Abstract
An endobronchial leiomyoma is a rare tumor of the bronchial tree. Very few cases have been reported in literature. Leiomyomas account for less than 2% of all benign lung tumors. Only one third is endobronchial in location, usually presenting as primary solitary lesions and airway obstruction findings. Literature on primary endobronchial leiomyomas is therefore scarce, with a few more than 100 cases being reported. These tumors arise from the smooth muscle of the bronchial tree. Symptomatology is based on the degree of endoluminal bronchial obstruction and surgical resection has generally been the mainstay of treatment. We describe a case of endobronchial leiomyoma in a 42 year old female. A diagnosis of Primary endobronchial leiomyoma was made on the basis of histopathology and immunohistochemistry. Rarity of this tumor in the bronchial tree with coexisting interstitial peumonitis urges us to report this case.
KEY WORDS: Benign tumor, bronchial tree, endobronchial leiomyoma
INTRODUCTION
Benign neoplasms comprise less than 10% of tumors involving the trachea and main stem bronchi. Leiomyoma of the airways is a rare benign tumor, usually described as being a solitary tumor.[1] Primary pulmonary leiomyoma are extremely uncommon both in adults and children, constituting approximately 2% of benign lung tumors. The affected patients usually have respiratory symptoms due to partial or complete airway obstruction which may simulate asthma or be complicated with bronchiectasis and recurrent pulmonary infection. Only one third of primary pulmonary leiomyomas are endobronchial in location, Literature on primary endobronchial leiomyomas is scarce, with a 2009 review reporting only 108 cases. The majority of lung leiomyomas, approximately 51%, are located in the parenchyma, endobronchial accounts for 33% and trachea for the remaining 16%.
CASE REPORT
A 42 years old, housewife presented with history of breathlessness on exertion and non –productive cough since 4 months. There was also history of mild fever inter-mittently. At the time of presentation patient was already on steroids for the last 10 days without any relief of symptoms. On examination she was afebrile. The vital parameters were within normal limits. There was no clubbing, cyanosis or lymphadenopathy. Auscultation revealed bilateral fine crepts at the bases. Rest of the physical examination was within normal limits. The patient's laboratory findings were as follows: Hb-13.0 gm/dl, Packed Cell Volume-41.0%. Total Leukocyte Count-9800/cumm, Polymorhs-65%, Lymphocytes-30%, Eosinophils-02%, Monocytes-03%, Platelets-3.325 lacs/cumm, Erythrocyte Sedimentation Rate-30mm/hr. Rheumatoid Arthiritis factor, Antinuclear Antibody profile:c- ANCA ,p- ANCA , anti-double stranded DNA were all negative. Other blood investigations like liver function tests, renal function tests, thyroid profiles were all within normal range. Sputum was negative for Acid Fast Bacilli. Chest X-ray showed Bilateral lower zone reticulonodular shadows. High resolution computed tomography (HRCT) thorax [Figures 1 and 2] showed areas of air space opacification, interlobular and subpleural interstitial thickening noted in both lower lobes and right middle lobe. Pulmonary function testing (PFT) showed severe restriction. 2D echocardiography was normal Left ventricular ejection fraction (LVEF) of 60 %. Bronchoscopy was done to obtain bronchioalveolar lavage for analysis. Upon bronchoscopy tumor like lesions were seen obstructing the apicoposterior segments of the Right upper lobe [Figure 3a–c]. Bronchial washings and biopsy samples were taken from the lesion. Microscopic examination of the bronchial lavage showed bronchial epithelial cells and polymorphs. Bronchial biopsy [Figure 4] histopathological examination showed intact pseudostrafied ciliated columnar epithelium. The tumor was composed of bundles and whorls of spindle shaped cells with monomorphous fusiform nuclei and acidophilic cytoplasm without cytonuclear atypia, mitotic cells or areas of necrosis. A diagnosis of endobronchial leiomyoma with interstitial pneumonitis was made. Ultrasonography (USG) abdomen and complete gynecological examination did not reveal any evidence of a leiomyoma in the uterus or elsewhere. Immunohistochemistry was consistent with a myogenic tumor as it showed diffuse cytoplasmic reactivity for smooth muscle actin and desmin. Inspite of extensive search no literature regarding endobronchial leiomyoma with a coexisting interstitial pneumonitis could be found. We managed the two conditions as different unrelated entities and patient was treated with steroids and antibiotics to which she responded very well in two weeks time. On review there was near complete resolution of reticulonodular shadows in the lower zones seen at the initial visit. There was decrease in symptoms (cough, dyspnoea, fever.). Oncology opinion was taken but as tumor was benign and had caused no significant endobronchial obstruction with not even sub-segmental collapse conservative management was advised while keeping the patient on regular follow up.
Figure 1.

HRCT Thorax: Showing-relatively normal upper lobes
Figure 2.
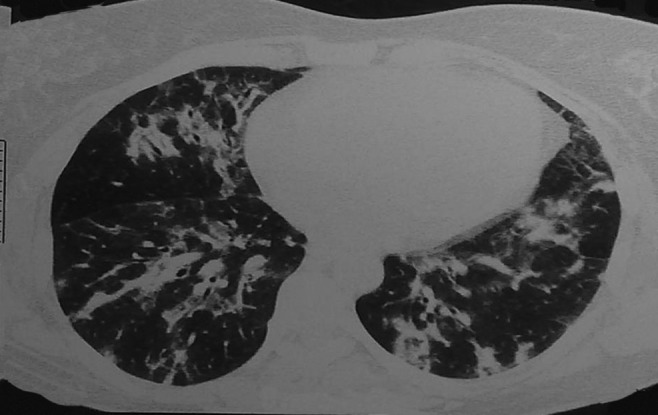
HRCT Thorax: Showing-findings of air space opacification, centrilobular nodules and interstitial thickening mainly involving both lower lobes
Figure 3a.

Bronchoscopy image showing leiomyoma
Figure 3c.
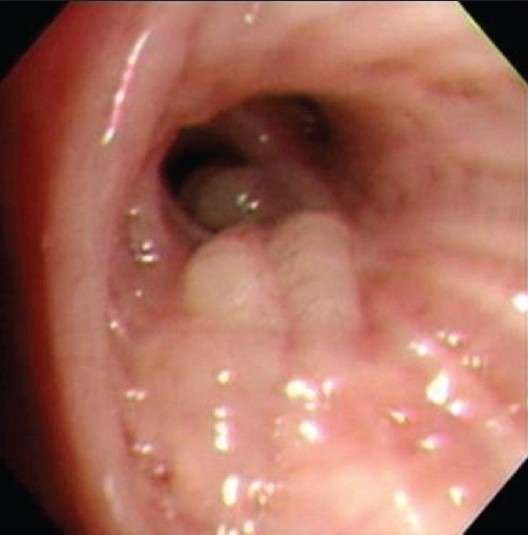
Bronchoscopy image showing leiomyoma
Figure 4.
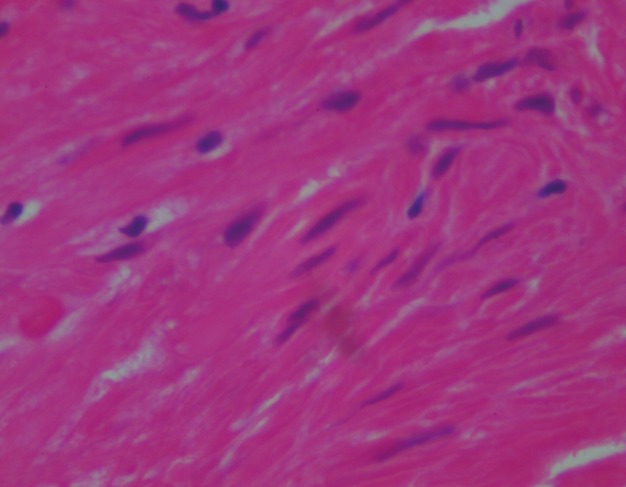
Submucosal tumour composed of cells arranged in whorls and fascicles, monomorphic cells with spindly nuclei. No necrosis or mitotic activity. Overall histopathology is consistent with benign spindle cell tumour-leiomyoma
Figure 3b.

Bronchoscopy image showing leiomyoma
DISCUSSION
The bronchial tree is a most unusual site for a leiomyoma that too with concomitant interstitial pneumonitis. Leiomyoma is a benign tumor of the smooth muscles. It is common in the uterus, but very uncommon in the smooth muscles of extrauterine sites. When they are located in other than well-known locations, i.e., oesophagus, small intestine or uterus, generally they are symptom free and detected by chance while performing routine check-up measures or diagnostic studies for other pathologies. Other locations of leiomyomas include thyroid,[2] extrapleural chest wall, lungs, trachea[3,4] and bronchi. Till date only very few cases have been reported in the world literature. Bronchial leiomyomas are benign tumors which predominantly occur in the fourth decade of life with female preponderance.[5,6] Bronchial leiomyomas are thought to arise from the smooth muscle cells of the bronchial wall and the interstium or from the smooth muscles of the arterioles. Leiomyomas of the respiratory tract can be termed according to site of occurrence e.g.,-tracheal bronchial, parenchyma based on the anatomical site of occurrence. The definitive diagnosis can be made by bronchoscopy which enables us to visualise the lesion as well as take samples for hisopathological analysis. Patients with bronchial leiomyomas usually have respiratory symptoms due to partial or complete obstruction of the affected bronchus.[7] Endobronchial growth can cause cough, wheeze, haemoptysis. Shortness of breath, chest pain, fever, chronic and recurrent episodes of pneumonitis in the same part of the lung. Parenchymal or peripheral leiomyoma will present as asymptomatic solitary nodule. Endobronchial leiomyomas are amongst the rarest of benign neoplasms of the lower respiratory tract. There is a female preponderance in the occurrence of the tumor. Development of smooth muscle neoplasm have reported in different conditions with immune deficiency, including acquired immunodeficiency syndrome (AIDS), particularly in children with cellular immune deficiencies and malignant lymphoma Epstein- Barr virus has also been detected in almost all AIDS- related smooth muscle neoplasms and in the reported case of bronchial leiomyoma in a boy with cellular immunodeficiency.[8] Endobronchial EBV-associated leiomyomas in adults are very rare tumors. They should be included in differential of endobronchial polyps in immunosuppressed patients. They have been reported in the literature mainly in children with congenital HIV; however, they can also be seen in adults The association of leiomyoma and HIV infection has been reported in a boy with a cellular immunodeficiency,[8] who had endobronchial leiomyoma. A case of an EBV -associated endobronchial leiomyoma was discovered in an adult patient with congenital AIDS[9] with Pneumocystis pneumonia. Histological criteria, including cellularity, mitotic activity, and pleomorphism have been proposed to differentiate between benign and malignant smooth muscle neoplasms. The principle criterion is mitotic activity that should be less than 5 per 50 HPF.[10] In the present case all morphologic findings were compatible with a benign spindle cell tumor. The treatment should be as conservative as possible since the tumor is usually benign. These tumors do not need to be removed unless clinically causing symptoms. Other treatment options include resection, highly active antiretroviral (HAART) in cases of AIDS and less often chemotherapy and radiotherapy. Surgery remains the mainstay of treatment for bronchial leiomyoma, type of surgery depending upon the location of the tumour. Treatment of bronchial leiomyoma should be conservative since the tumor is mostly benign. Localized resection, bronchotomy, segmental resection or bronchoscopic removals are different modes of surgery employed to treat the tumour. YAG laser or electrocautery can be used via bronchoscope to resect the tumor.[11]
CONCLUSION
Endobronchial leiomyomas are amongst the rarest of benign neoplasms of the lower respiratory tract. There is a female preponderance[5,12] in the occurrence of the tumor. The definitive diagnosis can be made by bronchoscopy which enables us to visualize the lesion as well as take samples for hisopathological analysis. The treatment should be as conservative as possible since the tumor is usually benign.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Ko SM, Han SB, Lee SK, Woo SK, Kim MJ, Keum DY, et al. Calcified endobronchial leiomyoma. Br J Radiol. 2007;80:91–3. doi: 10.1259/bjr/25631438. [DOI] [PubMed] [Google Scholar]
- 2.Erkiliç S, Erkiliç A, Bayazit YA. Primary leiomyoma of the thyroid gland. J Laryngol Otol. 2003;117:832–4. doi: 10.1258/002221503770716322. [DOI] [PubMed] [Google Scholar]
- 3.Park JS, Lee M, Kim HK, Choi YS, Kim K, Kim J, et al. Primary leiomyoma of the trachea, bronchus, and pulmonary parenchyma: A single-institutional experience. Eur J Cardiothorac Surg. 2012;41:41–5. doi: 10.1016/j.ejcts.2011.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bharadwaj SC, Unruh HW. Leimyoma of the trachea. Ann Thorac Surg. 2012;93:669–70. doi: 10.1016/j.athoracsur.2011.07.022. [DOI] [PubMed] [Google Scholar]
- 5.Taylor TL, Miller DR. Leiomyoma of the bronchus. J Thorac Cardiovasc Surg. 1969;57:245–8. [PubMed] [Google Scholar]
- 6.Sakaguchi M, Nakamura T, Shimizu T, Koike S, Kumeda S, Shigematsu H, et al. Leiomyoma of the lung: A case report. Kyobu Geka. 1999;52:157–60. [PubMed] [Google Scholar]
- 7.Perçinel S, Heper AO, Savafl B, Ceyhan K, Enön S, Güngör A. Bronchial Leiomyoma with Presumptive Diagnosis of Lung Carcinoma: A Case Report and Review of the Literature. Turk Respiratory J. 2008;9:41–5. [Google Scholar]
- 8.Hatano M, Takada H, Nomura A, Ohga S, Ohshima K, Saeki I, et al. Epstein-Barr virus: Associated bronchial leiomyoma in a boy with cellular immunodeficiency. Pediatr Pulmonol. 2006;41:371–3. doi: 10.1002/ppul.20375. [DOI] [PubMed] [Google Scholar]
- 9.Metta H, Corti M, Redini L, Dure R, Campitelli AM, Narbaitz M. Endobronchial leiomyoma: An unusual non-defining neoplasm in a patient with AIDS. Rev Inst Med Trop Sao Paulo. 2009;51:53–5. doi: 10.1590/s0036-46652009000100010. [DOI] [PubMed] [Google Scholar]
- 10.Sharifi N, Massoum SH, Shahri MK, Rezaei A, Ashari AA, Attar AS, et al. Endobronchial leiomyoma: Report of a case successfully treated by bronchoscopic resection. J Res Med Sci. 2010;15:364–70. [PMC free article] [PubMed] [Google Scholar]
- 11. [Last accessed on 2012]. Available from: http://www.ispub.com: 80/journal/the-internetjournal-of-thoracic-and-cardiovascular-surgery/volume-7-number-2/endobronchial-leiomyoma-successful-resection- by-sleeve-lobectomy.html .
- 12.Bilgin S, Yilmaz A, Okur E, Düzgün S, Tahaoğlu C, Akkaya E. Primary endobronchial leiomyoma: A case report. Tuberk Toraks. 2004;52:272–4. [PubMed] [Google Scholar]


