Abstract
We describe for the first time a case of an infant with rotavirus gastroenteritis complicated by a duodenal perforation. Awareness of the perforation risk may prevent severe or lethal outcomes in this common infection among infants and children.
Background
Gastrointestinal perforations are rare in the paediatric population and are mainly observed in sick preterm infants or in older children receiving intensive care.1 Reports on intestinal perforations associated with gastroenteritis are few and are missing on rotavirus-related infections.
Rotavirus is a frequent cause of acute gastroenteritis in childhood.2 It is usually a rather benign and self-limiting disease. However, worldwide it is estimated that rotavirus infections are responsible for half a million annual deaths in children, primarily related to acute severe dehydration. Rotavirus-related deaths are also reported in European countries, most frequently among infants3 and in neonates with rotavirus-associated necrotising enterocolitis.4 5
Case presentation
A previously healthy 9-month-old boy was admitted with clinical signs of severe dehydration after 5 days of diarrhoea, vomiting and fever. At home he had been given paracetamol, but no other medication. Upon admission he was lethargic and had clinical signs of shock with cold extremities, a prolonged capillary refill time (>3 s) and tachycardia. He responded clinically to fluid resuscitation, but developed abdominal pain, haematemesis and a distended abdomen. A plain abdominal x-ray revealed free subdiaphragmatic air (figure 1). He was operated and a small postpyloric duodenal perforation was detected and surgically closed. The postoperative course was uneventful.
Figure 1.
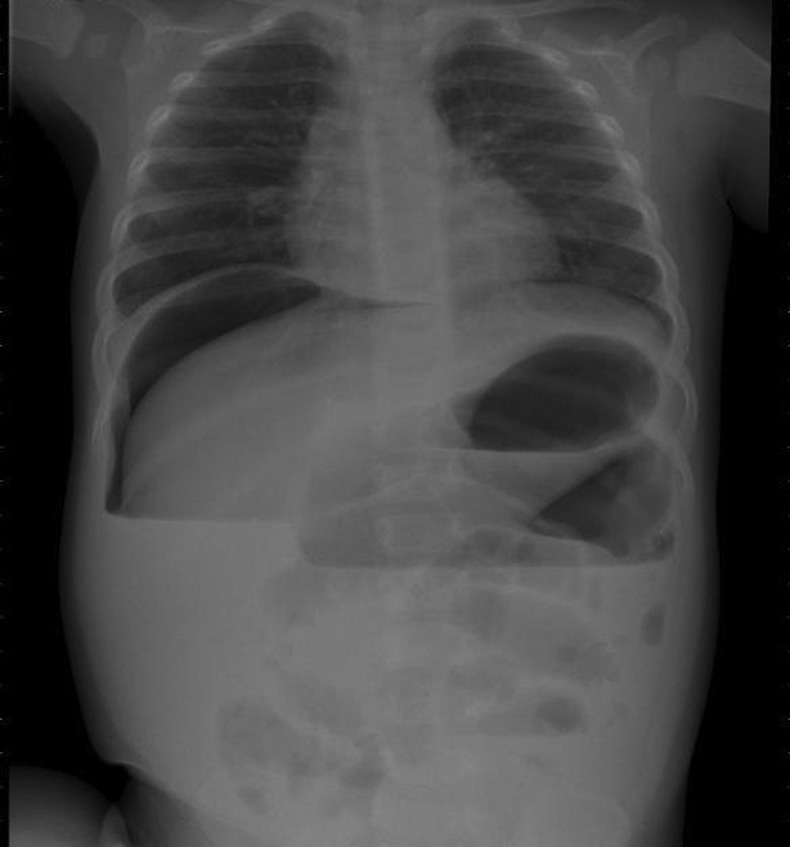
Free subdiaphragmatic air on plain abdominal x-ray of 9-month-old boy with duodenal perforation associated with rotavirus gastroenteritis.
Rotavirus antigen was found in the faeces. Stool cultures did not reveal pathogenic bacteria. Helicobacter pylori antigen in faeces was negative. The serum gastrin level was normal. Endoscopy 3 months later revealed normal findings and histological analyses of gastric and duodenal mucosa were all normal.
Discussion
A gastrointestinal perforation associated with acute diarrhoeal disease in children is very rare. We conducted a structured literature search in PubMed for the period from 1960 to 2012 using combinations of the search words ‘intestinal perforation’, ‘rotavirus’, ‘acute diarrhoea’ ‘children’ and ‘paediatric’, with non-English papers and papers on neonates (first 28 days of life) with gastrointestinal perforations being excluded. We found only five cases reporting a similar clinical picture as in this patient (table 1), all with duodenal perforation site and haematemesis and one additional paediatric case with rotavirus-associated gastric rupture.6–11 None of the cases with duodenal perforation were diagnosed with a rotavirus infection. However, Nejihashi et al12 recently described a healthy infant with rotavirus gastroenteritis who presented with haematemesis owing to a non-perforated bleeding duodenal ulcer.
Table 1.
Previous paediatric reports on gastrointestinal perforations associated with acute diarrhoeal disease
| Author | Sex | Age | Medical history | Acute symptoms of gastroenteritis | Dehydration | Haematemesis | Site of perforation |
|---|---|---|---|---|---|---|---|
| Johnstone et al7 | Boy | 1 year | Healthy | Loose stools and vomiting | + | ND | Duodenal |
| Bell et al6 | ND | 6 months | Healthy | Diarrhoea and vomiting | + | + | Duodenal |
| Tan et al9 | Girl | 3 year | Aqueductal stenosis and VP shunt | Diarrhoea and vomiting | + | + | Duodenal |
| Wilson et al10 | Boy | 7 year | Neurologically disabled | Diarrhoea and vomiting | + | + | Duodenal |
| Lee et al 8 | Boy | 3 month | Healthy | Diarrhoea | ND | + | Duodenal |
| Shimizu et al11 | Girl | 3 month | Hypothyroidism | Vomiting | + | − | Gastric |
ND, no data; VP, ventriculoperitoneal.
We urge clinicians to consider gastrointestinal perforation as a potentially severe complication in children with acute gastroenteritis, dehydration and in particular if the abdomen is distended and there is haematemesis. A plain abdominal x-ray may reveal pneumoperitoneum and guide appropriate treatment.
Learning points.
Gastrointestinal perforation in infants and children with rotavirus infections is rare, but a severe and potentially lethal complication.
Awareness of this complication in children with severe gastroenteritis is important for appropriate treatment.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Grosfeld JL, Molinari F, Rescorla FJ, et al. Gastrointestinal perforation and peritonitis in infants and children: experience with 179 cases over ten years. Surgery 1996;2013:650–5 [DOI] [PubMed] [Google Scholar]
- 2.Parashar UD, Hummelman EG, Glass RI, et al. Global illness and deaths caused by rotavirus disease in children. Emerg Infect Dis 2003;2013:565–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koch J, Wiese-Posselt M. Epidemiology of rotavirus infections in children less than 5 years of age: Germany, 2001–2008. Pediatr Infect Dis J 2011;2013:112–17 [DOI] [PubMed] [Google Scholar]
- 4.Rotbart HA, Nelson WL, Yolken RH, et al. Neonatal rotavirus-associated necrotizing enterocolitis: case control study and prospective surveillance during an outbreak. J Pediatr 1988;2013:87–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shai S, Perez-Becker R, Forster J, et al. Rotavirus disease in Germany—a prospective survey of very severe cases. Pediatr Infect Dis J 2013;2013:e62–7 [DOI] [PubMed] [Google Scholar]
- 6.Bell MJ, Keating JP, Bower RJ, et al. Perforated stress ulcers in infants. J Pediatr Surg 1981;2013:998–1002 [DOI] [PubMed] [Google Scholar]
- 7.Johnstone JM, Rintoul RF. Perforated duodenal ulcer in childhood. Br J Surg 1972;2013:288–9 [DOI] [PubMed] [Google Scholar]
- 8.Lee NM, Yun SW, Kwak BK, et al. Perforated duodenal ulcer presenting with massive hematochezia in a 30-month-old child. World J Gastroenterol 2009;2013:4853–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tan SH, Joseph VT, Wong HB. Perforated chronic duodenal ulcer in children. Singapore Med J 1984;2013:187–9 [PubMed] [Google Scholar]
- 10.Wilson JM, Darby CR. Perforated duodenal ulcer: an unusual complication of gastroenteritis. Arch Dis Child 1990;2013:990–1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shimizu T, Horiuchi T, Tamai H, et al. Idiopathic gastric rupture in a 3-month-old girl. Acta Paediatr 2003;2013:628–30 [DOI] [PubMed] [Google Scholar]
- 12.Nejihashi N, Sakano T, Ohta T, et al. An infant with rotavirus infection presenting as a severe acute duodenal ulcer. Pediatr Int 2011;2013:100–1 [DOI] [PubMed] [Google Scholar]


