes | pill organizer calendar blister packaging [14, 15] |
| Electronic medication monitors | No | No | Yes | No | No | Yes | Yes/No2 | MEMS (Aardex Ltd.) [16] |
| Second generation of electronic medication monitors | No | Yes3 | Yes | Yes3 | No4 | Yes | Yes | Med-eMonitor (InforMedix, Inc.) [17] Med-Tracker [18] |
| SMS by mobile phones | No | Yes | No | No | Yes5 | - | - | [12, 13] |
| Smartphone software for medication | Yes6 | Yes | Yes/No6 | No | Yes5 | - | - | Pill reminder applications |
1 Only small pill organizers are portable
2 Many bottles are needed to handle many medications
3 By reporting medication-taking records in real-time
4 Some tools can use around one’s house but not use far from the house
5 When mobile internet connection is available;
6 Sometimes inaccurate due to manual entry by patients
2. Objectives
The purpose of this study was to design, develop, and demonstrate the feasibility of a system using a smartphone to support the patient’s self-management of medication. The system aimed to provide patients with an accurate medication history, and give them reminders about medication-taking by means of real-time monitoring of taking the medication.
3. Methods
3.1 Interviews on how patients can manage their own medication
Before designing a system, we interviewed outpatients to determine the current state of medication self-management. We investigated their medication regimens, the number of their medications that they could remember correctly, the frequency of forgetting to take medication, and the means by which they carried or stored their medication in daily life (►Table 2, ►Table 3). We used semi-structured interview to clarify the means referring to the previous medication management instruments [19, 20]. Those interviewed were patients who visited the Department of Cardiovascular Medicine and the Department of Diabetes Metabolic Diseases at the University of Tokyo Hospital from April to June 2010. We interviewed consecutive patients who visited two departments of the hospital during office hours in the survey periods. The hospital is designated as an advanced treatment hospital. Patients who were under 20 years of age were excluded. They gave informed consent to participate in the interview.
Table 2.
Characteristics and medication regimens of patients in the interviews (n = 116)
| Characteristic | Value | |
|---|---|---|
| Age ( years, mean ± SD) | 67.8 ± 12.1 | |
| Male sex | 64.7% | |
| Average number of daily medicines (mean ± SD) | 7.6 ± 4.2 | |
| Department | ||
| Cardiovascular Medicine | 56 | |
| Diabetes and Metabolic Diseases | 60 | |
| Taking medicines everyday | 112 (100%) | |
| once/day | 15 (14%) | |
| twice/day | 27 (24%) | |
| three times/day | 54 (48%) | |
| four times/day | 15 (13%) | |
| five times/day | 1 (1%) | |
| Possession of mobile phones | 88 (75.9%) | |
| over 70 years old | 27 (73.0%) | |
| Use of mobile phone e-mail | 47 (41%) | |
SD standard deviation
Table 3.
Interviews themes and results (n = 112)
| Value | |||
|---|---|---|---|
| The number of their medications that they could remember correctly | |||
| All of their medication | 27 (24.1%) | ||
| A part of their medication | 36 (32.1%) | ||
| None of their medication | 49 (43.8%) | ||
| Forget to take their medication by self-reports | |||
| Forget to take their medication or take their medication more than two hours behind the schedule more than once a week | 46 (41.1%) | ||
| How to take medication outside the home | |||
| Frequency of taking their medications outside more than once a week (►Figure 2) | 51 (45.5%) | ||
| How to carry or where to keep their medication (multiple answer allowed) | |||
| In a bag | 30 | ||
| In a pocket | 13 | ||
| In a wallet or a commuter-pass holder | 8 | ||
| In a office desk drawer | 2 | ||
| Other | 2 | ||
| How to store their medication at home | |||
| Divided into dosage groups using so-called “pill organizers” (cutting heat-sealed sheets of pills into the amount for a single dose1) (►Figure 3A) | 42 (37.5%) | ||
| Divided into individual medication groups using some kinds of containers (►Figure 3B) | 24 (21.4%) | ||
| Keeping paper bags given at pharmacies2 | 20 (17.9%) | ||
| Keeping by a single pill bag which contains all the medication for a single dose (most of the time, multiple medication are in the same bag) | 13 (12%) | ||
| Others (organizing medications using other kinds of containers, etc.) | 13 (12%) | ||
1One sheet contains only single kind of medication
2Basically, multiple kind of pill sheets inside the same bag depending on the timing of dose. e.g. three times a day (after breakfast, lunch and dinner), twice a day (after breakfast and dinner), etc.)
3.2 Design of the medication self-management system
We aimed to design a smartphone-based medication self-management system (SMSS) that could fulfill all of the necessary functions listed in ►Table 1 as well as any identified from the interviews. This system required two main functions, which are described in the next paragraph, for supporting medication self-management anytime and anywhere; even in the event of emergencies or disasters when no mobile internet connection is available. ►Figure 1 shows the main functions and the design of the system.
Fig. 1.
Architecture of the smartphone-based medication self-management system (SMSS)
The first function was to store and provide an accurate and portable medication history for patients, as well as recording their medication-taking, in a smartphone. A number of pill reminder applications on smartphones have some of these functions. However, data of medication-taking in these applications are sometimes not accurate because they depend on manual entry by the patients. In particular, patients can forget to enter the information despite having taken their medication.
The second function was to provide patients with reminders to take their medication only when they have forgotten. Regular reminders are not efficient with respect to the following two points: (i) alert fatigue might occur in the case of long-term medication usage [21, 22]; and (ii) a reminder without checking the records of medication-taking has a potential risk for the patient to take medication again even if he/she has had already taken it.
These two functions were realized by two data input methods: (a) reading prescription data printed in a two-dimensional (2D) barcode (QR code™) using a smartphone camera and getting the photographic images of the pills; and (b) real-time monitoring of medication-taking by a novel pillbox with an automatic wireless sensor of opening and closing (wireless electronic pillbox). Recently, 2D barcodes for prescription data were introduced for printing on formal prescriptions in Japan, and they are compliant with the 2D symbols for prescriptions of the Japanese Association of Healthcare Information Systems Industry [23].
3.3 Feasibility study of the function of reminders
We conducted a study to demonstrate the feasibility of the function whereby a reminder was provided by means of a message from the wireless electronic pillbox to the smartphone when the patient forgot to take his/her medication. Ten patients, who were taking oral medication every day, were recruited for this study. Patients who were under 20 years of age or over 75 years of age were excluded. Before starting the study, both medication prescription data and the scheduled medication time were entered into the smartphone by the researchers. Patients started using the smartphone and the pillbox for taking their medication after probation period of a week. When a patient forgot to take his/her medication, the patient received a voice and vibration alert from his/her smartphone once. After completion of the study, the patients were interviewed concerning the acceptability of the reminder system, wireless pillboxes, and medication history in their smartphones.
3.4 Analysis
Descriptive statistics with simple frequencies are presented at the interviews and the feasibility study.
4. Results
4.1 Interviews concerning how patients can manage their own medication
A total of 132 patients visited during office hours during the study. All patients were contacted by the researcher and 116 (75 male, 41 female; age range: 40–99 years) gave oral informed consent. Of 37 patients who were older than 70 years of age, 27 (73.0%) used their own mobile phones, indicating that even elderly patients could use a mobile phone as a user device in the system (►Table 2).
Eighty-five patients (75.9%) did not remember their entire medication regimen correctly. Forty-six patients (41.1%) forgot to take their medication, or took their medication more than two hours behind schedule, more than once a week according to their self-reports.
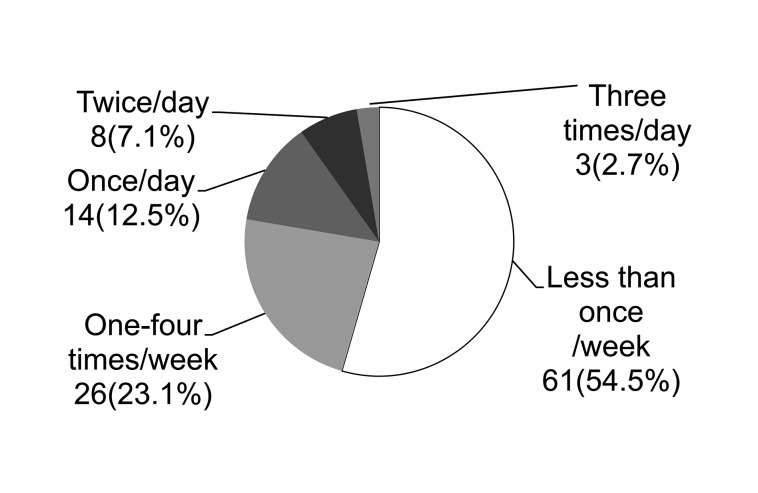
A total of 51 patients (45.5%) took their medications outside the home more than once a week (►Fig. 2). Most patients (a total of 51 patients) carried their medications in bags or in pockets to take those when they were away from home. These results indicated that pillboxes for portable use is required to support ubiquitous medication self-management and those should be pocket-sized.
Fig. 2.
Interviews result: number (percentage) of patients and frequency of taking medication outside the home
At home, with regard to dose and timing of medication, 42 patients (37.5%) managed them by cutting heat-sealed sheets of pills and using so-called “pill organizers” (►Figure 3A). Although this method is superior in terms of visual confirmation of medication adherence, an interviewee reported that it took 1 hour to allocate medicines in a pill organizer each month. Twenty-four patients (21.4%) managed their medication using separate sheets (►Figure 3B). These results indicated that pillboxes for home use should be adaptable to the different means of pillbox storage (►Table 3).
Fig. 3.

Photographs of a typical medication management system for home use. (A) Medication divided into dosage groups; (B) individual medication groups. (A typical sheet contains 10 or 14 tablets. Patients are generally given medications by the sheet in Japan.)
4.2 Development of a medication self-management system
We used an Android OS V1.6-based smartphone (Xperia; NTT DOCOMO), and core data were stored in the smartphone using a relational database engine (SQLiteV3.6.22; SQLite Consortium) synchronized with a database server (MySQL5.1; Oracle, Inc.). We used the Java language to develop the smartphone-based Android software using the Eclipse integrated development environment.
4.2.1 Data management of medication history and medication-taking
For the first function, namely “data management of medication history and medication-taking”, the patient’s smartphone was programmed to display the following information: medication history, current prescriptions, medication-taking records, calendar, adherence rate information, numbers of remaining tablets, and records of patients’ conditions (►Figure 4).
Fig. 4.
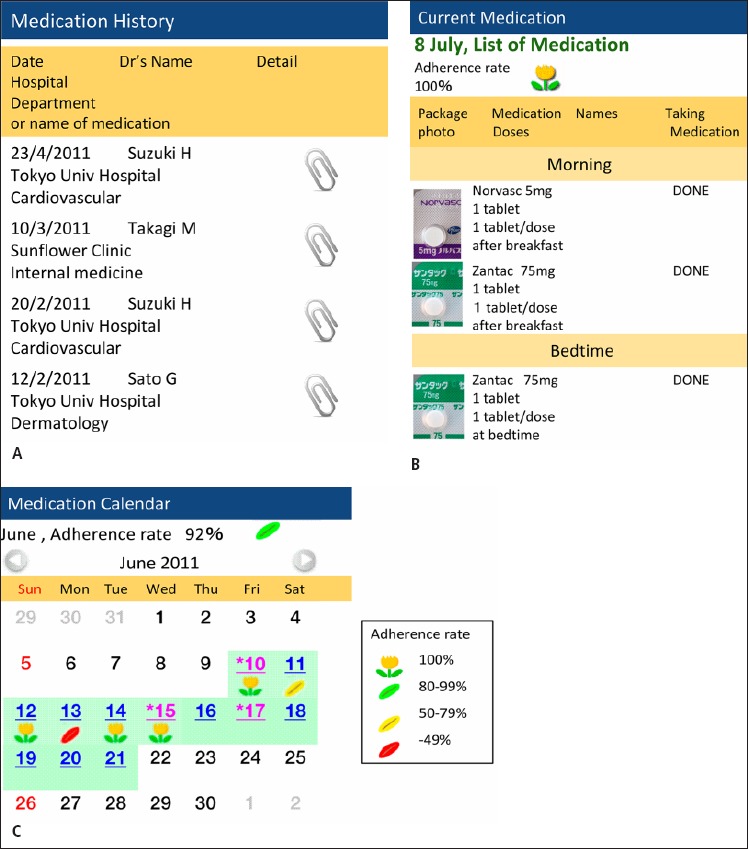
Medication information displayed by the “Ahkusuri” application on a smartphone showing: (A) medication history; (B) current medication; and (C) medication calendar with the adherence rate displayed.
4.2.2 Reminder to take medication
For the second function, “reminder to take medication only when the patient has forgotten”, we used real-time medication monitoring by wireless pillboxes that sensed the motion of opening. The event was automatically entered into the database inside the smartphone via a Bluetooth network. When patients took their medication, but not on time, they were requested by the system to input the record into the smartphone manually. When there was no record of taking medication after the scheduled medication time, a voice or vibration reminder was triggered by the smartphone within a predefined length of time. If the pillbox was opened more than once within a designated amount of time, the smartphone alerted patients to check their medication schedule to prevent them taking a double dose.
4.2.3 Reading of prescription data represented in 2D barcodes and getting the photographic images of the pills
The first data input method, “reading of prescription data printed in 2D barcodes using the camera of a smartphone”, allowed accurate dosage regimen data to be input into the smartphone easily by patients, even in the case of patients who had several medications. During our interviews, the average number of daily medications reported was 7.6, as shown in ►Table 2. After the 2D barcodes were added to the database of the smartphone, a photographic image of the data of the medicines was instantly imported from a pharmaceutical database on the web and displayed (►Figure 4B).
4.2.4 Real-time medication monitoring by wireless pillboxes
For the second data input method, “real-time medication monitoring”, a novel user-friendly wireless pillbox system was developed. Based on data from the interviews, pillboxes for portable use should be pocket-sized and the one for home use should be adaptable to the different means of pillbox storage, we chose two types of commercial pillboxes for development: one for home use and the other for portable use (►Figure 5A, B). The pillbox chosen for home use had 21 small compartments (New Kusuriyoubi, Medical Plan, Japan) for a week’s medication. The pillbox could be adapted to storage by “medication dosage groups” or “individual medications” (►Figure 3A, B). The pillbox chosen for portable use (supplements case, FANCL Corporation, Japan) was pocket-sized for ease of carriage.
Fig. 5.

Wireless pillboxes. (A) Pillbox for home use; (B) pillbox for portable use.
We next developed a mechanical and electronic module composed of a microcontroller unit, a Bluetooth device, and a switch sensor to sense whether the pillbox was open or closed, and embedded the module into the two types of pillboxes. The pillbox for home use required two size C batteries, and the one for portable use required four size AAA batteries.
The cost of each pillbox was approximately 100 US dollars, which could be reduced by one-third by mass production. This device was sufficiently inexpensive, and had the capability of accurately recording medication-taking.
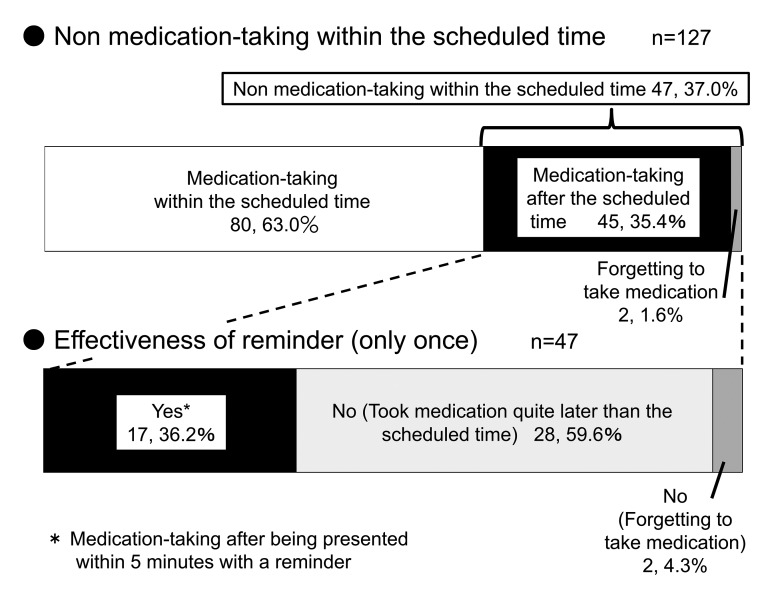
4.3 Feasibility study of the function of a reminder system
Ten eligible patients (5 male, 5 female; mean age: 57.3 years) participated in the feasibility study (►Table 4). There were a total of 133 dose timings. Six dose timing data could not be obtained because the patients did not carry the wireless pillboxes outside (three data) or because no data could be obtained from the wireless pillboxes (three data). A total of 127 dosing data were included in the timing analysis.
Table 4.
Characteristics of patients in the feasibility study (n = 10)
| Characteristic | Value | |
|---|---|---|
| Age (years, mean ± SD) | 57.3 ± 15.2 | |
| Male sex | 50% | |
| Average number of daily medicines (mean ± SD) | 2.5 ± 1.3 | |
| Taking medicines (person) | ||
| once/day | 5 (50 %) | |
| twice/day | 2 (20%) | |
| three times/day | 2 (20%) | |
| four times/day | 1 (10%) | |
| Frequency of forgetting to take medication before the study (self-reported, person) | ||
| Less than 4 times a year | 3(30%) | |
| Once every 2–3 months | 0(0%) | |
| 1–3 times a month | 4(40%) | |
| 1–6 times a week | 2(20%) | |
| Everyday | 1(10%) | |
“Not taking medicine within the scheduled time” occurred 47 times out of 127 (37.0%). In 17 of the 47 occasions (36.2%), patients took their medication upon being presented with a reminder only once (►Figure 6). Eight out of 10 patients reported that the reminders were effective. Eight out of 10 patients were satisfied with the system, and seven wanted to continue using the system.
Fig. 6.
Effectiveness of only one reminder for medication-taking during the study
5. Discussion
We developed a new type of medication self-management system using smartphones that addressed deficiencies in existing self-medication tools. This system would improve medication adherence by allowing patients to keep their medical information to hand in their pockets. Additionally, such a system would facilitate lifestyle modification, which remains a key aspect in chronic disease management [24].
5.1 Improvement of a reminder system
In the feasibility study, not all of reminders were effective for patients to take their medication in case they were away from the smartphone or they did not notice the small sound of reminders. We would design and improve reminders to repeat second or third time in user’s favorite interval, to display some messages about reminders on the smartphone until the patient inputs records of medication-taking, or to send a reminder to their home phone.
5.2 Medication history in a patient’s smartphone
In Japan, notebooks are widely used to record a patient’s medication history provided by a pharmacy. However, few patients carried such notebooks with them at all times or remembered their entire medication regimen correctly at our interviews. Furthermore, at the Great East Japan Earthquake and Tsunami in 2011, healthcare professionals at medical institutions in the evacuation area had trouble in identifying medications that patients had been taking [25]. Therefore, we think it is important that smartphones have the function to store medication history to allow information to be available when visiting a different hospital or even in the event of emergencies or disasters. Moreover, medication history in a smartphone can be incorporated into personal electronic health record systems.
To store an accurate medication history on patients’ smartphones, we used 2D barcodes as a means of providing prescription data to patients from healthcare providers. Patients can use those codes to maintain their history by themselves when they get prescriptions. We believe that 2D barcodes could be implemented in healthcare provider systems at low cost in short-term development compared to other methods (for example ICT cards or online).
5. 3 Importance of storing medication-taking records on a patient’s smartphone
The wireless pillboxes in this study provided a system to determine objectively patient adherence to medication-taking. For healthcare professionals, the report of objective adherence data would be extremely useful for assessing the effectiveness of treatment, because the data are not currently collected in general practice. Moreover, the data would be useful in clinical research studies.
For patients, accessibility to medication records and adherence rate information may motivate them to become more involved in managing their own medication. Further, the photographic images of the pill may be not only useful for checking the shape and color of the pill.
5. 4 Future perspectives
A previous study suggested that automated reminders with mobile communication would be effective in improving adherence [26]. Since the database on a smartphone is synchronized with the sub-database of the server in the proposed system, the sub-database could be able to share data on medication-taking or a record of the patient’s condition with healthcare professionals (►Figure 1). We believe that this function not only has great potential for promoting shared decision-making but facilitates general communication. A previous study revealed that failure to adopt personal health record systems was often linked with a lack of consumer involvement during planning, design, and implementation of communication systems [27]. The system we have developed would facilitate involvement of the patient and allow for communication between the patient and practitioner.
Future research is underway to provide a larger and longer scale evaluation by cross over study, such as on-reminder and off-reminder (only record medication-taking records). We should consider the study design carefully to evaluate SMSS as the least potential bias of period, carry over effects, and patients’ emotional effects. A data-sharing function between patients and healthcare professionals would also be developed.
5.5. Limitations
The primary limitation of this feasibility study was the limited generalizability to the broader population because of the small sample size, and the inclusion of participants with a variety of diseases and differences in awareness of medication-taking. Another limitation was that the study period was too short to demonstrate the feasibility, which would become evident with long time use. Further larger and longer term studies are warranted to overcome these limitations.
6. Conclusions
We developed the SMSS to monitor medication-taking in real time, and to provide reminders for medication-taking. The system has the advantage of using personal smartphones to store an accurate medication history. This feasibility study indicated that the SMSS is acceptable to patients. We believe that this proposed system is feasible and provides a robust innovative solution to the management of medication using mobile ICT.
Clinical Relevance Statement
A feasible smartphone-based medication self-management system with real-time medication monitoring was developed using 2D barcodes and user-friendly wireless pillboxes. The system offers patients two main functions: (1) storing and providing an accurate, portable personal medication history and medication-taking record; and (2) providing a reminder to take medication only when the patient has forgotten to take his/her medication. The proposed system was acceptable to patients.
Conflict of interest
The present study was supported in part by NTT DOCOMO, Inc., a commercial company providing communication systems for smartphones.
Protection of Human and Animal Subjects
The interviews were approved by the Research Ethics Committee of the Graduate School of Medicine, The University of Tokyo. The present study was conducted after receiving oral informed consent from each patient (Approval No. 2966). The feasibility study was also approved by the Committee and was conducted after receiving written informed consent from each patient (Approval No. 3243).
Acknowledgments
Special thanks to all participants involved in this study, and in particular to those who gave us useful advice on study methodology.
References
- 1.Eagleton J, Walker F, Barber N. An investigation into patient compliance with hospital discharge medication in a local population. Int J Pharm Pract 1993; 2: 107-109 [Google Scholar]
- 2.World Health Organization Adherence to Long-Term Therapies: Evidence for Action. Geneva, Switzerland: World Health Organization; 2003. [Cited 2012 June 27]. Available from: http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf [Google Scholar]
- 3.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005; 353(5): 487-497 [PMID:16079372] [DOI] [PubMed] [Google Scholar]
- 4.Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev 2008; 2: CD000011 [PMID:18425859] [DOI] [PubMed] [Google Scholar]
- 5.Simpson SH, Eurich DT, Majumdar SR, Padwal RS, Tsuyuki RT, Varney J, et al. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ 2006; 333(7557): 15-21 [PMID:16790458] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bosworth HB, Granger BB, Mendys P, Brindis R, Burkholder R, Czajkowski SM, et al. Medication adherence: A call for action.Am Heart J 2011; 162(3): 412-424 [PMID: 21884856] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments.AIDS Care 2000; 12(3): 255-266 [PMID:10928201] [DOI] [PubMed] [Google Scholar]
- 8.Zogg JB, Woods SP, Sauceda JA, Wiebe JS, Simoni JM. The role of prospective memory in medication adherence: a review of an emerging literature. J Behav Med 2012; 35(1): 47-62 [PMID:21487722] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boulos MNK, Wheeler S, Tavares C, Jones R. How smartphones are changing the face of mobile and participatory healthcare: an overview, with example from eCAALYX. Biomed Eng Online 201; 10: 24-37 [PMID:21466669] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clifford GD, Clifton D. Wireless Technology in Disease Management and Medicine. Ann Rev Med.2012; 63: 479-492 [PMID:22053737] [DOI] [PubMed] [Google Scholar]
- 11.Fenerty SD, West C, Davis SA, Kaplan SG, Feldman SR. The effect of reminder systems on patients’ adherence to treatment. Patient Prefer Adher 2012; 6: 127-135 [PMID:22379363] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lester RT, Ritvo P, Mills EJ, Kariri A, Karanja S, Chung MH, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet 2010; 376: 1838-1845 [PMID:21071074] [DOI] [PubMed] [Google Scholar]
- 13.Da Costa TM, Barbosa BJP, E Costa DAG, Siqulem D, Marin HF, Filho AC, et al. Results of a randomized controlled trial to assess the effects of a mobile SMS-based intervention on treatment adherence in HIV/ AIDS-infected Brazilian women and impressions and satisfaction with respect to incoming messages. Int J Med Inform 2012; 81(4): 257-269 [PMID:22296762] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahtani KR, Heneghan CJ, Glasziou PP, Perera R. Reminder packaging for improving adherence to self-administered long-term medications (Review). Cochrane Database Syst Rev 2011; 9: CD005025 [PMID:21901694] [DOI] [PubMed] [Google Scholar]
- 15.Zedler BK, Kakad P, Colilla S, Murrelle L, Shah NR. Does packaging with a calendar feature improve adherence to self-administered medication for long-term use? A systematic review. Clin Ther 2011; 33(1): 62-73 [PMID:21397775] [DOI] [PubMed] [Google Scholar]
- 16.Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ 2008; 336(7653): 1114-1117 [PMID:18480115] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haberer JE, Robbins GK, Ybarra M, Monk A, Ragland K, Weiser SD, et al. Real-Time electronic adherence monitoring is feasible, comparable to unannounced pill counts, and acceptable.Behav AIDS 2011; 16(2): 375-382 [PMID:21448728] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hayes TL, Hunt JM, Adami A, Kaye JA. An electronic pillbox for continuous monitoring of medication adherence. Conf Proc IEEE Eng Med Biol Soc 2006; 1: 6400-6403 [PMID:17946369] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moore DJ, Palmer BW, Patterson TL, Jeste DV. A review of performance-based measures of functional living skills. Psychiatr J Res 2007; 41(1–2): 97-118 [PMID: 16360706] [DOI] [PubMed] [Google Scholar]
- 20.Orwig D, Brandt N, Gruber-Baldini AL. Medication management assessment for older adults in the community. The Gerontologist 2006; 46(5): 661-668 [PMID: 17050757] [DOI] [PubMed] [Google Scholar]
- 21.Gerber BS, Stolley MR, Thompson AL, Sharp LK, Fitzgibbon ML. Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: a feasibility study.Health Inform J 2009; 15(1): 17-25 [PMID:19218309] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Phansalkar S, Edworthy J, Hellier E, Seger DL, Schedlbauer A, Avery AJ, et al. A review of human factors principles for the design and implementation of medication safety alerts in clinical information systems. J Am Med Inform Assoc 2010; 17(5): 493-501 [PMID:20819851] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The Japanese association of healthcare information systems industry (JAHIS) [Cited 2012 June 27]. Available from: http://www.jahis.jp/english/>
- 24.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA 2002; 288(19): 2469-2475 [PMID:12435261] [DOI] [PubMed] [Google Scholar]
- 25.Yamamoto T, Kato M, Shirabe S.Life, health, and community in a tsunami-affected town. Lancet 2011; 378(9788):318 [PMID: 21784268] [DOI] [PubMed] [Google Scholar]
- 26.Granger BB, Bosworth HB. Medication adherence: emerging use of technology. Curr Opin Cardiol 2011; 26(4): 279-287 [PMID:21597368] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Archer N, Fevrier-Thomas U, Lokker C, McKibbon KA, Straus SE. Personal health records: a scoping review. J Am Med Inform Assoc 2011; 18(4): 515-522 [PMID:21672914] [DOI] [PMC free article] [PubMed] [Google Scholar]