Abstract
Spinal epidural abscess (SEA) is a rare clinical condition among children. Most patients do not present with classical signs. A 13-year-old boy without any predisposing factors presented with paraparesis, bladder and bowel involvement. MRI spine demonstrated an SEA at the C7 and D1 levels on both sides of the midline with cord oedema at the C2–3 to C6 level with minimal marrow oedema in the C6 vertebral body. We treated the patient with antibiotics (ceftriaxone and vancomycin) alone. The patient showed excellent response with only minimal residual gait disturbance at the end of 6 weeks of antibiotic therapy. This is the first paediatric report of complete recovery of a patient at clinical stage 4 following antibiotic treatment alone from India. However, caution should be exercised to closely monitor the patient’s recovery as any progression in the neurological state warrants surgery.
Background
Spinal epidural abscess (SEA) is a rare clinical condition in children with an incidence of 0.2–1.2/10 000 hospital admissions.1 2 The important predisposing conditions for SEA are immunodeficiency, spinal trauma, procedures (epidural analgesia or block) or congenital anomaly of the spine and a source of infection (like skin and soft tissue infections, osteomyelitis). Most patients suffer from a significant diagnostic delay as only a minority present with the classic clinical triad of back pain, fever and neurological deficit.3 Surgical drainage with antibiotics is the most common treatment method.1–4 We present a case of SEA treated with only the use of antibiotics.
Case presentation
A 13-year-old previously healthy boy presented with neck and upper back pain and a tingling sensation in the hands and feet during the previous 6 days. In the last 4 days, the boy also reported urine incontinence, abdominal distension and an inability to sit or walk. Transient fever was reported within the 6-day period. The examination revealed neck stiffness and pain while performing the passive straight leg raise test. There was spinal tenderness in the upper back and flaccid paralysis below the D4 level with bowel and bladder involvement. There was no history of tuberculosis exposure.
Investigations
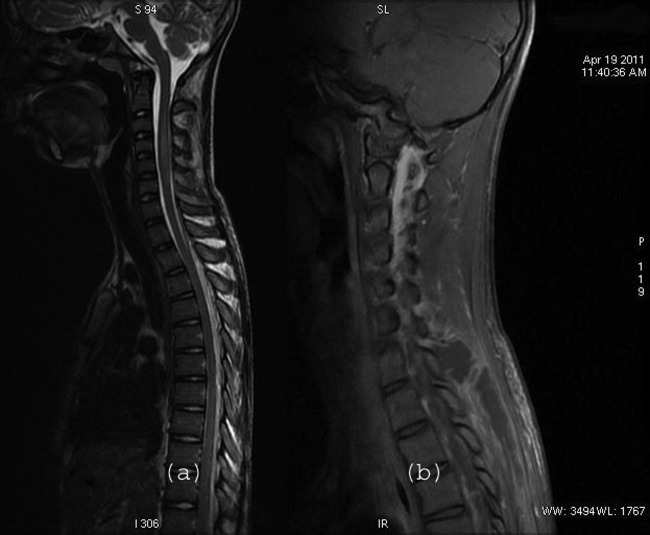
The total leucocyte count was 7100/mm3, erythrocyte sedimentation rate by Westergren method was 22 mm (high for age and sex) and an elevated C reactive protein. Cerebrospinal fluid examination showed 800 cells/mm3, 98% lymphocytes and 2% polymorphs with low (21 mg/dl) sugar. Plain and contrast-enhanced MRI scan of the spine (figure 1) showed necrotic collection with loculation in the posterior paraspinal muscles at the C7 and D1 levels on both sides of the midline extending into the C6–7 apophyseal joint bilaterally. This collection extends posteriorly into the epidural space from the D1 to the L3 level, obliterating the CSF column with no significant cord compression. Minimal oedema was noted in cord parenchyma at the C2–3 to the C6 level with minimal marrow oedema in the C6 vertebral body. Follow-up MRI (figure 2), which was done after 8 weeks, showed complete resolution of necrotic collection in the epidural space as well as the paraspinal plane. Blood culture and CSF culture were negative.
Figure 1.
T2-weighted sagittal image showing epidural collection dorsally extending from D1 to the dorsolumbar region with cord oedema in the cervical region from the C2–3 to the C6 level. Contrast-enhanced fat suppressed T1-weighted sequence in the right parasagittal plane showing an abscess appearing as a necrotic collection in the posterior paraspinal muscles with enhancing capsule/granulation tissue peripherally and involvement of the C6–7 apophyseal joint.
Figure 2.
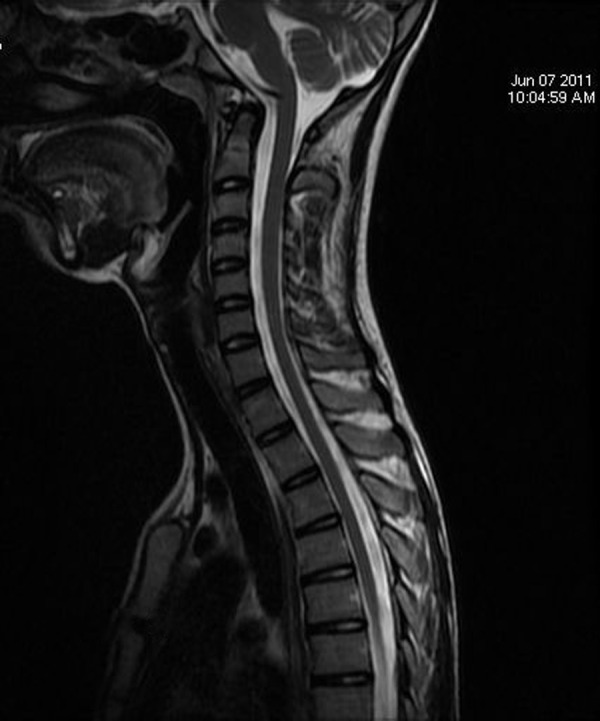
Follow-up T2-weighted sequence in the sagittal plane revealing a completely resolved epidural collection and cord oedema.
Differential diagnosis
The clinical differential diagnosis included acute myelitis, diskitis and meningitis. However, considering the classic triad of back pain, fever and neurological deficit, SEA was also suspected.1
Treatment
Patient was started on intravenous ceftriaxone (100 mg/kg/day) and vancomycin (10 mg/kg/dose, 8th hour).
Outcome and follow-up
Within 48 h of initiating the antibiotics, the patient began to demonstrate neurological improvement. The power of the lower limbs increased to grade 3/5 within 2 weeks and bladder control improved after 3 weeks. After the completion of a 6-week antibiotic therapy, only a minor residual gait disturbance could beobserved.
Discussion
A clinical staging system1 for SEA is useful for monitoring the clinical progression of the disease: stage 1, back pain at the level of the affected spine; stage 2, nerve-root pain radiating from the involved spinal area; stage 3, motor weakness, sensory deficit, bladder and bowel dysfunction; and stage 4, paralysis.
The cultures in the present case were negative but usually Staphylococcus aureus is the most common aetiological organism in children. S aureus is responsible for 86% of cases in children.4 Two cases of tubercular SEA have also been reported from India.5 MRI is the imaging modality of choice for establishing the diagnosis and monitoring progression.1
Decompressive laminectomy and debridement of infected tissues, together with systemic antibiotics, is the treatment of choice.1–4 Surgical drainage should be performed immediately as it is difficult to predict the progression of the disease.1 2 Medical management should be considered in patients who present without neurological deficit, complete deficit (clinical stage 4) for more than 72 h, extensive multilevel abscess or pan spinal disease, or patients with high operative risk because of severe concomitant disease.1 In the present case, surgical debridement was not performed as the patient presented with complete neurological deficit for 4 days.
The main outcome determinant for patients with SEA is neurologic status at the time of diagnosis. The death rate in adults varies between 5% and 23%, but mortality and morbidity are lower in children.3 Recent comparisons of medical and surgical management strategies demonstrated better outcomes for medical management.6
This is the first report of complete recovery from clinical stage 4 symptoms of a paediatric patient following antibiotic treatment alone in India. However, one should be cautious and closely monitor the patient’s recovery as any progression in the neurological stage warrants surgery. Our patient might have responded to antibiotics because of the lack of associated risk factors for SEA.
Learning points.
Acknowledgments
The authors would like to thank the Medical Director, Dr VK Mahadik, and the Dean, Dr JK Sharma, of RD Gardi Medical College, Ujjain, India, for granting us permission to publish the case. We acknowledge the help of Kristi Sydney, PhD scholar at Global Health (IHCAR), for English language review.
Footnotes
Contributors: AP, PS and MD diagnosed the case and followed the clinical course of the patient. PG reported the MRI and selected the radiological pictures for the case report. AP and PS wrote the first draft of the case report. AP, PS, PG and MD revised the paper critically for substantial intellectual content. All authors read and approved the final manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Darouiche RO. Spinal Epidural Abscess. NEJM 2006;2013:2012–20 [DOI] [PubMed] [Google Scholar]
- 2.Rubin G, Michowiz SD, Ashkenasi A, et al. Spinal epidural abscess in the pediatric age group: case report and review of literature. Pediatr Infect Dis J 1993;2013:1007–11 [DOI] [PubMed] [Google Scholar]
- 3.Auletta JJ, John CC. Spinal epidural abscesses in children: a 15-year experience and review of the literature. Clin Infect Dis 2001;2013:9–16 [DOI] [PubMed] [Google Scholar]
- 4.Jacobsen FS, Sullivan B. Spinal epidural abscesses in children. Orthopedics 1994;2013:1131–8 [DOI] [PubMed] [Google Scholar]
- 5.Kumar A, Singh AK, Badole CM, et al. Tubercular epidural abscess in children: report of two cases. Indian J Tuberc 2009;2013:217–19 [PubMed] [Google Scholar]
- 6.Karikari IO, Powers CJ, Reynolds RM, et al. Management of a spontaneous spinal epidural abscess: a single-center 10-year experience. Neurosurgery 2009; 2013:919–23; discussion 23–4 [DOI] [PubMed] [Google Scholar]