A 41-year-old woman presented to our attention with shortness of breath and occasional blood-tinged sputum. Chest radiography and chest computed tomography (CT) were carried out [Figure 1a and b]. The patient presented a history wherein there was a case of hysterectomy due to multiple leiomyomas 15 years back.
Figure 1.
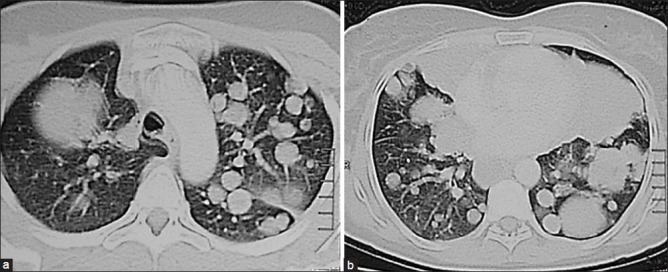
Chest computed tomogram at the upper lobe (a) and the lower lobe (b) levels showing bilateral multiple variable-sized pulmonary nodules
QUESTION
What can be the possible diagnosis?
ANSWER
Chest CT revealed bilateral multiple variable-sized lung nodules. Metastatic solid organ malignancy is the most likely diagnosis. Other differential diagnoses to be considered include septic emboli, fungal infection, non-inflammatory conditions such as sarcoidosis, lymphomatoid granulomatosis, amyloidosis, arteriovenous malformations, pneumoconiosis, and inflammatory conditions such as rheumatoid arthritis or Wegner's granulomatosis.
Histopathologic examination of lung biopsy showed proliferating atypical spindle cells with smooth muscle features entangling glandular structures lined by columnar cells with no evidence of malignancy [Figure 2]. The cells were positive for smooth muscle actin [Figure 3] but negative for cluster of determination 117 (CD117) immunohistochemical staining. The histologic picture, together with the clinical data, supports a diagnosis of benign metastasizing leiomyoma (BML) of the lung.
Figure 2.
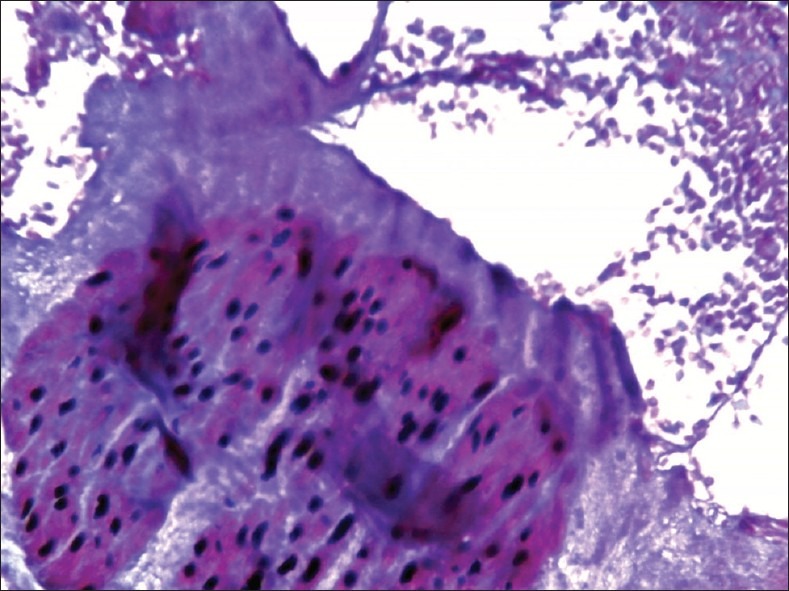
Interlacing bundles of benign smooth muscle fibers (H and E, ×200)
Figure 3.
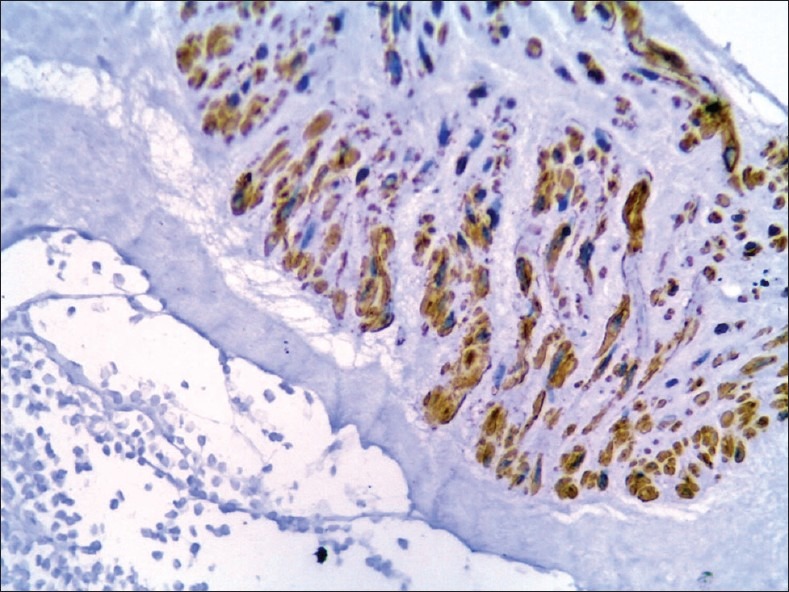
Cells are positive for smooth muscle actin immunostaining, (×200)
COMMENT
Many authors belie the existence of benign metastasizing leiomyoma and consider it together with the primary uterine lesion as a low-grade leiomyosarcomas. Other authors depend on the absence of cellular atypia, tumor necrosis, and vascular invasion, together with a low mitotic index, to support the true benign nature of the lesion.[1] Microemboli from the uterine leiomyoma may enter the venous or lymphatic channels at the time of myomectomy or hysterectomy and seed distant organs.
BML usually presents during the reproductive period of a female, but some cases may occur after menopause. Lung BML is usually asymptomatic, and most cases are discovered as incidental findings on chest radiographs. However, the patients may present with symptoms such as cough, chest pain, dyspnea, or hemoptysis. Diffuse involvement of the lung finally ends with respiratory failure and death. Radiographically, the presentation of lung BML ranges from solitary pulmonary nodule to multiple bilateral masses. Other radiological features such as cystic masses, miliary nodules, or diffuse reticulonodular densities mimicking interstitial lung disease were reported. Histopathologic examination is the cornerstone in diagnosis. The obtained material should be examined for expression of estrogen and progesterone receptors, as this provides the basis of estrogen depletion therapy.[2]
There is no standard model for the treatment of BML. Surgical resection of the primary source and metastatectomy of the lung lesion, if possible, should be the first step. The patient should be made estrogen-depleted, which is another important step, by performing bilateral oophorectomy and/or long-standing hormonal therapy. If surgical resection is not possible, hormonal therapy to induce shrinkage of the nodules is an alternative. Several medications have been tried, including a gonadotropin-releasing hormone agonist, progesterone (such as megestrol acetate), and tamoxifen. Systemic chemotherapy can be a last resort for recurrent or diffuse unresectable disease or when the tumor lacks expression of estrogen receptors.[3]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Rao AV, Wilson J, Sylvester K. Pulmonary benign metastasizing leiomyoma following hysterectomy: A clinicopathologic correlation. J Thorac Oncol. 2008;3:674–6. doi: 10.1097/JTO.0b013e3181757a46. [DOI] [PubMed] [Google Scholar]
- 2.Cohen DT, Oliva E, Hahn PF, Fuller AF, Jr, Lee SI. Uterine smooth-muscle tumors with unusual growth patterns: Imaging with pathologic correlation. AJR Am J Roentgenol. 2007;188:246–55. doi: 10.2214/AJR.05.1070. [DOI] [PubMed] [Google Scholar]
- 3.Lin YC, Wei LH, Shun CT, Cheng AL, Hsu CH. Disseminated peritoneal leiomyomatosis responds to systemic chemotherapy. Oncology. 2009;76:55–8. doi: 10.1159/000178761. [DOI] [PubMed] [Google Scholar]


