Summary
Background
To determine the frequency and pattern of malignant tumours of the female genital tract among Batswana women.
Design
A four-year retrospective histological study of the pattern of female genital tract malignancy in Botswana.
Setting
University of Botswana and the National Health Laboratory Gaborone, Botswana. The National Health Laboratory is the only public tertiary referral laboratory that provides diagnostic pathology services in the South-Eastern part of Botswana. It is located just adjacent to Princess Marina Hospital, the major tertiary referral hospital in the country.
Methods
All histologically confirmed diagnoses of female genital tract malignancies from January 1st 2006 to December 31st 2009 were reviewed by two pathologists and diagnoses re-confirmed by taking fresh tissue sections from paraffin embedded archival tissue blocks.
Results
The age of patients ranged from 13–96 years with a mean age of 54.5 ± 6.4 years. Cancer of the cervix constituted 80.6%, followed by uterine cancer (10.0%), carcinomas of the vulva (4.5%) and ovary (3.4%) in that order. Ovarian cancers predominated in the younger age group. There was a steady increase in the frequencies of cervical, uterine and ovarian cancers over the 4-year study period with a decline in uterine cancer in the 4th year.
Conclusion
Cervical cancer incidence is high among Batswana women and all female genital tract cancers occurred at a relatively early mean age. Therefore the importance of established and accessible screening programs and awareness campaigns need more emphasis than it is being given currently.
Keywords: Malignant pattern, female genital tract, Batswana women
Introduction
Malignant tumours of the female genital tract have a worldwide distribution but the frequency varies from one region to the other.
Over the past 50 years, organized screening programs in developed countries have contributed significantly to the decline in incidence and mortality from cancer of the uterine cervix. In contrast, largely due to lack of organized screening programs in most parts of Africa, cervical cancer remains one of the major killers of women in Sub Saharan Africa. 1,2 Low socio-economic status, illiteracy and HIV/AIDS pandemic as well as cultural and religious inhibitions also contribute to this high incidence and mortality. In particular, studies from some African countries have reported a 3 to 4-fold increase in the incidence of cervical cancer among HIV-infected women. These cancers are usually of a higher histological grade and are more aggressive than their counterparts in HIV-negative women.3,4,5
Ovarian cancer is reported to be the second major cause of death in women among female genital tract malignancies,6 and at least 75% of patients present with advanced disease. Studies have found that, importantly, there was an early mean age of presentation of all female genital tract malignancies and this has significant economic and social implications. Therefore effective and accessible screening programs are needed as these cancers affect predominantly patients in the productive age bracket of the society.
In Botswana, no studies to date have dealt specifically with the frequency and patterns of female genital tract malignancy. This is a country with a very high HIV prevalence. Our study is aimed at providing baseline data on this topic for future studies in Botswana and to increase awareness on this subject.
Materials and Methods
This retrospective investigation is based on a study of surgical biopsy specimens received in the Anatomic Pathology laboratory of the National Health Laboratory Gaborone, Botswana from 1st January 2006 to 31st December 2009. The National Health Laboratory is the major Government Laboratory for diagnostic services in Botswana and receives specimens mainly from the South-Eastern part of Botswana.
The sources of the specimens were in-patient biopsy specimens form Princess Marina National Referral Hospital Gaborone or from District hospitals, and referrals from private health centres. All the surgical biopsy specimens were submitted to the National Health Laboratory Gaborone, Botswana. Demographic data which included age of the patients, site of tumour and diagnosis were extracted from the Integrated Patient Management System (IPMS) database. The histology reports were retrieved from the database and the diagnoses were reviewed by two consultant Pathologists.
Where there was inconclusive diagnosis and comments, the slides were retrieved and reviewed. In some cases, paraffin embedded tissue blocks were retrieved from the archive and fresh sections were made by a senior laboratory Scientist. Where necessary, immunohistochemical studies were requested from the Lancet Laboratories in neighbouring Republic of South Africa for cases where haematoxylin and eosin stains alone could not provide a categorical diagnosis. The results were analyzed using Epi Info version 6.0 statistical software program.
Results
There were four hundred and forty-three histologically confirmed diagnoses of malignant female genital tract tumours at the National Health Laboratory Gaborone within the four-year study period. The mean annual distribution was 111 cases. The age of the patients ranged from 13–99 years with a mean age of presentation at 54.5 years ± 6.4(SD).
Cancer of the cervix accounted for more than two-thirds (80.6%) of all the cancers followed by uterine cancers (10.0%) and then cancers of the vulva (4.5%). A majority of the cancers presented between the 4th and 8th decades of life and rarely below the age of 30 years (Tables 1 and 2). Ovarian cancers constituted 3.4% of all the female genital tract cancers and were found more in the younger age group (Table 1).
Table 1.
Distribution of malignant female genital tract tumours by anatomical site.
| Anatomical site |
No of cases |
Per cent (%) |
| Cervix | 357 | 80.60 |
| Uterus | 44 | 10.00 |
| Vulva | 20 | 4.50 |
| Ovary | 15 | 3.40 |
| Vagina | 7 | 1.50 |
| Total | 443 | 100.00 |
Table 2.
Distribution of individual malignant female genital tract tumours by age and anatomical site
| Age (years) | Cervix | Uterus | Ovary | Vulva | Vagina |
| 10–19 | - | - | 2 | - | - |
| 2–-29 | 12 | - | 1 | - | - |
| 30–39 | 73 | 2 | 3 | 12 | - |
| 40–49 | 78 | 2 | 3 | 5 | - |
| 50–59 | 78 | 6 | 5 | 2 | - |
| 60–69 | 46 | 9 | - | - | 1 |
| 70–79 | 51 | 19 | - | 1 | 4 |
| 80–69 | 5 | 6 | 1 | - | 1 |
| 90–99 | 1 | - | - | - | - |
| Not specified | 13 | - | - | - | 1 |
| Total | 357 | 44 | 15 | 10 | 7 |
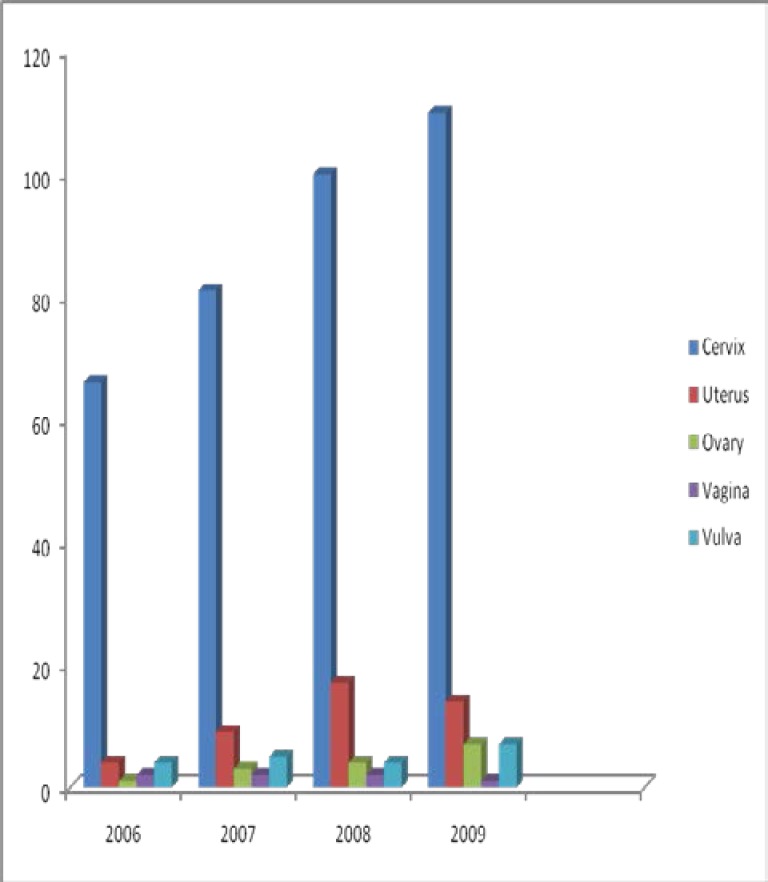
The frequency of cervical and ovarian cancers increased steadily over the four-year period, while that of uterine cancer experienced a decline in 2009. The reason for this decline is not apparent. The frequencies of vulval and vaginal cancers remained relatively unchanged over the study period (Figure 2).
Figure 2.
Yearly distributions of malignant female genital tract tumours from 2006 to 2009
Discussion
Cancers of the uterine cervix accounted for more than 80% of all malignant tumours of the female genital tract in this study. This finding is higher than the findings of previous studies in some parts of Sub-Saharan Africa. For instance, Kyari et al 1 in a hospital-based study found that cancers of the cervix constituted 70.5% of all cancers of the female genital tract in Eastern Nigeria.
Although breast cancer is the most common malignancy affecting women worldwide, cancer of the cervix is reported in many studies to be the most common non-skin malignancy of women in developing countries.19 The reason for this high frequency of cervical cancer in Sub-Saharan Africa has been attributed to lack of organized and effective screening programs. Additionally, the HIV pandemic has significantly contributed to the high incidence of cervical cancer. Epidemiological studies have shown that the risk of cervical cancer is strongly influenced by sexual activity.3,4,5 In these studies, the risk of developing cervical intraepithelial lesion in HIV-infected women is at least two to five times higher than in HIV negative women.
Although there is no evidence to date that HIV directly causes cervical neoplasia, many studies have shown that more than 90% of cervical cancer cells content high risk human papilloma virus (HPV) DNA.20 This suggests that cervical cancer may be directly linked to HPV infection. But whether HIV infection influences the course of disease has not been clearly elucidated. It has been postulated that immune suppression occasioned by HIV infection increases the risk of contracting high risk HPV by the cervical epithelial cells.
The second most common female genital tract malignancy in this study is uterine cancers which accounted for 10% of all the cancers. Although previous studies both in Nigeria and in the United Kingdom21 came to the opposite conclusion with ovarian cancers being the second most common tumours, we found however, that ovarian cancers occurred more in the younger age group as was documented in these studies. 21,22
The reason for uterine cancers being more common in this study is not immediately clear but it may be related to economic factors. Health care services are free to all Batswana and more readily accessible to all citizens. This undoubtedly increased hospital attendance. We also found that uterine cancers occurred a decade later among Batswana women than in other parts of Sub-Saharan Africa. This may be due to longer life expectancy among Batswana women prior to the HIV epidemic that ravished the country in the last one and a half decade or so. But this needs further studies.
Carcinoma of the vulva accounted for 4.5% of all the female genital tract cancers and was found almost exclusively below the fifth decade of life. This is higher than the 1.6% reported by Kyari et al. This higher incidence could be attributed to early repeated exposure to multiple sexual partners and thus high risk HPV.
Conclusion
The data presented in this study cannot be said to accurately represent community prevalence rates because cancer statistics go beyond hospital-based data. However, the data has significant implication for cancer prevention, diagnosis and management. Cancer of the cervix is high in Botswana and affects predominantly the productive age group of the society. This undoubtedly is attributed to the risk factors such as sexual habits. In Botswana, like most other countries in the region, many young girls have their sexual debut at very young age and most times it is unprotected sexual intercourse. Having multiple sexual partners is also a common practice providing high chance for contracting HPV. This has impact on the socio-economic well being of the country. According to the World population prospects (2002), life expectancy of women in Botswana has dropped from about 65 years in 1991 to 39.7 years during the HIV/AIDS pandemic. It is steadily rising again because of the high HAART coverage. Therefore more resources need to be allocated for establishing organized screening programs as a preventive measure and also to enhance accurate diagnosis and effective management of these cancers in the early stages. The practice of outsourcing and sending specimen to Republic of South Africa for confirmatory diagnosis only results in delay of establishing proper management protocol.
It is recommended that policy makers and implementers view the menace of female genital tract cancers in Botswana with special concern and special allocations be made in order to improve or establish new facilities, expertise and physician awareness at all levels of Health care delivery in Botswana. We believe this is achievable in Botswana, a country which already has a success story as the first country in Africa to have established a very successful anti-retroviral therapy program for its affected citizens.
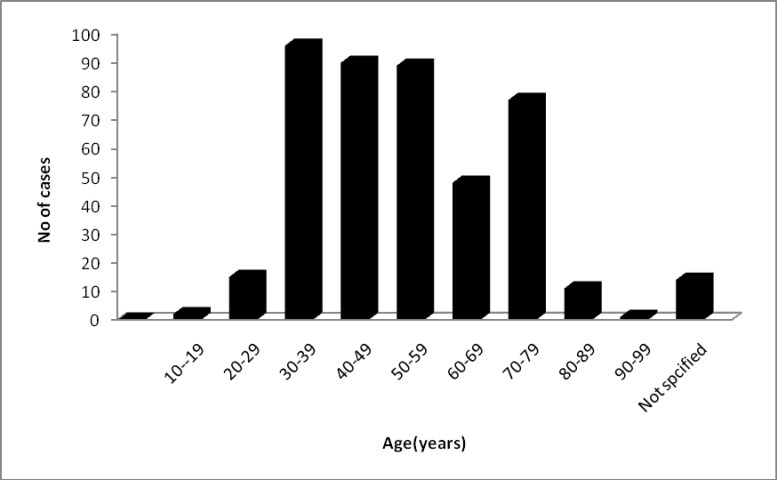
Figure 1.
Distribution of malignant female genital tract tumours by age.
There were 14 patients (3.16%) whose ages were not recorded at the time of specimen collection.
Mean age = 54.50 ± 6.40 (SD).
Acknowledgement
The authors would like to acknowledge Ms Cortinah Fani and Mr Thamiso Moinga for handling the technical aspect of this research.
References
- 1.Kyari O, Ngadda H, Mairiga A. Malignant tumours of the female genital tract in North-Eastern Nigeria. East Afr Med J. 2004;81:142–145. doi: 10.4314/eamj.v81i3.9144. [DOI] [PubMed] [Google Scholar]
- 2.Franco E L, Frano E D, Ferenczy A. Cervical cancer: epidemiology, prevention and the role of human papilloma virus infection. Canadian Med Ass J. 2001;164:1017–1025. [PMC free article] [PubMed] [Google Scholar]
- 3.Tanko NM, Echejoh GO, Manasseh AN, Mandong BM, Banwat EB, Daru PH. Cervical dysplasia in HIV seropositive women in Nigeria. Highland Medical Research Journal. 2006;4:21–26. [Google Scholar]
- 4.Fayo-Ndao MA, Diack-Mbaye A, Woto Gaye G. Cervical dysplasia in HIV infection in Senegal; Int Conf Aids; July 19–22, 1992; (8th International AIDS Conference Amsterdam) [Google Scholar]
- 5.Chirenze ZM. Association of cervical squamous intraepithelial and HIV-1 infection among Zimbabwean women in HIV/STI prevention centre. Int Journal of STD and AIDS. 2002;13:765–768. doi: 10.1258/095646202320753727. [DOI] [PubMed] [Google Scholar]
- 6.Mohammed A, Ahmed SA, Oluwole OP, Avidine S. Malignant tumours of the female genital tract in Zaria: Analysis of 513 cases. Ann Afr Med. 2006;5:93–96. [Google Scholar]
- 7.Cannistra SA, Niloff JM. Cancer of the uterine cervix. N Eng J Med. 1996;334:1030–1038. doi: 10.1056/NEJM199604183341606. [DOI] [PubMed] [Google Scholar]
- 8.Kristensen GB, Holm R, Abeler VM, Trope CG. Evaluation of the prognostic significance of cathepsin D, epidermal growth factor receptor and CerbB-2 in early cervical squamous cell carcinoma: an immunohistochemical study. Cancer. 1996;78:433–440. doi: 10.1002/(SICI)1097-0142(19960801)78:3<433::AID-CNCR9>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 9.Nair BS, Pillai R. Oncogenesis of squamous cell carcinoma of the uterine cervix. Int J Gynaecol Pathol. 1992;11:47–57. doi: 10.1097/00004347-199201000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Larsen NS. Invasive cervical cancer arising in young white females. J Natl Nacer Inst. 1994;86:6–7. doi: 10.1093/jnci/86.1.6. [DOI] [PubMed] [Google Scholar]
- 11.La Vecchia C, Franceschi S, Decarli A, Fasoli M, Gentle A, Parazinni F, Regallo M. Sexual factors, venereal diseases and the risk of intraepithelial and invasive cervical neoplasia. Cancer. 1986;58:935–941. doi: 10.1002/1097-0142(19860815)58:4<935::aid-cncr2820580422>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 12.Hawes SE, Kiviat NB. Are genital infections and inflammation cofactors in the Pathogenesis of invasive cervical cancer? J Nat Cancer Inst. 2002;94:1592–1593. doi: 10.1093/jnci/94.21.1592. [DOI] [PubMed] [Google Scholar]
- 13.Kessis TD, Slebos RJ, Han SM, Shah K, Bosch XF, Munoz N, Hedrick L, Cho KR. P53 gene mutations and MDM2 amplifications are uncommon in primary carcinomas of the uterine cervix. Am J Pathol. 1993;143:1398–1405. [PMC free article] [PubMed] [Google Scholar]
- 14.Harlow BL, Weiss Ns, Roth GJ, Chu J, Daling JR. Case-control study of borderline ovarian tumours. Reproductive history and exposure to exogenous female hormones. Can Res. 1988;48:5849–5852. [PubMed] [Google Scholar]
- 15.Lynch HT, Watson P, Bewtra C, Conway TA, Hippel CR, Kaur P, Lynch JF, Ponder BA. Hereditary ovarian cancer. Heterogeneity in age at diagnosis. Cancer. 1991;67:1460–1466. doi: 10.1002/1097-0142(19910301)67:5<1460::aid-cncr2820670534>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 16.Voigt LF, Weiss NS. Epidemiology of endometrial cancer. Cancer Treat Res. 1989;49:1–21. doi: 10.1007/978-1-4613-0867-6_1. [DOI] [PubMed] [Google Scholar]
- 17.Rose PG. Endometrial carcinoma. N Eng J Med. 1996;335:640–649. doi: 10.1056/NEJM199608293350907. [DOI] [PubMed] [Google Scholar]
- 18.Schammel DP, Mittal KR, Kaplan K, Deligdisch L, Tawassoli FA. Endometrial adenocarcinoma associated with intrauterine pregnancy: a report of five cases and a review of the literature. Int J gynaecol Pathol. 1998;17:327–335. doi: 10.1097/00004347-199810000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Olukoye AA. Cancers of the breast and cervix in Nigerian women and the role of primary health care. Nig Med Practitioner. 1989;18:26–30. [Google Scholar]
- 20.Walboomers JMM, Jacobs MV, Manos MM, Bosch FX. Human papilloma virus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1997;189:12–19. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 21.Chamberlain G, Fairly DH. Lecture notes on Obstetrics and Gynaecology. Oxford: Black well Science Ltd; 1999. Malignant Gynaecology conditions. [Google Scholar]
- 22.Onuigbo WIB. Cancer in teenagers. Nigerian J Surg Science. 1993;3:45–46. [Google Scholar]