Abstract
Although studies have suggested that bone-marrow human mesenchymal stem cells (BM-hMSCs) may be used as delivery vehicles for cancer therapy, it remains unclear whether BM-hMSCs are capable of targeting cancer stem cells, including glioma stem cells (GSCs), which are the tumor-initiating cells responsible for treatment failures. Using standard glioma models, we identify TGF-β as a tumor-factor that attracts BM-hMSCs via TGF-β receptors (TGFβR) on BM-hMSCs. Using human and rat GSCs, we then show for the first time that intravascularly administered BM-hMSCs home to GSC-xenografts that express TGF-β. In therapeutic studies, we show that BM-hMSCs carrying the oncolytic adenovirus Delta-24-RGD prolonged the survival of TGF-β-secreting GSC-xenografts and that the efficacy of this strategy can be abrogated by inhibition of TGFβR on BM-hMSCs. These findings reveal the TGF-β/TGFβR-axis as a mediator of the tropism of BM-hMSCs for GSCs, and suggest that TGF-β predicts patients in whom BM-hMSC delivery will be effective.
Keywords: Mesenchymal Stem Cells, Glioma Stem Cells, Malignant Gliomas, Glioblastoma, Transforming Growth Factor-β
Introduction
The outcome of patients with malignant gliomas, particularly, glioblastoma (GBM), the most common adult glioma, remains poor. The median survival of patients with GBM is only 14 months despite surgery, concurrent chemoradiotherapy and adjuvant chemotherapy1. Successful treatment of malignant gliomas has not been achieved at least in part because of deficiencies in delivering therapeutic agents to the tumor2,3. To address this deficiency, we have used bone marrow-derived human mesenchymal stem cells (BM-hMSCs) as intravascular therapeutic delivery vehicles to gliomas. We have shown that intravascularly delivered BM-hMSCs selectively home to glioma xenografts and that BM-hMSCs can be used to deliver therapeutic agents to gliomas4,5. Although several studies have suggested that tumor-derived factors mediate the tropism of BM-hMSCs to gliomas6–8, the mechanism underlying the homing of BM-hMSCs to gliomas remains unknown. Understanding this mechanism is important for the development of BM-hMSCs with enhanced homing capacity or for identifying patients in whom this biological delivery system would be most effective.
Heretofore, nearly all studies evaluating the homing of BM-hMSCs, particularly after intravascular delivery, have relied upon commercially available mouse or human glioma cell lines, which imprecisely mimic the features of human gliomas4–6,9. However, current evidence suggests that gliomas, like other cancers, are comprised of a rare fraction of cells with stem-like properties, called cancer stem cells or Glioma Stem Cells (GSCs), which grow as spheroids in culture and which typically, although not invariably, express CD133 on their surface10,11. GSCs isolated from patient specimens recapitulate the genotype of human gliomas and xenografts of GSCs mimic the phenotypic characteristics of human gliomas10,11. In addition, GSCs may account for the poor outcome of patients with malignant gliomas, because they are resistant to most therapies and are likely responsible for persistent tumor recurrence10–12. Consequently, targeting and eliminating GSCs is an important therapeutic goal for eradicating gliomas13,14. Despite the importance of GSCs in glioma biology, however, there has been little information regarding the homing of BM-hMSCs to GSCs15,16.
Transforming Growth Factor-β (TGF-β) has been implicated in the migration of mesenchymal-like cells toward wounds17 and cancer has been characterized as a “wound that never heals”18. TGF-β is a secreted factor produced by many types of tumors, including gliomas, and is implicated in many tumor related functions19–21. Depending upon the method of analysis, 30–70% of gliomas express high levels of TGF-β19,20,22. Moreover, recent evidence indicates that TGF-β contributes to the self-renewal and tumorigenesis of GSCs21,23. Likewise, TGF-β has been implicated as a pro-angiogenic factor that mediates the formation of new vessels within human gliomas24,25. Given the importance of TGF-β in GSC biology, we hypothesized that TGF-β may mediate the homing of BM-hMSCs to gliomas and may be necessary for homing of BM-hMSCs to GSCs.
Consequently, we tested the causal role of TGF-β in the homing of BM-hMSCs to malignant gliomas using commercially available human glioma cell lines (U87, U251, LN229), isogenic GSCs with high and low TGF-β expression derived from rat C6 gliomas26,27 and human GSCs isolated directly from patients with GBMs10. We show that TGF-β directly mediates the homing of intravascularly administered BM-hMSCs to gliomas by acting on the TGF-β type II receptor (TGFβRII) and TGFβRII co-receptor, CD105, expressed on BM-hMSCs. We provide the first evidence that BM-hMSCs are capable to homing to GSCs after intravascular delivery, and that this homing depends upon GSC expression of TGF-β. Furthermore, BM-hMSCs carrying the oncolytic adenoviruses, Delta-24-RGD4, are an effective treatment for GSCs that express high levels of TGF-β. These findings provide insight into the possible use of BM-hMSCs as delivery vehicles to treat GBMs by targeting GSCs that maintain these cancers.
Materials and Methods
Cells
BM-hMSCs were obtained from Lonza (Walkersville, MD)4,6. U87MG and LN229 were obtained from ATCC (Manassas, VA). U251 were provided by W.K.A.Yung (MDACC). GSCs were established as previously described10. C6 GSCs were provided as previously reported26,27.
Plasmids and virus preparation
Lentiviruses were prepared as described elsewhere28. TGF-β and CD105 shRNA constructs were made in pLKO.1 vector using standard protocols. TGF-β was stably expressed with lentiviral vectors of pEZ-Lv105-TGFβ (GeneCopoeia, Rockville, MD).
Cell proliferation assay
5×104 cells were plated in triplicate in 6 well plates and cultured for 4 and 7 days. Viable cells were counted using Vi-Cell (Beckman Coulter I, Fullerton, CA).
Western blotting
Protein lysates under reducing condition (for phospho-Smad3 and total Smad2/3) or non-reducing condition (for TGFβRII and CD105) were separated by SDS-PAGE. Antibodies were detected by SuperSignal® (Thermo Scientific, Rockford, IL). Primary antibodies: anti-phospho-Smad3 (rabbit, 1:1000, Cell Signaling Technology, Danvers, MA), anti-Smad2/3 (rabbit, 1:1000, Cell Signaling Technology.), anti-TGF-βRII (goat, 1 μg/ml, R&D systems, Minneapolis, MN), anti-human CD105 (clone SN6, 2 μg/ml, Invitrogen, Camarillo, CA), and anti-α-tubulin (1:1000, BioLegend, San Diego, CA).
ELISA
The expression level of TGF-β1 in the conditioned media was quantified using Quantikine® ELISA kit (R&D Systems, Minneapolis, MN) according to manufacturer’s protocol.
In vitro transwell migration assay
Conditioned media (CM) from cells cultured in serum-free media for 72hrs at 1×105 cells/ ml, was placed in the lower well of 24 mm tissue culture Transwell plates (8μm pour, Corning, Corning, NY) and BM-hMSC migration was assessed as previously described5,6. For blocking TGF-β, CM was mixed with anti-human LAP-TGFβ1 neutralizing antibodies (R&D Systems) at a final concentration of 5 μg/ ml.
Determination of Short Tandem Repeat (STR) polymorphisms
The DNA of C6-glioma cells (Wistar rat), rat chondrosarcoma cells (RCS cells, Sprague Dawley)29 and rat-2 fibroblast cells (Fisher rat) was used as control. As previously reported30, STR polymorphism was determined by PCR using the oligonucleotide primers (Supplementary Table 1) corresponding to twelve STR markers. The PCR-products were denatured as previously reported31.
Immunostaining
The primary antibodies were: anti-mouse-CD31 (goat, 1μg/ml, R&D Systems), anti-GFP (rabbit, 1:500, Novus Biologicals, Littleton, CO), anti-human latent associate protein TGFβ1 (LAP-TGFβ1) (goat, 1μg/ml, R&D Systems)32.
Quantification of xenograft vascularity
Xenografts were stained with anti-CD31 antibody. Representative sections were analyzed by counting all vessels with lumina/branches in 10-hpf (400x).
Evaluation of the lamellipodia protrusions
Cells were plated in Lab-Tek permanox slides (Fisher Scientific); when confluent a central scratch was made using a 1ml-tip. After washing, serum-free media with or without latent TGF-β1 (1 ng/ml, R&D systems) was added. 48hrs later, cells were fixed with 4%PFA and stained with fluorescent phallotoxins (Molecular Probes., Eugene, OR) (counterstain DAPI). Cells were counted in eight areas (x400).
hMSCs homing toward gliomas
BM-hMSCs were transduced with Ad5/F35-CMV-GFP vector33 as previously described4,6. Quantitative assessments were performed as previously described 6.
BM-hMSC carrying Delta-24-RGD
Delta-24-RGD was loaded into BM-hMSCs as previously described 4.
Statistics
Statistical differences were assessed by Student’s t-test with significance if p <0.05. The data were represented as mean±standard deviations or standard errors for at least 3-replicate determinations for each experiment.
Results
TGF-β contributes to the homing of BM-hMSCs to established glioma cell lines in vitro and in vivo
To understand the feasibility of homing of BM-hMSCs towards GSC xenografts, we first tried to define the homing mechanism of BM-hMSCs towards established glioma cell lines, U87, U251 and LN2295, by exploring the tropic effects of TGF-β on BM-hMSC. Consequently, we determined the relationship between the amounts of TGF-β produced by these lines and the level of hMSC migration in vitro using ELISA and transwell migration assays. ELISA showed that U87 and U251 glioma lines produced higher amounts of TGF-β than LN229 (Fig. 1A). In this assay, active TGF-β (which has biological activity through binding TGF-β receptors) was not detected in the conditioned media from each glioma line (data not shown), and the conditioned media contained mostly latent TGF-β.
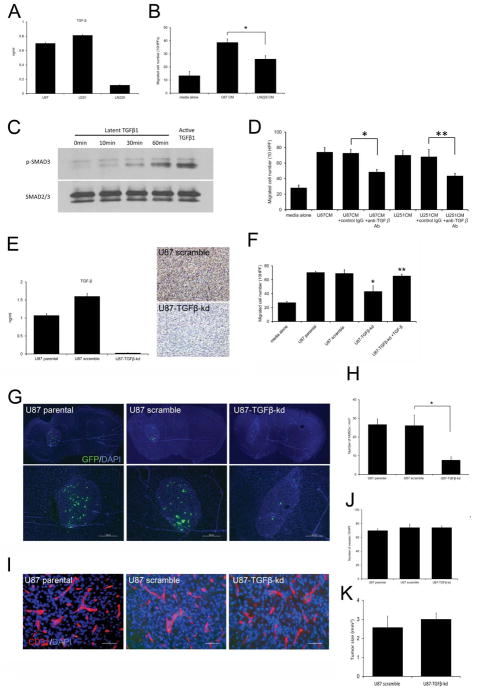
Figure 1.
TGF-β levels correlate with BM-hMSCs tropism
(A)The amount of TGF-β in the conditioned media from U87, U251 and LN229 cells by ELISA. Error bars, SDs.
(B)The migration of BM-hMSCs to the conditioned media of U87 cells (high TGF-β) compared with that of LN229 (low TGF-β). Error bars, SDs.
(C)Western blots showing expression of phospho-SMAD3 in BM-hMSCs at indicated time points after treatment with latent TGF-β. The treatment of active TGF-β for 10 min was used as positive control. Total SMAD2 /3 was the internal control.
(D)The migration of BM-hMSCs to the conditioned media of U87 or U251 cells with or without anti- TGF-β neutralizing antibodies. Error bars, SDs.
(E)The amounts of TGF-β in the conditioned media of U87 parental, U87 scramble or U87-TGFβ-kd cells by ELISA (left panel). Error bars, SDs. TGF-β expression in U87 scramble or U87-TGFβ-kd tumors by immunohistochemistry (right panels). Scale bars, 50μm.
(F)Migration of BM-hMSCs to conditioned media of U87-TGFβ-kd cells with or without TGF-β. Error bars, SDs.
(G) Homing of BM-hMSCs labeled with GFP to brain xenografts of U87-parental, U87-scramble, or U87-TGFβ-kd. The upper panels showing whole brains, lower showing the tumors. Scale bars, 500μm.
(H) Quantitative assessments of localization of BM-hMSCs. Error bars, SEs.
(I) Representative pictures of vessels in U87 parental, U87-scramble, and U87-TGFβ-kd brain tumors. Scale bars, 50μm.
(J) The number of vessels with lumina or branches in 10 high-power fields at a magnification of 400x. Error bars, SDs.
(K)Graph showing the average size of tumors before and after knock down of TGF-βError bars, SD.
In vitro transwell migration assays demonstrated that conditioned media from U87 (containing high amounts of TGF-β) resulted in a statistically significant increase in BM-hMSCs migration through matrigel compared with conditioned media from LN229 (containing low levels of TGF-β) (p<0.01, Fig. 1B), suggesting a correlation between TGF-β levels and BM-hMSC homing to gliomas. Since the conditioned media used in in vitro transwell migration assays contained largely latent TGF-β, we hypothesized that BM-hMSCs were capable of converting latent TGF-β to its active form. Since the half-life of active TGF-β is only a few minutes32, we indirectly measured active TGF-β by examining phospho-Smad3 in BM-hMSCs exposed to latent TGF-β. Western blots showed that phospho-Smad3 was expressed in BM-hMSCs after exposure to latent TGF-β in a time dependent manner (Fig. 1C), demonstrating that BM-hMSCs can convert latent TGF-β to active TGF-β.
To establish a causal role of TGF-β in BM-hMSC migration, we performed in vitro transwell migration assays using neutralizing antibodies against TGF-β. Treatment of conditioned media from U87 or U251 with the TGF-β neutralizing antibodies significantly attenuated hMSC migration compared with control (nonspecific IgG) conditioned media (p<0.05, Fig. 1D).
To further demonstrate a causal relationship between TGF-β expression and hMSC homing, TGF-β1 was stably knocked down in U87 glioma cells (generating U87-TGFβ-kd). ELISA confirmed decreased TGF-β expression in the knockdown U87 cells in vitro (Fig. 1E). Transwell migration assays demonstrated that significantly fewer hMSCs migrated toward conditioned media from U87-TGFβ-kd compared with U87 parental or U87 scramble cell lines (p<0.01, Fig. 1F). Addition of TGF-β1 to the conditioned media of U87-TGFβ-kd restored the migration of hMSCs back to pre-knock-down levels (p<0.05, Fig. 1F).
Finally, when recombinant latent TGF-β1 itself was place in the lower wells of transwell assays, significantly more BM-hMSCs migrated through matrigel compared with media alone, and TGF-β1 attracted BM-hMSCs in a dose dependent manner (Supplementary Fig. S1), further supporting a role of TGF-β in BM-hMSC migration.
In order to determine whether in vitro results also occurred in vivo, intracranial xenografts of U87 parental (N=3), U87 scramble (N=3) or U87-TGFβ-kd (N=3) were established in the frontal lobes of nude mice and 7 days later gfp-labeled BM-hMSCs (BM-hMSCs-gfp) were injected into the carotid artery of tumor-bearing mice. Immunohistochemistry for TGF-β confirmed loss of TGF-β expression in the knockdown-U87 xenografts compared with controls in vivo (Fig. 1E). Qualitative assessments showed that large numbers of gfp-labeled BM-hMSCs homed to the U87-parental or U87-scramble xenografts, whereas few BM-hMSCs were seen within the TGF-β knock-down xenografts (Fig. 1G). Quantitative assessments based on counting the number of BM-hMSCs-gfp per area of tumor showed that the average number of BM-hMSCs in U87-TGFβ-kd xenografts (7.7±1.7cell/mm2) was significantly less than that of the U87-parental or U87-scramble xenografts (26.1±5.7cell/mm2, P<.05, Fig. 1H). Taken together, these studies indicate that TGF-β produced by the tumor causally contributes to the homing of BM-hMSCs to established glioma cell lines.
Tropic effect of TGF-β on BM-hMSCs is independent of vessel density or tumor size
Because TGF-β is known to promote tumor angiogenesis24,25 and possibly influence tumor growth, we explored whether the effects of TGF-β on BM-hMSC homing were a result of increases in the amount of vessels in the xenografts or increases in the size of the xenografts. Therefore, we determined the number of vessels per area tumor by staining with CD31 antibody, a known marker of endothelial cells, and we determined the tumor size by measuring the cross-sectional area on serial sections. There was no significant difference in the vessel densities between the U87-parental, U87 scrambled, and U87-TGFβ-kd xenografts (Fig. 1I & J). Likewise, there was no significant difference in the size of the U87-parental, U87 scrambled, and U87-TGFβ-kd xenografts (Fig. 1K) Therefore, the tropic effect of TGF-β on BM-hMSCs is independent of the vessel densities and tumor size. This result is supported by a previous report showing that TGF-β regulates coverage of pericytes rather than density of endothelial cells25.
The tropic effect of TGF-β on BM-hMSCs is mediated via TGF-β receptors and co-receptors expressed on BM-hMSCs
To assess whether the tropic effects of TGF-β were directly mediated by TGF-β receptors, which are known to be expressed on BM-hMSCs34,35, TGF-β type II receptor (TGFβRII) was stably knocked down in BM-hMSCs (BM-hMSCs-TGFβRII-kd) (Fig. 2A). We verified that knocking down the TGF-β receptor did not alter BM-hMSC viability by measuring the proliferation of the BM-hMSCs-TGFβRII-kd at days 4 and 7, and confirmed that there were no statistically significant differences in the growth of BM-hMSC-parental, BM-hMSC-scramble, and BM-hMSCs-TGFβRII-kd (Supplementary Fig. S2). We then tested the migration of BM-hMSCs-TGFβRII-kd in vitro using Transwell migration assays, and showed that knockdown of TGFβRII significantly reduced the migration of BM-hMSCs to conditioned media from U87 cells (p<.01, Fig. 2B).
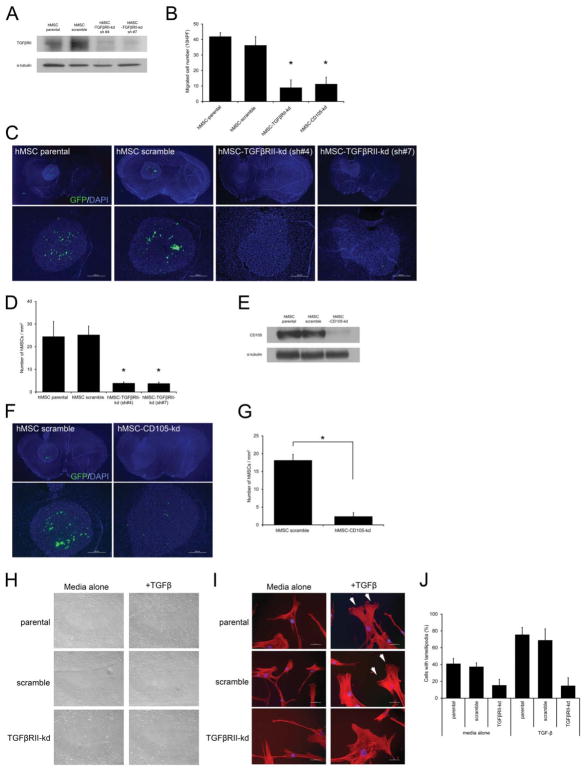
Figure 2.
TGFβ mediates the tropism of BM-hMSCs to gliomas through TGF-β receptors on BM-hMSCs
(A) and (E). Expression of TGFβIIR (A) or CD105 (E) in BM-hMSCs by western blots. α-tubulin is internal control.
(B) In vitro migration of BM-hMSCs in which TGF-β receptors were knocked down toward CM of U87. Error bars, SDs.
(C) Homing of GFP-labeled BM-hMSCs-TGFβRII-kd (two independent shRNAs, #4 and #7) to U87 tumor. The scale bars, 500μm.
(D) Quantitative assessments of homing of BM-hMSCs. Error bars, SEs.
(F) Homing of BM-hMSC-CD105-kd to U87 tumors. Scale bars, 500μm.
(G) Quantitative assessments of localization of BM-hMSCs. Error bars, SEs.
(H) (I) (J) Lamellipodia formation was examined in BM-hMSCs-parental, -scramble, and -TGFβRII-kd with or without TGF-β. (H) Representative pictures of cells at scratch sites at 10x of magnification. (I) Representative pictures of cells at the edge of the scratch. Scale bars, 50μm. Arrows, lamellipodia. (J) Quantitative assessments of cell with lamellipodia. Error bars, SDs.
To analyze the effects of knocking down TGF-β receptor II in BM-hMSCs in vivo, BM-hMSCs-parental, BM-hMSCs-scrambled, or BM-hMSCs-TGFβRII-kd were injected into carotid arteries of mice harboring 7-day old U87 gliomas (N=6 mice/group). There was a clear decrease in the homing of the BM-hMSCs-TGFβRII-kd compared with the BM-hMSCs-parental or BM-hMSCs-scrambled (Fig. 2C). The same result was seen for two independent knock-down constructs, sh#4 and #7 (Fig. 2C). Quantification of the results showed a statistically significant decrease in intratumoral localization when the TGF-β receptor II was knocked down in the BM-hMSCs [3.9 ± 0.6 (sh#4) and 3.8 ± 0.6 (sh#7) compared with BM-hMSC-parental (24.5± 6.7 cells/mm2) or BM-hMSCs-scramble (25.2± 3.9 cells/mm2, p<.01, Fig. 2D].
To further assess the tropic effects of TGF-β, the co-receptor of the TGF-β receptor, CD105 (i.e., Endoglin), which is a well-known marker for BM-hMSC, was stably knocked down in BM-hMSCs (generating BM-hMSCs-CD105-kd) (Fig. 2E). There was no significant difference in proliferation between BM-hMSCs-parental, BM-hMSC-scramble, or BM-hMSCs-CD105-kd (Supplementary Fig. S2). In vitro transwell migration assays showed that the knocking down CD105 in BM-hMSCs significantly abrogated the migration of BM-hMSCs toward conditioned media from U87 (p<.01, Fig. 2B).
To test the role of CD105 in the localization of BM-hMSCs for gliomas in vivo, BM-hMSCs-scrambled or BM-hMSCs-CD105-kd were injected into carotid artery of 7-day old U87 brain tumor bearing mice (N= 3 mice/ group). Qualitative analyses showed that whereas large numbers of BM-hMSCs-scrambled localized to U87 tumors, BM-hMSCs-CD105-kd showed a drastic reduction in homing to U87 xenografts (Fig. 2F). Quantification of the result confirmed that knocking down CD105 significantly inhibited the localization of BM-hMSCs to U87 xenografts in vivo (18.1±1.7 cells/mm2 for BM-hMSCs-scramble versus. 2.4±1.1 cells/mm2 for BM-hMSC-CD105-kd, p<.01, Fig. 2G).
TGF-β enhances lamellipodia formation in BM-hMSCs
Actin-fiber formations, such as lamellipodia protrusions, are required for cell migration36,37. Therefore, we examined whether TGF-β enhances the formation of lamellipodia protrusions on BM-hMSCs as a possible mechanism for the increased migration of BM-hMSCs after exposure to TGF-β. Compared with media alone, treatment of BM-hMSCs with TGF-β significantly increased the number of cells expressing lamellipodia at the migrating edge of the scratch (Fig. 2H–J). In addition, when TGFβRII was knocked down in BM-hMSCs, there was no increase in lamellipodia after treatment with TGF-β (Fig. 2I & J). Of note, is that there was a decrease in lamellipodia formation in BM-hMSCs-TGFβRII-kd at base line, consistent with the autocrine secretion of TGF-β by BM-hMSCs35,38. Together, these results indicate that the tropic effects of TGF-β on BM-hMSCs are mediated at least in part by the augmentation of lamellipodia protrusions in BM-hMSCs.
TGF-β mediates homing of hMSCs to GSCs derived from C6 gliomas
Given the contribution of TGF-β to the homing of BM-hMSCs to U87 gliomas, we were interested in whether TGF-β also mediated the homing of BM-hMSCs to GSCs. Setoguchi et al. recently reported the isolation of GSCs from the C6 glioma cell line. Consequently, we obtained two C6 GSC clones26,27 which grew as neurospheres in culture and formed intracranial tumors in nude mice. Interestingly, we found that one clone expressed low levels of TGF-β (called GSC001low) whereas the other expressed high levels of TGF-β (called GSC001high) (Fig. 3A). Assaying STR polymorphisms in these lines showed that the GSC001low and GSC001high clones are isogenic (Supplementary Fig. S3 and Supplementary Table S1). To test the extent to which BM-hMSCs were capable of homing to these GSCs, GSC001low or GSC001high were injected into the frontal lobes of nude mice. After 21 days when xenografts were established, gfp-labled BM-hMSCs were injected into the carotid artery of tumor bearing mice. Immunohistochemistry confirmed that TGF-β was not detectable in GSC001low xenografts, whereas TGF-β was readily seen in GSC001high xenografts (Fig. 3A). Qualitative analyses revealed that BM-hMSCs localized to GSC001high xenografts, whereas no BM-hMSCs were found in GSC001low xenografts (Fig. 3B). These results suggested that TGF-β was necessary for BM-hMSCs to localize to C6 GSCs in vivo.
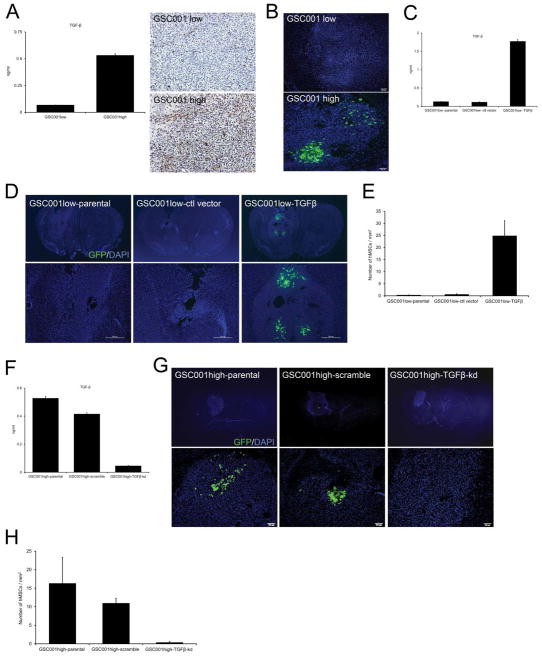
Figure 3.
TGF-β mediates homing of BM-hMSCs to isogenic GSCs from C6 gliomas.
(A) The amount of TGF-β in the conditioned media of GSC001low and GSC001high cells by ELISA (left). Error bars, SDs. Immunohistochemistry of TGF-β in GSC001low and GSC001high brain tumors (right). Scale bars, 50μm.
(B) Homing of BM-hMSCs-GFP to GSC001low (Scale bar, 200 μm) and GSC001high brain xenografts (Scale bar, 100 μm).
(C) Amounts of TGF-β in CM of GSC001low-parental, GSC001low-control vector, or GSC001low-TGFβ cells by ELISA. Error bars, SDs.
(D) The homing of BM-hMSCs-GFP to brain xenografts of GSC001low-parental (left), GSC001low-control vector (middle) or GSC001low-TGFβ (right). Scale bars, 500μm.
(E) Quantitative assessments of homing of BM-hMSCs. Error bars, SEs.
(F) Amounts of TGF-β in the conditioned media of GSC001high-parental or GSC001high-scramble, or GSC001high-TGFβ-kd cells by ELISA. Error bars, SDs.
(G)Homing of BM-hMSCs-GFP to brain xenografts of GSC001high-parental (left), GSC001high-scramble (middle) or GSC001high-TGFβ-kd (right). Scale bars, 100μm.
(H) Quantitative assessments of homing of BM-hMSCs. Error bars, SEs.
To verify the importance of TGF-β in BM-hMSC homing to C6 GSCs, we stably overexpressed TGF-β in GSC001low using lentivirus technology (called GSC001low-TGFβ). ELISA and immunohistochemistry confirmed that GSC001low-TGFβ produced high levels of TGF-β compared with GSC001low-parental, or GSC001low-vector (Fig. 3C and Supplementary Fig. S4A). Intracranial xenografts of GSC001low-parental (N=3), GSC001low-vector (N=3) or GSC001low-TGFβ (N=3) were established in the frontal lobes of nude mice, and gfp-labeled BM-hMSCs were injected into the carotid artery of mice bearing 7-day old xenografts. After 3 days the brains were harvested and analyzed for the presence of BM-hMSCs. Qualitatively, many BM-hMSCs localized to the GSC001low-TGFβ tumors which produce high levels of TGF-β, whereas almost no MSCs were seen in controls (Fig. 3D and Supplementary Fig. S4A). Quantitative assessments showed that the average number of BM-hMSCs in GSC001low-TGFβ tumors (24.8±6.3 cell/mm2)was significantly higher than that of the GSC001low-parental xenografts, or GSC001low-vector xenografts (0.57±0.24 cell/mm2, P<.05, Fig. 3E).
Next TGF-β was stably knocked down in GSC001high cells (generating GSC001high-TGFβ-kd). ELISA and immunohistochemistry confirmed successful reduction in TGF-β production by GSC001high-TGFβ-kd compared with controls in vitro and in vivo, respectively (Fig. 3F and Supplementary Fig. S4B). We then examined the extent to which hMSCs localize to GSC001high-TGFβ-kd tumors. After injection into the carotid artery, gfp-labeled BM-hMSCs showed significant reduction in their ability to localized to intracranial xenografts of GSC001high-TGFβ-kd (N=3), compared with GSC001high-parental (N=3) and GSC001high-scramble (N=3), (Fig. 3G). Quantitative analyses verified these results with significantly fewer BM-hMSCs localizing to GSC001high-TGFβ-kd tumors (0.35±0.22 cell/mm2) than the GSC001high-scramble tumors (11.0±1.3 cell/mm2; P<.01, Fig. 3G & H, and Supplementary Fig. S4B).
As in our previous experiments, there was no significant difference in the vessel densities between the GSC001low-control and GSC001low-TGFβ tumors or between GSC001high-scramble and GSC001high-TGFβ-kd tumors at the time of BM-hMSC injection (Supplementary Fig. S5A and S5B). These results demonstrated that TGF-β plays a causal role in homing of hMSCs to C6 GSCs.
TGF-β mediates homing of hMSCs to human GSCs derived from patient specimens
The results form C6 GSCs, led us to ask whether TGF-β also mediates the homing of BM-hMSCs to human GSCs, derived from patients with human gliomas. However, a review of the literature revealed that up to now no study has addressed the more basic question of whether intravascularly delivered BM-hMSCs are capable of homing to human GSC xenografts. Consequently, using the methods of Singh et al.10, we first established a group of five GSC lines, derived directly from fresh human surgical specimens of patients with malignant gliomas (Table 1). These lines grew as non-adherent spheroids in culture (Supplementary Fig. S6) and formed invasive tumors when implanted as xenografts in the brains of nude mice, although GSC17 showed only moderate invasive features (Fig. 4A–J). Consistent with other reports, CD133, a known marker of human GSCs, was expressed in some, but not all the lines (Table 1)10,11. To determine whether human-GSC xenografts could attract BM-hMSCs, xenografts of GSC11, GSC17, GSC 229, GSC268 or GSC274 were established in the frontal lobes of nude mice, and gfp-labeled BM-hMSCs were injected into the carotid artery of tumor-bearing mice. After 4 days brains were removed and examined by fluorescent microscopy for BM-hMSCs. As shown in Figure 4K–M, BM-hMSCs were capable of homing to xenografts of GSC17, GSC268, and GSC274. However, BM-hMSCs were not observed in xenografts from GSC11 and GSC229 (Fig. 4N–O). Therefore, there was heterogeneity in the capacity of BM-hMSCs to target GSCs in vivo.
Table 1.
Characteristics of GSCs from human surgical specimens
| Cell Line | CD133 expression (%) | Histology | Animal mean survival (days ± SD) |
|---|---|---|---|
| GSC268 | 9.0 | GBM | 101±23.7 |
| GSC17 | 0.0 | GBM | 21.6±2.9 |
| GSC274 | 47.0 | GBM | 62.8±6.1 |
| GSC11 | 40.0 | GBM | 64.1±5.3 |
| GSC229 | 10.0 | GBM | 65.4±3.5 |
GBM, glioblastoma multiforme
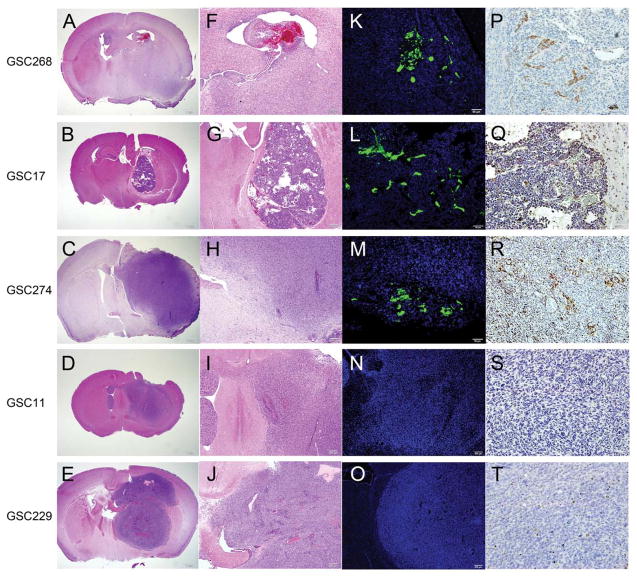
Figure 4.
TGF-β mediates homing of BM-hMSCs to GSCs. A–E, Brain xenografts of GSCs (GSC268, GSC17, GSC274, GSC11, GSC229) after H&E staining (scale bars, 1mm); F – J, high power views of tumor (scale bars, 200 μm). K–M Homing of BM-hMSCs-GFP to different GSC tumors (scale bars for K, L, M, 50 μm and for N, O scale bars, 200 μm). P–T Immunohistochemistry of TGF-β (scale bars, 50 μm).
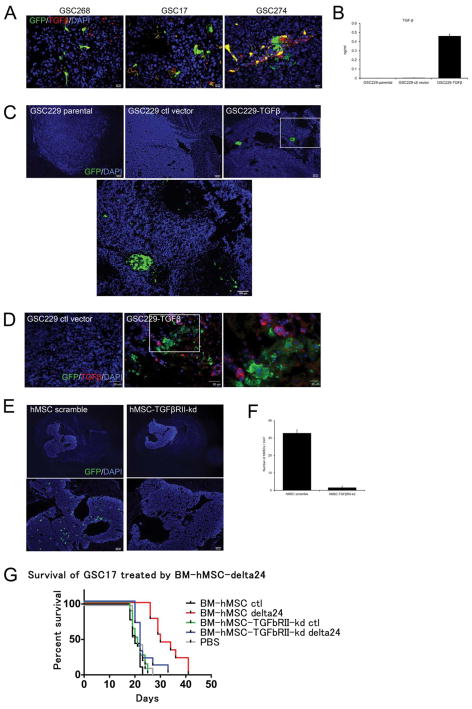
Given these differences in the ability of BM-hMSCs to home to GSCs, we asked whether there was a correlation between TGF-β expression and BM-hMSC homing in our 5 GSC xenografts. Interestingly, immunohistochemical staining for TGF-β demonstrated that all three GSC xenografts that attracted BM-hMSCs (GSC17, GSC268, GSC274) expressed high levels of TGF-β (Fig. 4P–R), whereas TGF-β was not detectable in the two GSC tumors (GSC11 and GSC229) that did not attract BM-hMSCs (Fig. 4S–T). Therefore, there was a direct correlation between the expression of TGF-β in the GSCs and the ability of BM-hMSCs to home to the GSCs. In addition, we noted that BM-hMSCs localized in clusters within GSCs rather than diffusely throughout the tumor. Indeed, simultaneous double immunofluorescent staining for BM-hMSCs-GFP and for TGF-β, revealed that BM-hMSCs localized specifically within the vicinity of cells expressing high levels of TGF-β in GSC 268, GSC17, and GSC274 tumors, and were less clustered in areas of the tumor that lacked TGF-β expression (Fig. 5A), further supporting the contribution of TGF-β to the homing of BM-hMSCs.
Figure 5.
BM-hMSCs localize in close proximity to cells expressing high level of TGF-β in human GSC brain xenografts.
(A)Double staining of GFP and TGF-β to detect BM-hMSCs-GFP and the tumor cells expressing TGF-β in GSC xenografts. The green colored cells are BM-hMSCs-GFP, red colored cells are the cells expressing TGF-β. Small yellow colored dots are red blood cells by autofluorescence. Some of green MSCs manifesting yellow color in them, indicating TGF-β expression in MSCs. The scale bars, 20 μm.
(B)The amounts of TGF-β in the CM of parental, control vector or TGF-β1 over-expressing GSC229 by ELISA. Error bars, SDs.
(C)Homing of BM-hMSCs-GFP to brain xenografts of GSC229-parental (upper left), GSC229-control vector (upper middle) or GSC229-TGFβ (upper right), scale bars, 200μm. Lower panel shows the box in picture of GSC229-TGFβ. Scale bar, 100 μm.
(D)Double staining of GFP and TGF-β to detect BM-hMSCs-GFP and tumor cells expressing TGF-β in brain tumors of GSC229-control vector (left), GSC229-TGFβ (middle), scale bars, 50 μm. Right panel showing the box in middle panel, scale bar, 20 μm.
(E)Homing of BM-hMSCs-GFP to brain xenografts of GSC17 with or without knockdown of TGFβRII in BM-hMSCs, BM-hMSC- scramble (left), BM-hMSC-TGFβRII-kd (right). scale bars, 200μm.
(F)Quantitative assessments of homing of BM-hMSCs. Error bars, SEs.
(G) Kaplan-Meier survival curve shows that BM-hMSCs-Delta24 prolong survival of brain xenografts of GSCs expressing high level of TGF-β.
To establish a causal role of TGF-β in BM-hMSC homing to GSCs, we tested the extent to which BM-hMSCs localize to GSC229 in which we stably over-expressed TGF-β (generating GSC229-TGFβ), thereby converting a GSC that does not produce TGF-β into one that does. ELISA confirmed that GSC229-TGFβ secreted higher levels of TGF-β compared with GSC229-parental or GSC229-ctl vector. Intracranial xenografts of GSC229-parental (N=3), GSC229-ctl-vector (N=3) or GSC229-TGFβ (N=3) were established in the frontal lobes of nude mice, and BM-hMSCs-GFP were injected into the carotid artery of mice bearing 6-week old tumors. After 3 days the brains were harvested and analyzed for the presence of labeled hMSCs. Whereas GSC229-parental and GSC229-ctl vector remained unable to attract BM-hMSCs, BM-hMSCs localized to the GSC229-TGFβ tumors in two of three mice, albeit in a clustering pattern (Fig. 5C). Importantly, simultaneous double immunofluorescent staining for BM-hMSCs-GFP and for TGF-β, revealed that BM-hMSCs localized specifically within the vicinity of cells expressing high levels of TGF-β in GSC229-TGFβ tumors, and were less clustered in areas of the tumor that expressed low level of TGF-β (Fig. 5D). Importantly, there was no difference in the size of the GSC229-TGFβ xenografts compared with the GSC229-parental and GSC229-ctl vector tumors (Supplemental Fig. S5C)
To further define the role of TGF-β in the homing of BM-hMSC to GSCs, we tested the ability of BM-hMSC in which TGFβ receptor II was knocked down (BM-hMSCs-TGFβRII-kd) to localize to GSCs. Specifically, BM-hMSCs-scramble or BM-hMSCs-TGFβRII-kd were injected into carotid artery of mice bearing GSC17 xenografts (N=3 mice/group). By both qualitative (Fig. 5E) and quantitative (Fig. 5F) assessments, the homing of hMSCs-TGFβRII-kd was significantly less than the homing of the BM-hMSCs-scrambled [32.8 ± 1.9 (scramble) vs. 1.6 ± 0.9 (TGFβRII-kd) cells/mm2, p<.01].
Finally, we tested whether intravascular administration of BM-hMSCs is a clinically applicable approach for therapeutic delivery to GSCs expressing high TGF-β. We have previously shown that BM-hMSCs can be loaded with the oncolytic adenoviruses, Delta-24-RGD, and that these BM-hMSCs are capable of delivering this virus to intracranial U87 xengrafts4. Consequently, we sought to determine whether BM-hMSCs carrying Delta-24-RGD would be efficacious against GSCs and whether the therapeutic effects would depend on TGFβRII expression on BM-hMSCs. Specifically, GSC17 was implanted into the frontal lobes of nude mice. BM-hMSCs that had been infected with Delta-24-RGD (BM-hMSC-Delta24) or BM-hMSCs (control) were injected intra-arterially into the mice. Survival analysis showed that BM-hMSCs delivering the oncolytic adenoviruses significantly prolonged the survival of mice. To show that the therapeutic effects required TGFβRII on BM-hMSCs, in the same experiment animals were treated with intra-arterial injections of BM-hMSCs-TGFβRII-kd or with BM-hMSCs-TGFβRII-kd-Delta24. As expected, there was no difference in survival between BM-hMSCs-TGFβRII-kd and BM-hMSCs-TGFβRII-kd-Delta24 or with BM-hMSC control, indicating that TGFβRII is important for mediating the localization of BM-hMSCs to tumors in this therapeutic approach (Fig. 5G).
Discussion
The mechanism underlying the homing of BM-hMSCs to solid tumors, particularly gliomas, has not been fully elucidated. We now show that TGF-β mediates the homing of BM-hMSCs to gliomas based on studies of three different glioma models: established glioma cell lines (U87, U251, LN229), isogenic GSCs from C6 gliomas, and human GSCs from patients. In both in vitro and in vivo studies, down-regulation or blocking TGF-β abrogated the ability of BM-hMSCs to localize to gliomas, and up-regulation of TGF-β enhanced BM-hMSC homing, suggesting that TGF-β is necessary for BM-hMSC homing in all these models. In addition, knock-down studies indicate that the tropic effects of TGF-β are mediated directly through TGF-βRII and its co-receptor, CD105, which is an identifying surface marker of hMSCs.
TGF-β has been implicated in many tumor-related functions including proliferation and anti-apoptosis39, angiogenesis24,25, maintenance of stemness21,23, and immunosuppression40. However, its role as a tropic factor for BM-hMSCs in vivo in tumors has not been examined in detail up to now. In a diaphyseal dysplasia mouse model, Tang et al. demonstrated that TGF-β induces migration of mouse BM-MSCs in vitro and in vivo, and that the migration of BM-MSCs is important for coupling bone resorption with bone formation41, providing the first evidence that TGF-β may enhance BM-MSC migration in vivo. With regards to tumors, several in vitro studies have shown that tumor-derived TGF-β enhances the migrate of BM-MSCs in invasion assays8,42; however, none of these reports evaluated TGF-β using in vivo tumor models and none linked TGF-β to GSCs. By examining TGF-β expression in three model systems, we correlated TGF-β expression with the ability of the tumor to attract BM-hMSCs. Likewise, forced increases in TGF-β production enhanced BM-hMSC homing, and conversely, forced inhibition of TGF-β abrogated BM-hMSC homing in vitro and especially in vivo in each of these model systems. Taken together, these experiments reveal TGF-β as a major contributor to the ability of BM-hMSC to home to gliomas.
Up to now it has been unclear whether BM-hMSCs home to patient-derived human GSCs15,16. Targeting human GSCs is a laudable goal because GSCs are resistant to most therapies, and are responsible for the poor outcome of patients with gliomas10–14. Our results provide the first definitive evidence that BM-hMSCs are capable of homing to human GSC xenografts after intravascular delivery. Importantly, and consistent with the findings in U87, U251 and C6 GSCs, of the five human GSC models tested, three expressed TGF-β in vivo based on immunohistochemical staining of GSC xenografts for TGF-β, and only these 3 lines were capable of supporting the homing of BM-hMSCs after intravascular delivery. These results suggest that TGF-β expression level can identify those GSC xenografts that will attract BM-hMSCs. Interestingly, the commercial cell lines (U87) tended to express TGF-β diffusely throughout the tumor, whereas TGF-β was expressed more focally in GSC xenografts. Consistent with these patterns, BM-hMSCs were distributed diffusely in U87 xenografts, whereas they tended to cluster around foci of high TGF-β in GSC xenografts, as confirmed by double immunofluorescent staining for BM-hMSCs and TGF-β. This clustering was also evident in GSC229-TGF-β in which TGF-β was up-regulated by stable transfection. Although high levels of TGF-β were detected in vitro in this transduced cell line, the expression of TGF-β was focal in the in vivo xenografts and the BM-hMSCs tended to cluster around these foci. Because recent work has suggested that TGF-β is important for maintaining GSC stemness21,23; we speculate that the focal areas of TGF-β in these xenografts may represent the cells in the heterogenous xenograft that retained their self-renewal capacity, i.e., the undifferentiated GSCs. Therefore, because BM-hMSCs migrate toward TGF-β, which may be expressed primarily by the GSCs, we further speculate that BM-hMSCs may be capable of homing to and delivering therapeutic agents specifically to GSCs that drive tumorigenesis and reside in focal niches within the larger tumor mass21,23. In this context, we showed that BM-hMSCs are capable of targeting and delivering therapeutic agents against GSC-xenografts. As a proof-of-principle we loaded the BM-hMSCs with the oncolytic adenovirus, Delta-24-RGD4, and showed that these therapeutic BM-hMSCs are able to prolong the survival of mice harboring GSC-derived xenografts. Clearly, BM-hMSCs can be loaded with other anti-GSC agents, including secretable proteins5 that specifically interfere with GSC function.
The finding that human GSCs attract BM-hMSCs with different affinities suggests that there may be heterogeneity in the ability of BM-hMSCs to home to patient tumors. Therefore, TGF-β expression may be a useful bio-marker for predicting whether BM-hMSCs will home to gliomas in individual patients. The concept that delivery systems may be more or less effective in different patients represents a new paradigm in stem cell delivery because up to now it has generally been assumed that all gliomas attract BM-hMSCs equally. It is logical to assume that other cell based delivery systems, e.g., neural stem cells, inducible pluripotent stem cells, or embryonic stem cells, may also depend upon specific tumor milieus to support their homing to particular tumors15. To our knowledge this variability has not been explored in these other cell types.
Zhang et al. suggested that that TGF-β mediates recruitment of BM-MSCs indirectly through MCP-1 production in vascular smooth muscle cells43. In contrast, we found that TGF-β acts directly on BM-hMSCs via TGFβRII or CD105. Consistent with this direct effect, we found that TGF-β enhanced lamellipodia formation on BM-hMSCs and that this increase could be attenuated by knocking down TGFβRII. It is well-known that actin-fiber formations, e.g., lamellipodia, are required for cell migration36,37. Consistent with our data, Tang et al. recently found that MSC migration was caused by up-regulation of lamellipodia regulated by TGF-β/Smad pathway41. Alternatively, Rho-GTPases of the Rac/Cdc42 or Rif subfamilies are known to contribute to actin polymerization in lamellipodia37,44. Because TGF-β has been shown to activate the RhoA/p160ROCK pathway via Smad-independent signaling45, TGF-β may regulate lamellipodia in BM-hMSCs through the RhoA/p160ROCK pathway. Also consistent with a direct effect of TGF-β on BM-hMSCs, we found that overexpression or knocked down of TGF-β did not alter vessel density, suggesting that the effects of TGF-β on BM-hMSC homing were not indirectly related to angiogenesis. Taken together, our data suggest that in addition to the indirect pathways identified by Zhang et al.43, TGF-β directly mediates the tropism of BM-MSCs. Therefore, it may be possible to enhance BM-hMSC migration by up-regulation of TGFβRII, leading to increased sensitivity of BM-hMSCs to low levels of TGF-β in gliomas.
We previously reported that platelet derived growth factor-B (PDGFB) may also mediate the homing of BM-hMSCs toward gliomas6. Although our previous studies did not specifically assess the role of PDGF-BB in GSCs, in the context of the current study on TGF-β, they suggest that multiple factors may be capable of mediating the homing of BM-hMSCs to gliomas. Indeed, the relative contribution of PDGF-BB and TGF-β, as well as other factors7,8,46, to BM-hMSC migration toward gliomas remains to be determined. Whether these factors function independently and provide biological redundancy, or whether they act in concert, attracting BM-hMSCs to different tumor components, has not been determined. Lastly, it remains unclear whether TGF-β also drives the tropism of BM-hMSCs for tumors other than gliomas.
Supplementary Material
Acknowledgments
We thank Stephanie Jenkins for her assistance with preparation of the manuscript. We thank Dr. Hideyo Yasuda at Department of Genomics, The University of Texas M. D. Anderson Cancer Center, for his technical support of STR polymorphism assay.
Grant Support
This study was supported by grants from the National Cancer Institute CA115729 and 1P50 CA127001, The Ben and Cathy Ivy Foundation, The Broach Foundation for Brain Cancer Research, MD Anderson Center for Targeted Therapy, The National Brain Tumor Foundation, The Collaborative Ependymoma Research Network (CERN), The Elias Family Fund, The Gene Pennebaker Brain Cancer Fund, the Sorenson Foundation, and the Brian McCulloch Fund to F.F.L.
Footnotes
Conflict of Interest: The authors do not have any conflicts of interest to disclose.
References
- 1.Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987–996. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 2.Pardridge WM. Blood-brain barrier drug targeting: The future of brain drug development. Mol Interv. 2003;3:90–105. 151. doi: 10.1124/mi.3.2.90. [DOI] [PubMed] [Google Scholar]
- 3.Decleves X, Amiel A, Delattre JY, Scherrmann JM. Role of abc transporters in the chemoresistance of human gliomas. Curr Cancer Drug Targets. 2006;6:433–445. doi: 10.2174/156800906777723930. [DOI] [PubMed] [Google Scholar]
- 4.Yong RL, Shinojima N, Fueyo J, Gumin J, Vecil GG, Marini FC, et al. Human bone marrow-derived mesenchymal stem cells for intravascular delivery of oncolytic adenovirus delta24-rgd to human gliomas. Cancer Res. 2009;69:8932–8940. doi: 10.1158/0008-5472.CAN-08-3873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nakamizo A, Marini F, Amano T, Khan A, Studeny M, Gumin J, et al. Human bone marrow-derived mesenchymal stem cells in the treatment of gliomas. Cancer Res. 2005;65:3307–3318. doi: 10.1158/0008-5472.CAN-04-1874. [DOI] [PubMed] [Google Scholar]
- 6.Hata N, Shinojima N, Gumin J, Yong R, Marini F, Andreeff M, et al. Platelet-derived growth factor bb mediates the tropism of human mesenchymal stem cells for malignant gliomas. Neurosurgery. 2010;66:144–156. doi: 10.1227/01.NEU.0000363149.58885.2E. discussion 156–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dwyer RM, Potter-Beirne SM, Harrington KA, Lowery AJ, Hennessy E, Murphy JM, et al. Monocyte chemotactic protein-1 secreted by primary breast tumors stimulates migration of mesenchymal stem cells. Clin Cancer Res. 2007;13:5020–5027. doi: 10.1158/1078-0432.CCR-07-0731. [DOI] [PubMed] [Google Scholar]
- 8.Birnbaum T, Roider J, Schankin CJ, Padovan CS, Schichor C, Goldbrunner R, et al. Malignant gliomas actively recruit bone marrow stromal cells by secreting angiogenic cytokines. J Neurooncol. 2007;83:241–247. doi: 10.1007/s11060-007-9332-4. [DOI] [PubMed] [Google Scholar]
- 9.Doucette T, Rao G, Yang Y, Gumin J, Shinojima N, Bekele BN, et al. Mesenchymal stem cells display tumor-specific tropism in an rcas/ntv-a glioma model. Neoplasia. 2011;13:716–725. doi: 10.1593/neo.101680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh SK, Hawkins C, Clarke ID, Squire JA, Bayani J, Hide T, et al. Identification of human brain tumour initiating cells. Nature. 2004;432:396–401. doi: 10.1038/nature03128. [DOI] [PubMed] [Google Scholar]
- 11.Chen R, Nishimura MC, Bumbaca SM, Kharbanda S, Forrest WF, Kasman IM, et al. A hierarchy of self-renewing tumor-initiating cell types in glioblastoma. Cancer Cell. 2010;17:362–375. doi: 10.1016/j.ccr.2009.12.049. [DOI] [PubMed] [Google Scholar]
- 12.Dean M, Fojo T, Bates S. Tumour stem cells and drug resistance. Nat Rev Cancer. 2005;5:275–284. doi: 10.1038/nrc1590. [DOI] [PubMed] [Google Scholar]
- 13.Takebe N, Harris PJ, Warren RQ, Ivy SP. Targeting cancer stem cells by inhibiting wnt, notch, and hedgehog pathways. Nat Rev Clin Oncol. 2011;8:97–106. doi: 10.1038/nrclinonc.2010.196. [DOI] [PubMed] [Google Scholar]
- 14.Maitland NJ, Collins AT. Cancer stem cells - a therapeutic target? Curr Opin Mol Ther. 2010;12:662–673. [PubMed] [Google Scholar]
- 15.Binello E, Germano IM. Stem cells as therapeutic vehicles for the treatment of high-grade gliomas. Neuro Oncol. 2011 doi: 10.1093/neuonc/nor204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oh MC, Lim DA. Novel treatment strategies for malignant gliomas using neural stem cells. Neurotherapeutics. 2009;6:458–464. doi: 10.1016/j.nurt.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pohlers D, Brenmoehl J, Loffler I, Muller CK, Leipner C, Schultze-Mosgau S, et al. Tgf-beta and fibrosis in different organs - molecular pathway imprints. Biochimica et biophysica acta. 2009;1792:746–756. doi: 10.1016/j.bbadis.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 18.Dvorak HF. Tumors: Wounds that do not heal. Similarities between tumor stroma generation and wound healing. The New England journal of medicine. 1986;315:1650–1659. doi: 10.1056/NEJM198612253152606. [DOI] [PubMed] [Google Scholar]
- 19.Schneider T, Sailer M, Ansorge S, Firsching R, Reinhold D. Increased concentrations of transforming growth factor beta1 and beta2 in the plasma of patients with glioblastoma. J Neurooncol. 2006;79:61–65. doi: 10.1007/s11060-005-9116-7. [DOI] [PubMed] [Google Scholar]
- 20.Bruna A, Darken RS, Rojo F, Ocana A, Penuelas S, Arias A, et al. High tgfbeta-smad activity confers poor prognosis in glioma patients and promotes cell proliferation depending on the methylation of the pdgf-b gene. Cancer Cell. 2007;11:147–160. doi: 10.1016/j.ccr.2006.11.023. [DOI] [PubMed] [Google Scholar]
- 21.Ikushima H, Todo T, Ino Y, Takahashi M, Miyazawa K, Miyazono K. Autocrine tgf-beta signaling maintains tumorigenicity of glioma-initiating cells through sry-related hmg-box factors. Cell Stem Cell. 2009;5:504–514. doi: 10.1016/j.stem.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 22.Strege RJ, Godt C, Stark AM, Hugo HH, Mehdorn HM. Protein expression of fas, fas ligand, bcl-2 and tgfbeta2 and correlation with survival in initial and recurrent human gliomas. J Neurooncol. 2004;67:29–39. doi: 10.1023/b:neon.0000021739.34343.75. [DOI] [PubMed] [Google Scholar]
- 23.Penuelas S, Anido J, Prieto-Sanchez RM, Folch G, Barba I, Cuartas I, et al. Tgf-beta increases glioma-initiating cell self-renewal through the induction of lif in human glioblastoma. Cancer Cell. 2009;15:315–327. doi: 10.1016/j.ccr.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 24.Carmeliet P, Jain RK. Molecular mechanisms and clinical applications of angiogenesis. Nature. 2011;473:298–307. doi: 10.1038/nature10144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kano MR, Bae Y, Iwata C, Morishita Y, Yashiro M, Oka M, et al. Improvement of cancer-targeting therapy, using nanocarriers for intractable solid tumors by inhibition of tgf-beta signaling. Proc Natl Acad Sci U S A. 2007;104:3460–3465. doi: 10.1073/pnas.0611660104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Setoguchi T, Taga T, Kondo T. Cancer stem cells persist in many cancer cell lines. Cell Cycle. 2004;3:414–415. doi: 10.4161/cc.3.4.799. [DOI] [PubMed] [Google Scholar]
- 27.Kondo T, Setoguchi T, Taga T. Persistence of a small subpopulation of cancer stem-like cells in the c6 glioma cell line. Proc Natl Acad Sci U S A. 2004;101:781–786. doi: 10.1073/pnas.0307618100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tiscornia G, Singer O, Verma IM. Production and purification of lentiviral vectors. Nature protocols. 2006;1:241–245. doi: 10.1038/nprot.2006.37. [DOI] [PubMed] [Google Scholar]
- 29.Oh CD, Maity SN, Lu JF, Zhang J, Liang S, Coustry F, et al. Identification of sox9 interaction sites in the genome of chondrocytes. PLoS One. 2010;5:e10113. doi: 10.1371/journal.pone.0010113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walder RY, Garrett MR, McClain AM, Beck GE, Brennan TM, Kramer NA, et al. Short tandem repeat polymorphic markers for the rat genome from marker-selected libraries. Mamm Genome. 1998;9:1013–1021. doi: 10.1007/s003359900917. [DOI] [PubMed] [Google Scholar]
- 31.Masek T, Vopalensky V, Suchomelova P, Pospisek M. Denaturing rna electrophoresis in tae agarose gels. Anal Biochem. 2005;336:46–50. doi: 10.1016/j.ab.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 32.Wakefield LM, Winokur TS, Hollands RS, Christopherson K, Levinson AD, Sporn MB. Recombinant latent transforming growth factor beta 1 has a longer plasma half-life in rats than active transforming growth factor beta 1, and a different tissue distribution. J Clin Invest. 1990;86:1976–1984. doi: 10.1172/JCI114932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Olmsted-Davis EA, Gugala Z, Gannon FH, Yotnda P, McAlhany RE, Lindsey RW, et al. Use of a chimeric adenovirus vector enhances bmp2 production and bone formation. Hum Gene Ther. 2002;13:1337–1347. doi: 10.1089/104303402760128568. [DOI] [PubMed] [Google Scholar]
- 34.Kollar K, Cook MM, Atkinson K, Brooke G. Molecular mechanisms involved in mesenchymal stem cell migration to the site of acute myocardial infarction. Int J Cell Biol. 2009;2009:904682. doi: 10.1155/2009/904682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kode JA, Mukherjee S, Joglekar MV, Hardikar AA. Mesenchymal stem cells: Immunobiology and role in immunomodulation and tissue regeneration. Cytotherapy. 2009;11:377–391. doi: 10.1080/14653240903080367. [DOI] [PubMed] [Google Scholar]
- 36.Giannone G, Dubin-Thaler BJ, Rossier O, Cai Y, Chaga O, Jiang G, et al. Lamellipodial actin mechanically links myosin activity with adhesion-site formation. Cell. 2007;128:561–575. doi: 10.1016/j.cell.2006.12.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ladwein M, Rottner K. On the rho’d: The regulation of membrane protrusions by rho-gtpases. FEBS Lett. 2008;582:2066–2074. doi: 10.1016/j.febslet.2008.04.033. [DOI] [PubMed] [Google Scholar]
- 38.Menicanin D, Bartold PM, Zannettino AC, Gronthos S. Genomic profiling of mesenchymal stem cells. Stem Cell Rev. 2009;5:36–50. doi: 10.1007/s12015-009-9056-2. [DOI] [PubMed] [Google Scholar]
- 39.Bierie B, Moses HL. Tumour microenvironment: Tgfbeta: The molecular jekyll and hyde of cancer. Nat Rev Cancer. 2006;6:506–520. doi: 10.1038/nrc1926. [DOI] [PubMed] [Google Scholar]
- 40.Gorelik L, Flavell RA. Immune-mediated eradication of tumors through the blockade of transforming growth factor-beta signaling in t cells. Nat Med. 2001;7:1118–1122. doi: 10.1038/nm1001-1118. [DOI] [PubMed] [Google Scholar]
- 41.Tang Y, Wu X, Lei W, Pang L, Wan C, Shi Z, et al. Tgf-beta1-induced migration of bone mesenchymal stem cells couples bone resorption with formation. Nat Med. 2009;15:757–765. doi: 10.1038/nm.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Goldstein RH, Reagan MR, Anderson K, Kaplan DL, Rosenblatt M. Human bone marrow-derived mscs can home to orthotopic breast cancer tumors and promote bone metastasis. Cancer Res. 2010;70:10044–10050. doi: 10.1158/0008-5472.CAN-10-1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang F, Tsai S, Kato K, Yamanouchi D, Wang C, Rafii S, et al. Transforming growth factor-beta promotes recruitment of bone marrow cells and bone marrow-derived mesenchymal stem cells through stimulation of mcp-1 production in vascular smooth muscle cells. J Biol Chem. 2009;284:17564–17574. doi: 10.1074/jbc.M109.013987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hall A. Rho gtpases and the actin cytoskeleton. Science. 1998;279:509–514. doi: 10.1126/science.279.5350.509. [DOI] [PubMed] [Google Scholar]
- 45.Derynck R, Zhang YE. Smad-dependent and smad-independent pathways in tgf-beta family signalling. Nature. 2003;425:577–584. doi: 10.1038/nature02006. [DOI] [PubMed] [Google Scholar]
- 46.Belema-Bedada F, Uchida S, Martire A, Kostin S, Braun T. Efficient homing of multipotent adult mesenchymal stem cells depends on frount-mediated clustering of ccr2. Cell Stem Cell. 2008;2:566–575. doi: 10.1016/j.stem.2008.03.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.