Summary
Background
In October 2010 an outbreak of cholera began among a group of small-scale gold miners in the East-Akim Municipality (EAM), Eastern Region. We investigated to verify the diagnosis, identify risk factors and recommend control measures.
Methods
We conducted a descriptive investigation, active case-search and an unmatched case-control study. A cholera case-patient was a person with acute watery diarrhoea, with or without vomiting in EAM from 1st October to 20th November, 2010. Stool from case-patients and water samples were taken for laboratory diagnosis. We performed univariate and bivariate analysis using epi-info version 3.3.
Results
Of 136 case-patients, 77 (56.6%) were males, of which 40% were miners or from miners households. Index case, a 20 yr-old male miner from Apapam village reported on October 13th, and case-patients peaked (18.4%) 20 days later. Attack rate was 2/1000 population with no fatality. Ages ranged from 1–84 years; mean of 34±18 yrs. Age-group 20–29 yrs was mostly affected (30.1%) with Apapam village having most case-patients (19.9%). Vibrio cholera serotype ogawa was isolated from stool samples. The main water source, Birim river was polluted by small-scale miners through defecation, post-defecation baths and sand-washings. Compared to controls, case-patients were more likely to have drunk from Birim-River [OR= 6.99, 95% CI: 2.75–18].
Conclusion
Vibrio cholera serotype ogawa caused the EAM cholera-outbreak affecting many young adult-males. Drinking water from contaminated community-wide -River was the major risk factors. Boiling or chlorination of water was initiated based on our recommendations and this controlled the outbreak.
Keywords: case-control study, cholera, outbreaks, serotype-ogawa, miners, Ghana
Introduction
Cholera is an acute infectious illness with profuse watery diarrhoea caused by toxigenic Vibrio cholera serogroup O1 or O139. V. cholera is a curved Gram-negative bacillus that belongs to the family Vibrionaceae and shares common characteristics with the family Enterobacteriaceae1.
Its short incubation period of two hours to five days enhances the potentially explosive pattern of outbreaks. Cholera is transmitted through fecal contamination of water or food and can result in hypovolemic shock and death if not promptly treated with fluids. Transmission is closely linked to inadequate environmental management. The disease is a key indicator of lack of social development. Risk factors for cholera outbreaks include poor access to safe drinking water, contaminated food, inadequate sanitation, and large numbers of refugees or internally displaced persons (IDPs)1,2.
Principally, this historically dreaded disease remains a major public health problem in many parts of Africa, Asia, and Latin America1, 2. Globally, there are an estimated 3–5 million cholera cases and 100,000 – 120,000 cholera-deaths every year3. In Ghana, there were over 9,000 cholera cases in 1999 with approximately 250 deaths (CFR of 2.8%). Cholera is now thought to be endemic in parts of the country. Ghana has seen outbreaks of the disease roughly every five years since the 19704. As of April 2011, over 8000 cases with 89 deaths (CFR =1.1) had been reported mainly from three regions (Central, Eastern and Greater Accra) in an outbreak that began September 20105. In the Eastern region, two confirmed cases of cholera from the East Akim Municipality (EAM) were reported on October 29th, 2010.
We report the epidemiological investigation conducted to characterize the EAM outbreak, determine the associated risk factors and inform appropriate control measures.
Methods
Study Area
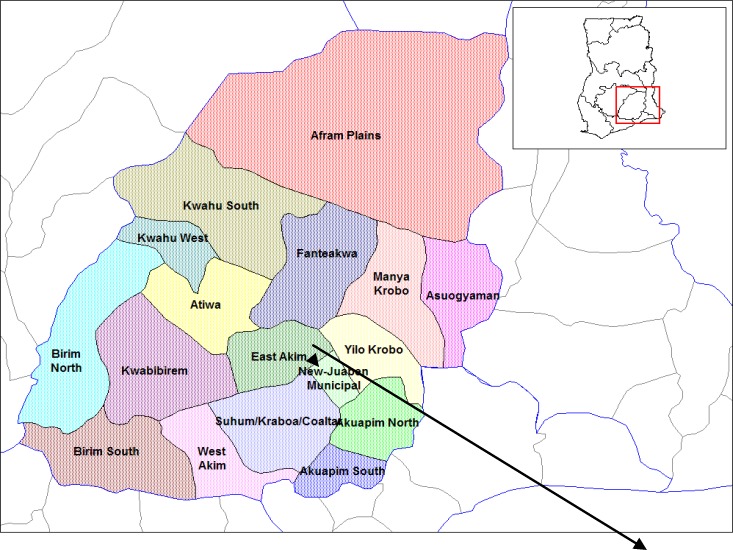
The outbreak investigation was conducted between 18th to 21st November 2010 in the East Akim Municipality in the Eastern Region of Ghana. The Municipal capital, Kibi, is 55km from the regional capital; Koforidua and 105km from the national capital Accra. The Municipality shares boundaries with Atiwa, New Juabeng, Suhum-Kraboa Coaltar, Kwaebibirem and Yilo krobo districts (Figure 1). It covers an area of 950 km2 and has six sub-municipalities namely Tafo, Kibi, Apedwa, Asafo, Bunso and Asiakwa with a total population of 114,837.
Figure 1.
Map of Eastern region of Ghana showing the East Akim Municipality (EAM)
There are two hospitals, four health centres, three clinics (private) and 15 Community-based Health Planning and Services (CHPS) compounds. The Disease Control Systems in the East Akim Municipality fall within the purview of the Disease Control Unit of the Ghana Health Service, the Environmental Health Unit of the District Assembly and a number of Non-Governmental Organizations.
The Disease Control Unit is responsible for the investigation of outbreaks of communicable diseases, surveillance of reportable diseases, and provision of educational materials and services to assist communities in reducing the incidence of communicable diseases.
The main economic activities in the municipality are farming, mining and petty trading. The Municipality experiences two main seasons as typical in other places in Ghana namely the wet season which starts from April and ends in October and a dry season from November to March.
The Birim River with its tributaries serves as the major source of drinking water for most of the communities in the Municipality. It also serves as the main source of water for mining activities in the area. The vegetation of the municipality is forest with traces of savannah in the north-eastern sector.
The outbreak was mainly cantered in Akim Tafo, Kibi-Apapam and Asikam. Akim Tafo is one of the urban sub-municipalities with a population of 26,798 while Kibi Apapam and Asikam are rural communities with a population of 2,630 and 533 respectively. Akim Tafo is populated with individuals engaged in economic activities in both the formal and informal sectors. Mining has become a major economic activity in Kibi Apapam and Asikam in recent times. Although diarrhoea diseases are prevalent in Akim Tafo no outbreaks have been reported in any of the three communities until October, 2010.
Study Design
Descriptive Study: We interviewed the Municipal Disease Control Officer (MDCO), the Public Health Nurse, the Hospital Management Teams, the Environmental Health Officer and the Municipal Chief Executive to obtain information on the outbreak and preliminary data on those affected. We reviewed surveillance data and the initial line-list generated by the MDCO.
Based on the information gathered we defined a cholera case-patient as a person having acute watery diarrhoea, with or without vomiting. We also defined a cholera case-patient as a person with vibrio cholera isolated from stool sample or epidemiologically-linked to a person with vibrio cholera isolation in East Akim Municipality between October 1st and November 20th, 2010. We then reviewed medical records from all health facilities in the municipality including the two large Government-owned Hospitals to identify persons meeting the case definition. Further records review was conducted at three other health facilities in nearby districts where some case-patients claimed to have visited. Data abstracted included age, sex, occupation, place of residence, date of onset, date of presentation at health facility, signs and symptoms, and outcome. Active case search and community interviews were conducted to trace other cases and contacts.
Case Control Study: We conducted unmatched case-control study in the municipality using the entire East Akim Municipality as study population. Based on sample size formula for comparing proportions as embedded in the ‘Statcalc’ utility feature of epi-info statistical software, we used a confidence level of 95%, power of 80%, expected exposure frequency in controls of 20%, expected exposure frequency in cases of 50%, case to control ratio of 1:2 and an odds ratio of 4 (for a risk factor on which intervention would have a significant impact) to a minimum sample size of 39 cases and 78 controls were obtained.
The case-definition was applied and controls were defined as persons living in the same community with case-patients but who did not have acute watery diarrhoea during the same period. Case finding was done through the Municipality database of cholera cases derived from inpatient information and case search provided by patients evaluated at the two hospitals, clinics and communities. These records captured demographic information including: name, gender, date of birth, place of birth, clinical status, therapeutic status, result of therapy, V. cholera serotype, and health system status.
Two controls were selected for each case by location of residence within the community. The controls were found for each case by a member of the investigation team standing in front of the case's house and spinning a bottle to determine a starting direction. Next, a number between two and five was drawn at random to indicate the number of houses in the chosen direction to proceed before attempting to interview the first control. This method was chosen because of the absence of a sampling frame (street addresses, post code etc).
The study was explained to the household by the field workers and if they agreed to participate, workers selected two of the available household members without diarrhoea and vomiting by simple number draws and interviewed the individuals as controls for the study. In the case of a refusal, the field-workers repeated the bottle-spinning procedure to select another household. Individuals were excluded from being controls if they reported suffering from watery diarrhoea since 1st October, 2010.
Copies of a standardized questionnaire, written in English, were administered to cases and controls in their native tongue by bilingual/multi-lingual trained interviewers/field workers recruited from the Municipal Health Directorate. The questionnaire collected basic demographic information and contained questions pertaining to potential food and water exposures and hygiene practices from October 1st to the interview date. In cases where a child was the study subject, questions were asked to an adult within the household (typically a family member) who had knowledge of the child's activities.
Laboratory Investigations: We collected stool and water samples from the case-patients and sent to the Regional Hospital laboratory at Koforidua for primary microbiologic assessment. The investigations were done by the laboratory staff of the hospital with the support of one of the co-authors.
Stool was either directly plated on thiosulfate-citrate-bile salts agar (TCBS) or transported on Cary-Blair transport media and plated on TCBS agar. Colonies of growth were evaluated using standard biochemical reactions, and vibrio cholera -positive isolates were serogrouped and serotyped using agglutination tests with commercial anti-sera.6
Environmental Survey: An environmental survey of households of cases and controls was undertaken. We inspected their sources of water supply principally observing activities around the community-wide Birim River, the drainage system, the sewage lines, general sanitation along the water bodies and collected water specimens and sent them for water quality testing at the Regional Hospital laboratory.
Ethical Issues: Informed consent and permission was sought from the participants before the interviews. We protected the confidentiality of participants through use of codes. However, ethical committee review did not apply as this was a public health response to an outbreak. Preliminary report of the outbreak was discussed with the District Health Administration, the District Assembly and the chiefs and elders of the affected communities.
Data Analysis: Data were entered into Epi Info software version 3.3 for data cleaning and analysis.
We performed descriptive analysis of the outbreak data by person, place and time. Univariate analyses were expressed as frequency distributions, percentages, mean± SD, range, and rates (attack rates, case-fatality rates etc) as appropriate. For inferential analysis of the case-control study data, we dichotomized qualitative exposure-variables and compared them among case-patients versus controls in bivariate analysis to identify potential risk factors using Chi-Square test at 95% confidence level or alpha-level of 5%. An exposure was considered a risk factor if the odds of association with cholera-case status at 95% confidence interval was statistically significant based on a p-value of <0.05.
Results
Descriptive Analysis
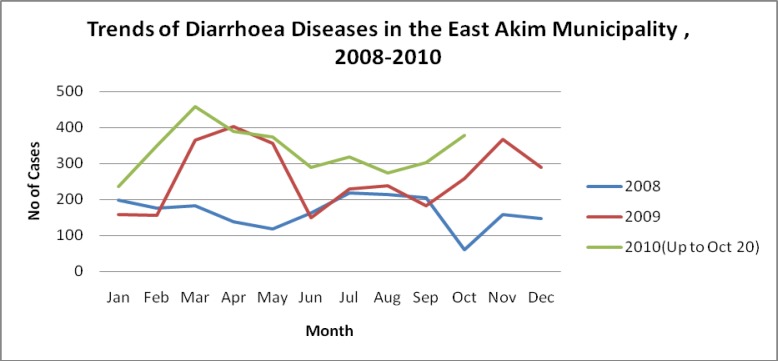
The distribution of diarrhoeal diseases for the past three years in the municipality shows an increasing trend in March–April and October–November between 2009 and 2010 (Figure 2).
The primary case was a 27 year old male “galamsey” worker, who developed diarrhoea and vomiting on the 13th of October, 2010. He had visited his mother at Apinamang in the Kwaebibirem district, who at the time of visit was suffering from severe diarrhoea with vomiting. The primary case assisted in transporting her to the St. Dominic's hospital in Akwatia. Immediately on his return to Kibi Apapam, he developed similar symptoms and signs and was rushed to the hospital on the 16th October.
The index case was a miner, 20 years of age from Apapam community who reported at Kibi Government Hospital on the 26th October, 2010. Stool specimen taken from both tested positive for Vibrio cholera. Through the active case search in the community, it was realized that a number of cases did not report to health facilities for medical attention but instead resorted to alternative local measures for treatment, for example, drinking of starch extracted from cassava, drinking of salty water, and a concoction of charcoal mixed with salt. A few others took Oral Rehydration Salts (ORS) bought from a nearby chemical shop.
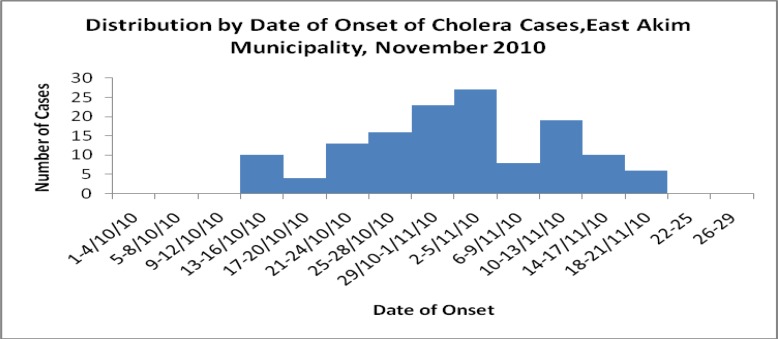
An intermittent common source outbreak was observed (Figure 3) with multiple peaks that commenced between 13th–16th October.
Figure 3.
Distribution of by date of onset of cholera cases in the study area.
The other peaks were observed in the periods 2nd–5th and 10th–13th November, 2010. There was a gradual increase in the number of cases from the 17th of October to the 5th of November then a sharp decline of cases up to the 9th of November. This was followed by a sudden increase in the number of cases which peaked between the 10th to the 13th of November, and a gradual decline in the number of cases up to the 21st of November.
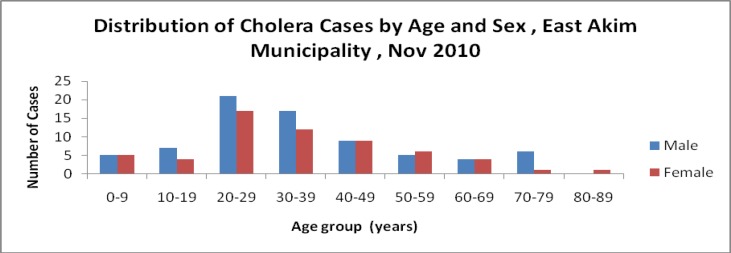
A total of 136 cases were recorded out of which 76 (56.6%) were males. Forty percent (30) of the males were miners. The overall attack rate was 0.18% or approximately 2 per 1000 population with no deaths. Sex- specific attack rates were 0.10% and 0.13% for females and males respectively. The age-specific attack rates among children under five and fifteen were 0.030% and 0.031% respectively, whilst among the youth the rate was 0.16%.
Males were more affected than females
The affected age ranges from 1–84 years with a median age of 30, mean of 34 and a standard deviation of 18 years. The age group 20–29 years was mostly 41 (30.1%) affected. The least 1 (0.007%) affected age group was above 80 years
Distribution of Cholera Cases by Place
Most of the affected cases were found in the Kibi-Apapam, Asikam, and Tafo catchment areas. The others were scattered in other areas in the Municipality. Twenty seven (19.8%) of the cases were found in the Tafo catchment area whilst Kibi Apapam had 25 (18.4%) cases. Asikam also recorded 23 cases constituting 16.9% of cases recorded.
Analytical Study
We recruited 107 participants for the case control study, of which 39 were cases and 78 were controls giving a case-to-control ratio of 1:2. The mean age for cases was 36.7 years and controls 33.7 years. The age range among the cases was 6 – 84 years and that of the controls 12– 80 years. The majority (22/39 or 56.4%) of cases were males whiles among the controls females (51/78 or 75%) were predominant. Diarrhoea (35.5%) was the commonest symptom among cases.
Those who developed cholera were 6.99 times as likely to have drunk from the river and streams as compared to those who did not develop the disease [OR= 6.99, 95% CI:2.75–18]
Laboratory Results
Two of the stool specimen that were sent to the Regional Hospital Laboratory for culture and identification were confirmed positive for Vibrio cholera serotype ogawa. Water samples showed no material growth.
Environmental Assessment
Most of the water bodies were found to be macroscopically dirty due to the indiscriminate mining activities. Majority of the people use pit latrines which were shallow because of high water table in most of the communities. Refuse disposal was poor with rubbish heaps near dwellings. Channels with stagnant water were common around buildings in swampy areas.
Discussion
Cholera is a disease of history that remains a major public health problem in many parts of Eastern region of Ghana which includes the East Akim Municipality. Cholera continues to be an important public health problem among many poorer and vulnerable communities, despite the detailed understanding of the bacteriology, epidemiology, and public health aspects for more than a century7.
The study revealed that, the cholera outbreak affected all age groups in the municipality and more especially among young adult males probably due to the involvement of some of them in the brisk small- scale mining activities in the area which exposed them to the index case through direct contact or sharing of contaminated water-source. Similar preponderance of cholera cases among males was observed by Sur et al8 in Kolkata, India. A number of females were also affected especially those aged between 20–49 years. This age group corresponds to the primary part of the population involved in the mining activity.
This observation could be due to the fact that some of the females were miners, a few as food vendors at the mining sites and also members of the household of the miners. Traditionally females are more involved in fetching water for domestic use from the local stream, possibly drinking directly from the stream, which could expose them further to the infection. Other age groups not directly involved in mining were minimally affected. House-hold contacts with affected small-scale illegal miners could be the underlying factor for the community-wide transmission of this outbreak.
The laboratory investigations on the stool specimen indicated the isolation of Vibrio cholera 01 serotype ogawa as the causative organism for the outbreak. Two of these specimens were taken from affected individuals in urban settlements in the district.
In a retrospective descriptive study by Alam M et al on 16,379 stool samples in Karachi, Pakistan (1997–2001), V. cholerae O1 Ogawa was the most common organism isolated (32.8%) and was found as the most common enteric pathogen isolated in an urban setting.9
Epidemiological and environmental evidence indicated that this outbreak was waterborne. Waterborne cholera is common worldwide.8,10 The Millennium Development Goals (MDG) proposes to decrease by half the population without access to safe water and sanitation by 2015.11 While the MDG consider piped water as an improved water source, transmission of waterborne pathogens may occur when the pipes are not periodically maintained or are absent.
We observed pollution of the Birim River with sand-washings and defecation by small-scale miners. Also, most of the people used shallow pit latrines due to the high water table in most of the communities. Environmental unsanitary conditions, dense population and large slum population are known to facilitate cholera outbreaks.12,13 The reproduction rate of cholera in a community is defined by social and environmental factors. The importance of the aquatic reservoir depends on the sanitary conditions of the community.14 Cholera is spread mainly through drinking fecal-contaminated water.
When cholera appears in a community, it is essential to ensure three things, namely hygienic disposal of human feces, an adequate supply of safe drinking water, and good food hygiene. The most useful measure in preventing the spread of cholera is the provision of safe drinking water and sanitary disposal of human feces.1, 2 Whereas typical at-risk areas for cholera outbreak include urban slums and camps for internally displaced people or refugees, our investigation revealed that certain occupational groups like the small-scale illegal miners or “Galamseys” who operate in conditions where minimum requirements of clean water and sanitation are not met may also facilitate the transmission of the disease.
As a limitation to the study, the rapid flow of the Birim River and the timing or location of water sample collection as well as probable technical deficiencies might have led to the non isolation of vibrio cholera or other known microbial causes of watery diarrhoea from the water samples sent to the laboratory. Social economic status and differences in age groups as confounders in the unmatched case control study could also influence the association found. Despite these limitations, the study provided useful information that will inform stake-holders actions in controlling the outbreak and to avert similar future outbreaks by ensuring the provision of potable water and proper sanitary environmental conditions among population groups in this and other communities in the country.
Conclusions
An outbreak of ogawa serotype cholera with no mortality was established in the East Akim Municipality. It was an intermittent common source outbreak and affected mostly persons aged 20–29 years from Tafo catchment area. We established that drinking from the community-wide rivers and streams in the municipality were the major risk factor for the outbreak. Boiling or chlorination of water was initiated based on our recommendations and this controlled the outbreak.
Figure 4.
Distribution of cholera cases by age and sex
Table 1.
Selected Exposures among Cases and Controls, East Akim Municipality, November, 2010
| Risk Factor | Cases #/Total |
Controls #/Total |
Odds Ratio |
95% C.I. |
| Water | ||||
| 1. Stream/river | 27/39 | 19/78 | 6.99 | 2.75–18.0 |
| 2. Borehole | 4/39 | 8/78 | 0.86 | 0.20–3.47 |
| 3. Sachet water | 1/39 | 18/78 | 0.09 | 0.00–0.68 |
| 4. Well | 3/39 | 15/78 | 0.35 | 0.07–1.42 |
| Food | ||||
| 5. Banku | 19/39 | 43/78 | 0.77 | 0.33–1.79 |
| 6. Fufu | 20/39 | 41/78 | 0.92 | 0.4–2.15 |
| 7. Kenkey | 9/39 | 16/78 | 1.16 | 0.42–3.21 |
| 8. Orange | 8/39 | 25/78 | 0.55 | 0.20–1.47 |
| Others | ||||
| 9. Availability of Latrine in house |
18/39 | 34/78 | 1.11 | 0.48–2.58 |
| 10. Washing of hands with soap before meals |
6/39 | 18/78 | 0.61 | 0.19–1.83 |
| 11. Contact with person with diarrhoea |
17/39 | 32/78 | 1.11 | 0.47–2.6 |
| 12. Visited any person with diarrhoea |
12/39 | 31/78 | 0.67 | 0.27–1.64 |
Acknowledgements
The authors wish to thank Regional Health Directorate-Koforidua, The District Health Management Team-East Akim and the Chiefs and Elders of East Akim for their assistance in the investigations.
References
- 1.Seas C, Gotuzzo E. Vibrio cholerae. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and Practice of Infectious Diseases. USA: Churchill Livingston; 2000. pp. 2266–2272. [Google Scholar]
- 2.Shears P. Recent developments in cholera. Curr Opin Infect Dis. 2001;14:553–558. doi: 10.1097/00001432-200110000-00008. [DOI] [PubMed] [Google Scholar]
- 3.WHO fact sheet on cholera. Last up-date August 2011. Available from: http://www.who.int/mediacentre/factsheets/fs107/en/
- 4.Amankwa J. Cholera epidemic kills 60 in Ghana. Ghanaweb. 2011. Mar 18th, Available from: http://www.ghanaweb.com/GhanaHomePage/NewsArchive/artikel.php?ID=205245.
- 5.Ghana Health Service/Ministry of health, author. Weekly Bulletin Disease Surveillance Division. 2010 Week 18. [Google Scholar]
- 6.Bopp CA, Ries A A, Wells J G. Laboratory Methods for the Diagnosis of Epidemic Dysentery and Cholera. Atlanta, GA: Centers for Disease Control and Prevention; 1999. [Google Scholar]
- 7.Shears P. Recent developments in cholera. Curr Opin Infect Dis. 2001;14:553–558. doi: 10.1097/00001432-200110000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Sur D, Deen J L, Manna B, Niyogi S K, Deb AK, Kanungo S. The burden of cholera in the slums of Kolkata, India: data from a prospective, community based study. Arch Dis Child. 2005;90:1175–1181. doi: 10.1136/adc.2004.071316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alam M, Akhtar Y N, Ali SS. Seasonal variation in bacterial pathogens isolated from stool samples in Karachi, Pakistan. J Pak Med Assoc. 2003;53:125–129. [PubMed] [Google Scholar]
- 10.Heymann DL, editor. Control of communicable diseases manual. 19th ed. Washington C, USA: American Public Health Association; 2008. Cholera and other vibrioses; p. 120. [Google Scholar]
- 11.WHO, author. First steps for managing an outbreak of acute diarrhoea. Geneva, Switzerland: WHO; Global task force on cholera control. WHO/CDS/CSR/NCS/2003.7 Rev.1. Available at: http://www.who.int/healthtopics/cholera. [Google Scholar]
- 12.Sur D, Sarkar B L, Manna B. Epidemiological, microbiological and electron microscopic study of a cholera outbreak in a Kolkata slum community. Indian J Med Res. 2006;123:31–36. [PubMed] [Google Scholar]
- 13.Sur D, Dutta S, Sarkar B L. Occurrence, significance and molecular epidemiology of cholera outbreaks in West Bengal. Indian J Med Res. 2007;125:772–776. [PubMed] [Google Scholar]
- 14.Codeco CT. Endemic and epidemic dynamics of cholera: the role of the aquatic reservoir. BMC Infect Dis. 2001;1:1. doi: 10.1186/1471-2334-1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]