Abstract
A 36-year-old man was referred to the general medical team with endophthalmitis. He was noted to have raised inflammatory markers and deranged liver function tests on admission. Subsequent abdominal ultrasound scan revealed a liver abscess requiring percutaneous drainage. A common human pathogen, Klebsiella pneumoniae, was cultured from multiple sites. K pneumoniae has virulent serotypes (K1 and K2) that can cause primary liver abscess with metastatic infections. Cases have previously been predominantly reported in Southeast Asia but are increasing in prevalence in Europe and North America. The main known risk factor for the disease is diabetes mellitus. Swift antibiotic therapy, ophthalmology review and percutaneous drainage of any liver abscess are essential. Early recognition of the syndrome, despite potentially few initial symptoms, can significantly reduce morbidity and mortality. The authors report the first recorded case of K pneumoniae liver abscess with endophthalmitis in the UK.
Background
Klebsiella pneumoniae liver abscess with extrahepatic complications is predominantly seen in Southeast Asia with an increasing number of cases being reported in Western Europe and North America. Diabetes mellitus predisposes a patient to developing the disease. Early antibiotic treatment is essential to reduce morbidity and mortality. This case presents the first recorded case of K pneumoniae liver abscess with endophthalmitis in the UK.
Case presentation
A 36-year-old Iraqi man, who last travelled to Iraq 6 months ago, was referred from a specialist eye hospital for a 3-day history of severe central right eye pain and reduced vision. Prior to the eye pain he had a 2-week history of feeling ‘cold and shivering’. This had been empirically treated with a course of amoxicillin. He also had a 6-day history of first right metatarsophalangeal and left knee joint pain, for which he was given naproxen for presumed gout. He informed us that he had had urethritis without haematuria on a few occasions over the preceding week. All other systems were unremarkable. He had no significant medical history.
On admission he was febrile. On examination of the right eye there was a mild periorbital oedema with severe chemosis. The cornea was hazy (figure 1) and visual acuity was limited to perception of light. General examination was otherwise unremarkable.
Figure 1.
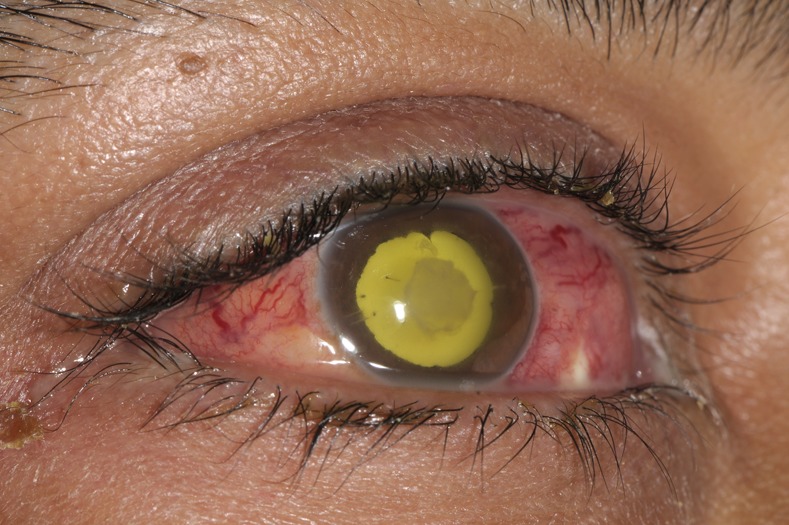
Endophthalmitis.
Investigations
Initial blood results showed raised inflammatory markers with a white cell count (WCC) of 15.8× 109/l (neutrophil count of 12.6 × 109/l) and C reactive protein of 140 mg/l. Liver function tests were deranged with an alanine aminotransferase (ALT) of 66 IU/l and alkaline phosphatase (ALP) of 223 IU/l but a normal total bilirubin level of 11 mg/dl and prothrombin time. Testing for diabetes mellitus and HIV were both negative.
Aqueous and intravitreal biopsies grew K pneumoniae and he was diagnosed with endogenous endophthalmitis secondary to a systemic infection. Blood cultures were negative. Mid-stream urine grew K pneumoniae.
Chest x-ray was unremarkable.
Abdominal ultrasound scan showed a 6.3×5.4 cm hypoechoic avascular lesion within segment 8 of the liver (figure 2). This liver abscess was confirmed by abdominal CT. Following drainage of the abscess, MR cholangiopancreatography was performed to rule out a biliary fistula, which showed 2.6×2.6 cm focus of intermediate T2-weighted signal within segments 8/4A of the liver. There was no evidence of gallstones or a biliary fistula.
Figure 2.

Abdominal ultrasound scan showing a liver abscess.
A whole body bone scan was performed to rule out osteomyelitis. This showed increased uptake and vascularity at the right first metatarsal bone with no increased uptake around the orbital bones bilaterally.
MRI of both orbits revealed right-sided panophthalmitis.
MRI of the right foot revealed flexor halluces longus tenosynovitis.
Treatment
The patient was given intravitreal amikacin 0.4 mg/0.1 ml and vancomycin 1 mg/0.1 ml. He was then initiated on dexamethasone 0.1% hourly, chloramphenicol 0.5% four times a day and cyclopentolate 1% three times a day for his right eye.
The liver abscess was percutaneously drained under ultrasound guidance, 80 ml of pus was drained which grew K pneumoniae sensitive to ciprofloxacin. He was treated with a 10-week course of oral ciprofloxacin 750 mg twice daily.
On day 10 of his antibiotic course and following abscess drainage his liver function tests improved to ALT 53 IU/l, ALP 158 IU/l and bilirubin 5 mg/dl. On discharge (day 30) his blood tests revealed WCC 5.3× 109/l, ALT 47 IU/l, ALP 141 IU/l and bilirubin 4 mg/dl.
Outcome and follow-up
A 2-month follow-up revealed liver function tests were within normal limits (ALT 31 IU/l, ALP 73 IU/l and bilirubin 6 mg/dl) and MRI liver scan showed no residual disease or evidence of a biliary fistula.
Visual acuity in the right eye has deteriorated and he now has no vision in this eye.
Discussion
K pneumoniae, a common human pathogen, is most often associated with pneumonia and urinary tract infections. Recently, there has been a reported rise in the incidence of a new syndrome occurring primarily in middle-aged men in Taiwan.1 2 In these cases, community acquired K pneumoniae serotypes K1 and K2 have been found to cause primary liver abscess with metastatic infections.1 Extrahepatic infections include: bacteraemia, meningitis, endophthalmitis, necrotising fasciitis, endocarditis, spinal epidural abscesses, septic pulmonary embolism and septic arthritis.3–9 The predominance of cases in Southeast Asia, particularly Taiwan, is unexplained. This genotype of K pneumoniae has not only been isolated in Taiwan but in three different continents indicating a geographically widespread pathogen.10 The majority of cases outside Asia were of patients of Asian decent, however, no research has proven a genetic predisposition in the Asian population.
K pneumoniae is often found in the intestinal flora of healthy individuals and can infect the liver via the portal system or intestinal epithelium.11 Recent studies have shown an increased prevalence of the virulent K pneumoniae in faecal samples from subjects of Asian descent compared with those from other backgrounds. This may explain the high prevalence of the disease in Asia.12 13
Diabetes mellitus is a significant predisposing risk factor for K pneumoniae liver abscess. Good glycaemic control reduces the risk of metastatic infections, especially endophthalmitis. The increased risk in diabetics is because of the impaired neutrophil-mediated phagocytosis of capsular serotypes K1 and K2 K pneumoniae.14 The significance of other risk factors for developing the disease has been poorly studied but include: excess alcohol intake, hepatobiliary disease, previous intraabdominal surgery and occult colon cancer.6
Patients with K pneumoniae liver abscess commonly present with fevers, rigors and right upper quadrant pain. These symptoms are not specific to K pneumoniae but rather an indication of a possible pyogenic liver abscess. Symptoms of extraheptic infections occasionally manifest first and, therefore, imaging of the liver is essential. Blood tests usually show an elevated WCC (neutrophilia), platelet count, C reactive protein and abnormal liver function tests.8
K pneumoniae endophthalmitis classically presents with swelling, redness, sudden-onset of blurred vision and pupillary hypopyon.15 The diagnosis is confirmed by positive swab microbiology or blood cultures.16 17 Visual outcome tends to be poor with sight limited to hand motion if light can be perceived. Good vision at diagnosis is a predictor of better visual outcomes.18
CT imaging of the liver is the most sensitive method of diagnosing an abscess.19 Appearances on CT that indicates an abscess are most likely to be caused by K pneumoniae include a single abscess, unilobar involvement (commonly right lobe), solid and/or multiloculated.20 As patients are susceptible to septic pulmonary emboli, chest x-ray is recommended. Multiple, ill-defined peripheral round opacities on x-ray indicate the need for further imaging, commonly CT of chest.21
Early antibiotic treatment is essential, third-generation cephalosporins are frequently used to treat both the liver abscess and metastatic infections.8 The duration of treatment is determined by the resolution of fever, neutrophilia and liver abscess. Cephalosporins have a good and fast penetration to the aqueous humour of the eye, cerebrospinal, synovial and pericardial fluid.22 23 The liver abscess itself requires early percutaneous drainage.
Learning points.
Consider the diagnosis of Klebsiella pneumoniae serotypes K1 and K2 in patients presenting with multiple infected sites, particularly in those of Asian descent.
Undertake imaging of the liver to rule out pyogenic abscess in patients presenting with K pneumoniae endophthalmitis.
Early antibiotic intervention, percutaneous drainage of any liver abscess and ophthalmology review is essential.
Although this condition is more prevalent in Southeast Asia, cases have been reported in the USA, Australia, Spain and the Middle East. This is the first recorded case in the UK.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Siu LK, Yeh KM, Lin JC, et al. Klebsiella pneumoniae liver abscess: a new invasive syndrome. Lancet Infect Dis 2012;2013:881–7 [DOI] [PubMed] [Google Scholar]
- 2.Lederman ER, Crum NF. Pyogenic liver abscess with a focus on Klebsiella pneumoniae as a primary pathogen: an emerging disease with unique clinical characteristics. Am J Gastroenterol 2005;2013:322–31 [DOI] [PubMed] [Google Scholar]
- 3.Chang WN, Huang CR, Lu CH, et al. Adult Klebsiella pneumoniae meningitis in Taiwan: an overview. Acta Neurol Taiwan 2012;2013:87–96 [PubMed] [Google Scholar]
- 4.Fung CP, Chang FY, Lee SC, et al. A global emerging disease of Klebsiella pneumoniae liver abscess: is serotype K1 an important factor for complicated endophthalmitis? Gut 2002;2013:420–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu BS, Lau YJ, Shi ZY, et al. Necrotizing fasciitis associated with Klebsiella pneumoniae liver abscess. Clin Infect Dis 1999;2013:1360–1 [DOI] [PubMed] [Google Scholar]
- 6.Matsushita M, Hajiro K, Okazaki K, et al. Endophthalmitis with brain, lung, and liver abscesses associated with an occult colon cancer. Am J Gastroenterol 2000;2013:3664–5 [DOI] [PubMed] [Google Scholar]
- 7.Hsieh MJ, Lu TC, Ma MH, et al. Unrecognized cervical spinal epidural abscess associated with metastatic Klebsiella pneumoniae bacteremia and liver abscess in nondiabetic patients. Diagn Microbiol Infect Dis 2009;2013:65–8 [DOI] [PubMed] [Google Scholar]
- 8.Lee SS, Chen YS, Tsai HC, et al. Predictors of septic metastatic infection and mortality among patients with Klebsiella pneumoniae liver abscess. Clin Infect Dis 2008:642–50 [DOI] [PubMed] [Google Scholar]
- 9.Kohler JE, Hutchens MP, Sadow PM, et al. Klebsiella pneumoniae necrotizing fasciitis and septic arthritis: an appearance in the Western hemisphere. Surg Infect (Larchmt) 2007;2013:227–32 [DOI] [PubMed] [Google Scholar]
- 10.Turton JF, Englender H, Gabriel SN, et al. Genetically similar isolates of Klebsiella pneumoniae serotype K1 causing liver abscesses in three continents. J Med Microbiol 2007;2013:593–7 [DOI] [PubMed] [Google Scholar]
- 11.Fung CP, Lin YT, Lin JC, et al. Klebsiella pneumoniae in gastrointestinal tract and pyogenic liver abscess. Emerg Infect Dis 2012;2013:1322–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siu LK, Fung CP, Chang FY, et al. Molecular typing and virulence analysis of serotype K1 Klebsiella pneumoniae strains isolated from liver abscess patients and stool samples from noninfectious subjects in Hong Kong, Singapore, and Taiwan. J Clin Microbiol 2011;2013:3761–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chung DR, Lee H, Park MH, et al. Fecal carriage of serotype K1 Klebsiella pneumoniae ST23 strains closely related to liver abscess isolates in Koreans living in Korea. Eur J Clin Microbiol Infect Dis 2012;2013:481–6 [DOI] [PubMed] [Google Scholar]
- 14.Lin JC, Siu LK, Fung CP, et al. Impaired phagocytosis of capsular serotypes K1 or K2 Klebsiella pneumoniae in type 2 diabetes mellitus patients with poor glycemic control. J Clin Endocrinol Metab 2006;2013:3084–7 [DOI] [PubMed] [Google Scholar]
- 15.Yang CS, Tsai HY, Sung CS, et al. Endogenous Klebsiella endophthalmitis associated with pyogenic liver abscess. Ophthalmology 2007;2013:876–80 [DOI] [PubMed] [Google Scholar]
- 16.Tan YM, Chee SP, Soo KC, et al. Ocular manifestations and complications of pyogenic liver abscess. World J Surg 2004;2013:38–42 [DOI] [PubMed] [Google Scholar]
- 17.Sheu SJ, Kung YH, Wu TT, et al. Risk factors for endogenous endophthalmitis secondary to Klebsiella pneumoniae liver abscess: 20-year experience in Southern Taiwan. Retina 2011;2013:2026–31 [DOI] [PubMed] [Google Scholar]
- 18.Lee S, Um T, Joe SG, et al. Changes in the clinical features and prognostic factors of endogenous endophthalmitis: fifteen years of clinical experience in Korea. Retina 2012;2013:977–84 [DOI] [PubMed] [Google Scholar]
- 19.Golia P, Sadler M. Pyogenic liver abscess: Klebsiella as an emerging pathogen. Emerg Radiol 2006;2013:87–8 [DOI] [PubMed] [Google Scholar]
- 20.Alsaif HS, Venkatesh SK, Chan DS, et al. CT appearance of pyogenic liver abscesses caused by Klebsiella pneumoniae. Radiology 2011;2013:129–38 [DOI] [PubMed] [Google Scholar]
- 21.Lin JC, Chang FY. Pyogenic liver abscess associated with septic pulmonary embolism. J Chin Med Assoc 2008;2013:603–4 [DOI] [PubMed] [Google Scholar]
- 22.Sharir M, Triester G, Kneer J, et al. The intravitreal penetration of ceftriaxone in man following systemic administration. Invest Ophthalmol Vis Sci 1989;2013:2179–83 [PubMed] [Google Scholar]
- 23.Cherubin CE, Eng RH, Norrby R, et al. Penetration of newer cephalosporins into cerebrospinal fluid. Rev Infect Dis 1989;2013:526–48 [DOI] [PubMed] [Google Scholar]


