Summary
Objectives
To describe the epidemiology and public health response to H1N1 outbreak and make recommendations to prevent future outbreaks.
Design
A descriptive study of an outbreak investigation.
Setting
A secondary school in Asante Akim South District.
Methods
Influenza A H1N1 2009 infection was laboratory-confirmed by Polymerase Chain Reaction (PCR) in clinically ill students after collecting throat swabs. Sixty students of the school had presented with fever, cough, headache and sore throat. The students' dormitories were also inspected to assess degree of ventilation and general level of cleanliness in the rooms.
Results
The outbreak followed a propagated transmission lasting 10 days with two peaks on 22nd and 24th June, 2010.The clinical attack rate was 9.9%. Secondary attack rates at the highly congested female dormitory were 28%, 31.3% and 17.8% for Rooms 1, 2 and 3 respectively. The generation time for the Influenza H1N1 a 2009 outbreak in the school was about two days.
Conclusion
A mild form of Influenza A H1N1 2009 was confirmed in a secondary school affecting mainly those in the boarding house. Cases identified were treated, but post-exposure prophylaxis with oseltamivir administered to the remaining school population actually halted the outbreak, after social distancing interventions had not succeeded.
Keywords: prophylaxis, Influenza A H1N1 2009, oseltamivir, outbreak, respiratory illness
Introduction
Before the introduction of vaccines against the Influenza A H1N1 2009 infection, early control measures included both pharmaceutical and non-pharmaceutical interventions (e.g. school closures, isolation, and quarantine), depending on the specific outbreak setting and available resources.
Different countries have had many outbreaks within schools1,4 since April 2009. In some countries2,4 closing affected schools and offering antiviral prophylaxis with oseltamivir were the initial policies.
Other countries decided to close schools when there was a marked increase in hospitalization or when school operations were affected by absenteeism3. Social distancing interventions such as school closure were among the initial means to control the epidemic spread of a novel influenza virus.5,6 The risk of disease transmission may be further reduced by antiviral prophylactic treatments such as oseltamivir.7
However, limited evidence was available concerning the effectiveness of these measures during a real outbreak8, 9, particularly in Ghana. The use of H1N1 vaccines in Ghana was limited and was targeted at health workers, persons at risk of severe disease and security personnel. Pandermix was the vaccine used in Ghana in 2010 during the mass vaccination against Influenza A H1N1 2009 virus infection.
Pandemic Influenza A H1N1 2009 was first recorded in Ghana in October, 2009 and the initial cases were mainly among persons with a recent history of travel outside the country. However in 2010, there were reports of several cases throughout the country. In the Ashanti Region, there were reported cases of acute febrile respiratory illnesses in primary schools particularly in the capital city, Kumasi and some other communities outside the capital.10
A secondary school in Ashanti Region experienced several cases of acute febrile respiratory illness among students within a few days The Medical Assistant of a local Health Centre informed the District Health Directorate on 22nd June, 2010 about suspected cases of Pandemic Influenza A H1N1 2009 virus infection at a local secondary school with fifteen students presenting with cough, fever, headache, general body pains and sore throat following their report to the health facility.
The Regional Health Directorate was also informed about the reported cases of acute febrile respiratory illness in the secondary school and a team was constituted to investigate the outbreak. The objectives of the study were to describe the epidemiology and public health response to this outbreakand make recommendations to prevent future outbreaks.
Methods
Setting
Asante Akim South District is one of 27 districts in Ashanti Region of Ghana.. It has 6 sub districts and a total population of 133,502 (projection from March 2000 census) with 16 health facilities. There are two second cycle schools in the affected sub-district, one of which reported the outbreak. The total student population in the secondary school was 608 out of which 65.6% (399) were boarding students. Males constituted 54.4% (331) of the total student population. The school had a tutorial staff of 28 teachers. There were two main dormitories in the school, the boys' and girls' dormitories that had further been sub divided into three Houses of residence each.
Definitions
The following case definitions were used for the investigation. A suspected case of pandemic Influenza A H1N1 2009 virus infection was a person (student or worker of the local secondary school) who after 1st June, 2010 developed acute febrile respiratory illness (fever, and one of the following: cough, sore throat, shortness of breath, difficulty in breathing or chest pains) with onset within 7 days of close contact with a person who is a probable or confirmed case of the new Influenza A H1N1 2009 virus infection. A confirmed case was an individual with laboratory confirmed pandemic Influenza A H1N1 2009 virus infection by Real-time RT-PCR.
Laboratory Testing
Throat swabs were taken from three suspected cases at the time the outbreak was detected. These throat swabs were collected into a Viral Transport Medium (VTM) on the 22nd June 2010. The specimens were kept in an ice box (2–8°C) with bio-safety precaution and transported to the National Public Health Laboratory in Accra within 24 hours after collection. Laboratory testing of the respiratory samples by PCR was carried out by the National Influenza Center at the Noguchi Memorial Institute for Medical Research, University of Ghana, Legon.
Screening of Students
Using the case definition, thorough screening of the students was carried out at a makeshift clinic established in the school.
Initial cases, mainly females, presented with cough, headache, fever, general malaise and sore throat. Subsequently additional cases were identified from both the girls and boys dormitories.
Records Review
The consulting room register at the local health facility and the District Hospital were reviewed, where no missed cases were detected. The housemasters' exeat (permission) records in the school were also reviewed and there was evidence of several students seeking permission to go home on health grounds though there were no central records to collate all exeats given to students over the period.
Inspection of Dormitories
The dormitories were inspected by the team to assess degree of ventilation and general level of cleanliness in the rooms.
Ethical clearance
The Regional Health Directorate of the Ghana Health Service approved the study. Informed consent was obtained from the teachers, students and Board members of the Parents Teachers Association.
Results
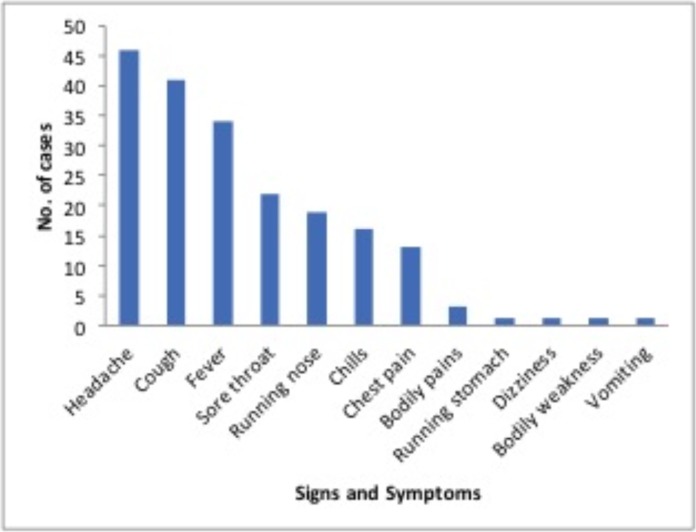
In total, there were 60 symptomatic cases with acute Influenza-like Illness. Influenza A H1N1 2009 virus infection was laboratory-confirmed by PCR with primers specific for Influenza A H1N1 2009 virus infection in all of the three samples collected from the clinically ill cases. Figure 1 shows the clinical presentation of the cases.
Figure 1.
Symptoms & Signs of Influenza A H1N1 2009 outbreak, Ashanti Region 2010
Characteristics of the Cases
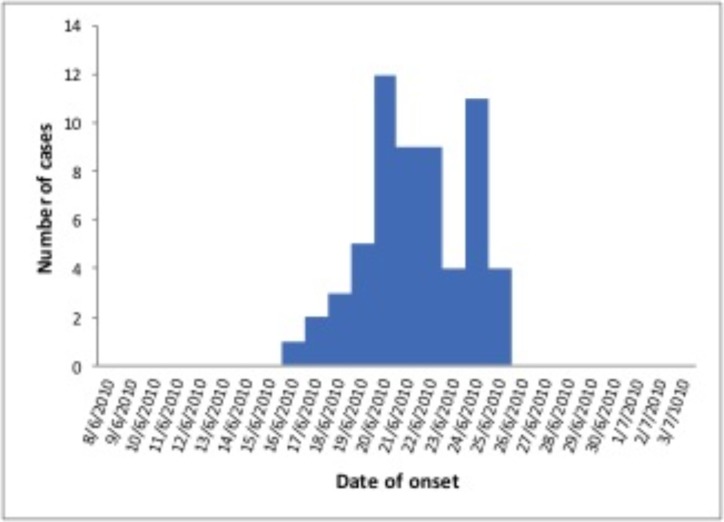
The mean age of the students meeting the case definition was 17.8 years (95% CI 17.5–18.1), with a range of 16 to 20 years, while the mean weight of the students was 53.5kg (95% CI 51.4–55.7). Females (91.7%) were more infected than males during the outbreak.The epidemic curve of the outbreak showed a propagated transmission (direct contact) with two peaks on 22nd and 24th June, 2010.
The outbreak lasted for about 10 days from 16th to 26th June, 2010, with symptoms of the index case appearing on 16th June, 2010. Interventions were initiated on 22nd June and mass post-exposure prophylaxis administered on 25th June, 2011. No other cases were recorded after 26th June, 2011. The generation time of the outbreak was estimated to be the period between the two peaks which was about two days (Figure 2).
Figure 2.
Distribution of cases of Influenza A N1H1 2009 outbreak in Ashanti Region in 2010
Attack rates
All categories of the school population and houses of residence were affected by the outbreak but in different proportions. Taking the entire school population (students and staff), there was a clinical attack rate of 9.4% (60/636). However, given that the living circumstances of the students were significantly distinct from those of members of staff, the student population was considered as the affected cohort. Among the students, the clinical attack rate was 9.9% (60/608). The secondary attack rates at the female dormitory were 28%, 31.3% and 17.8% for Rooms 1, 2 and 3 respectively. Room 2 with the highest attack rate housed the index case.
Inspection of Dormitories
The female dormitories on inspection were found to be overcrowded with closely packed beds. These beds were triple-decker and were spaced less than one metre apart. The rooms were sparsely provided with ceiling fans and most of the windows were closed.
Public Health Response
Social distancing
Thirty-seven students were initially identified as clinically ill cases and were segregated into 3 groups, the ill, moderately ill and those with mild symptoms. These symptomatic students were put in an isolated dormitory to prevent cross infection to the other students at risk. These symptomatic students, all females however did not follow the social distancing guidelines developed by the health team and ended up mixing with the non-symptomatic students during sleeping hours.
Antiviral treatment and prophylaxis
Seven cases that were initially ill were treated with osteltamivir and paracetamol on the 22nd June, 2011 while awaiting results of the throat swab collected. The other symptomatic students were later treated with oseltamivir after confirmation of Influenza A H1N1 2009 was received from the National Influenza laboratory, on 25th June, 2011 and prophylaxis given to their close contacts.
Following the identification of additional cases on 26th June, 2011, the team extended antiviral prophylaxis beyond the initial group of close contacts to all staff and students in the school. The ill students with pandemic Influenza A H1N1 2009 virus infection were treated with oseltamivir 75 mg twice daily for five days while the remaining students were offered post-exposure prophylaxis of oseltamivir 75 mg once daily for 7 days.
Information to parents and district local authorities
Parents and the District Assembly were informed about the confirmed case of Influenza A H1N1 2009 virus infection in the school and that unnecessary visits were discouraged. Information was also communicated to parents to keep day students at home if they reported ill.
Clinic at school
An assessment and collection point was established at the school to offer assessment and treatment to students and staff members.
School closure
Because immediate school closure was not an option, the following control measures were implemented particularly for boarding students: active case finding, treatment of infected students, and post-exposure prophylaxis for the rest of the school. Midterm break for the school was postponed from the 30th June, 2010 to the 5th July, 2010 for all students to complete the osteltamivir prophylaxis and also to allow the incubation period to pass without any new infection being identified.
Health Education
The teaching staff, students and community were sensitized on the mode of transmission, cardinal clinical features of H1N1 and preventive measures.
Continuous Surveillance
No additional cases were recorded since 26th June, 2010. The students returned from their mid terms on the 9th July, 2010 and no other new cases were reported extending into two incubation periods.
Discussion
This was the first major report of outbreak of pandemic (H1N1) 2009 in a residential school setting in the Ashanti Region. The index case had contact with a suspected case while visiting her parents outside the school. Our findings suggest a high transmission rate of pandemic Influenza A H1N1 2009 virus infection in a closed community which had not been reported anywhere else in the region.
The delay in notifying the surveillance system at the local level affected rapid response from the District and Regional teams. Several students had reported to school authorities with acute febrile respiratory like illness and had been given permission to go home for medical attention; however the low index of suspicion of a possible Influenza A H1N1 2009 infection among school authorities at that level could not activate a response from the surveillance system.
The outbreak peaked on 22nd June, when the school authorities finally alerted the Medical Assistant of the local health centre. The attack rate was very high among the female students probably due to the fact that the index case was a female and also a boarding student. Furthermore, the female dormitory was heavily over crowded with no proper ventilation system which gave the opportunity for easy transmission of infection among the females. Students are a well-documented source of community influenza transmission and represent markers for more widespread community transmission.11
In the early stages of a pandemic, schools with a wide geographic catchment area may therefore accelerate the spread of infection. Even though the Influenza A H1N1 2009 vaccine is currently available, antiviral prophylaxis may be considered as an additional strategy in reducing the pandemic's effects, especially in areas in which the supply of vaccine is limited. Furthermore, this strategy may be important in future epidemics and pandemics, either before vaccines are made available or when there is a poor match between the vaccine and circulating strains. In Ghana, vaccines were not available to schools due to the limited supplies.
The high congestion in some boarding school poses a greater risk of H1N1 outbreaks and therefore greater consideration need to be given them in future distribution of vaccines. Oseltamivir administration was initiated to suspected patients before laboratory confirmation of the infective organism. The favourable conditions that existed in the schools particularly in the female dormitory for fast transmission of H1N1 infection necessitated that treatment was provided to symptomatic patients without delay. This was perhaps the main reason for fewer complications in spite of high transmission rate in the school. Delay in treatment has been found to be one of the major reasons for high complications and mortality.12
Post-exposure prophylaxis has been considered in previous modeling studies and projected to be a useful measure for mitigating the spread of pandemic infections in the absence of antiviral resistance.13,14,15 In addition to being a useful measure in reducing the secondary influenza transmission in households 16,17, targeted prophylaxis has been shown to be effective in reducing the overall attack rates and in slowing disease spread in the community.15
However, despite such potential benefits, the emergence of drug resistance poses a significant threat to the effectiveness of post-exposure prophylaxis and the use of limited drug stockpiles. Available reports however do not support the presence of resistant osteltamivir strains in Ghana18 and therefore post-exposure prophylaxis becomes an appropriate intervention to halt such high transmission infections.
Most pandemic plans support the treatment of ill individuals upon diagnosis as an efficient approach to the use of drug stockpiles.19 However, the potential role of antiviral prophylaxis for asymptomatic individuals exposed to infectious cases remains contentious.
In the absence of transmissible drug-resistant viral strains, models suggest that widespread use of post-exposure prophylaxis could contain influenza epidemics, particularly if applied early.13,14 In this particular outbreak, the use of post-exposure prophylaxis was the most vital disease control intervention. Though the use of antiviral prophylaxis poses logistical challenges and could carry adverse epidemiological consequences20, 21, the Regional Health Directorate in this case had sufficient supplies of oseltamivir to contain the outbreak. At the end there were no reports of adverse events following the drug administration in contrast to other reports in Sheffield, United Kingdom22 and Magdagascar.23
Precipitating factors
Initial weak support from school authorities to enforce social distancing particularly on the first day, which allowed free mixing of isolated clinically ill students with non symptomatic colleagues.
Overcrowded nature of the dormitories, particularly the female section coupled with poor ventilation facilitated the spread of the infection.
Conclusion
Influenza A H1N1 2009 was confirmed in the school and mainly affected those at the female section of the boarding house due to the prevailing precipitating factors. The pandemic Influenza A H1N1 2009 virus infection in this outbreak was generally mild. Our study suggests that oseltamivir prophylaxis may help to contain the extent of outbreaks of Influenza A H1N1 2009 in closed settings. Mass oseltamivir prophylaxis is a therefore useful strategy to control outbreaks in enclosed locations like boarding schools where social distancing may be very difficult to implement.
Recommendations
Congestion in boarding schools must be addressed as it may facilitate the spread of various diseases particularly respiratory diseases.
The issuance of medical excuse to students on account of illness in schools needs to be coordinated so that the magnitude of disease can be determined at a point in time and outbreaks detected early
Acknowledgement
The authors thank the Bompata Sub District health team, the District and Regional Epidemic Rapid Response Teams. Special appreciation also goes to the staff of Bompata Secondary School and the Asante Akim South District Assembly.
References
- 1.Lessler J, Reich NG, Cummings DAT. Outbreak of 2009 Pandemic Influenza A(H1N1) at a New York City school. N Engl J Med. 2009;361:2628–2636. doi: 10.1056/NEJMoa0906089. [DOI] [PubMed] [Google Scholar]
- 2.Calatayud L, Kurkela S, Neave PE, Brock A, Perkins S, Zuckerman, Sudhanva M, Bermingham A, Ellis J, Pebody R, Catchpole M, Heathcock R, Maguire H. Pandemic(H1N1° 2009 virus outbreak in a school in London, April–May 2009: an observational study. Epidemiol Infect. 2010;138:183–191. doi: 10.1017/S0950268809991191. [DOI] [PubMed] [Google Scholar]
- 3.Park SY, Nakata MN, Elm JL, Ching-Lee MR, Rajan R, Giles CA, Hua H, Kanenaka MS, Ando MA, Sasaki JE, Le C, Manuzak A, Wong M, Whelan CA, Ueki R, Kunimoto G, Lee R, Gose R, Chen T, Sreenivasan MV. Outbreak of 2009 Pandemic Influenza A(H1N1) at a school - Hawaii, May 2009. MMWR. 2010;58:1440–1444. [PubMed] [Google Scholar]
- 4.Guinard A, Grout L, Durand C, Schwoebel V. Outbreak of influenza A(H1N1) without travel history in a school in the Toulouse district, France, June 2009. Euro Surveill. 2009;14:85–87. doi: 10.2807/ese.14.27.19265-en. [DOI] [PubMed] [Google Scholar]
- 5.Kelso JK, Milne GJ, Kelly H. Simulation suggests that rapid activation of social distancing can arrest epidemic development due to a novel strain of influenza. BMC Public Health. 2009;9:117. doi: 10.1186/1471-2458-9-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heymann AD, Hoch I, Valinsky L, Kokia E, Steinberg DM. School closure may be effective in reducing transmission of respiratory viruses in the community. Epidemiol Infect. 2009;137:1369–1376. doi: 10.1017/S0950268809002556. [DOI] [PubMed] [Google Scholar]
- 7. [6 June 2012]. Available from www.who.int/csr/resources/publications/swinefl/h1n1 guidelines_-pharmaceutical-mngt.pdf.
- 8.Heymann A, Chodick G, Reichman B, Kokia E, Laufer J. Influence of school closure on the incidence of viral respiratory diseases among children and on health care utilization. Pediatr Infect Dis. 2004;23:675–677. doi: 10.1097/01.inf.0000128778.54105.06. [DOI] [PubMed] [Google Scholar]
- 9.Cowling BJ, Lau EH, Lam CL, Cheng CK, Kovar J, Chan KH, Peiris JS, Leung GM. Effects of school closures, 2008 winter influenza season, Hong Kong. Emerg Infect Dis. 2008;14:1660–1662. doi: 10.3201/eid1410.080646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Annual Report. Ashanti Regional Health Directorate; 2010. [Google Scholar]
- 11.Rogelio PP, Daniel RZ, Samuel PL, Mauricio H, Franisco QF, Edgar B, et al. Pneumonia and respiratory failure from swine-origin Influenza A H1N1 2009 virus infection in Mexico. N Engl J Med. 2009;361:680–689. doi: 10.1056/NEJMoa0904252. [DOI] [PubMed] [Google Scholar]
- 12.Neuzil KM, Hohlbeinn C, Zhu Y. Illness among schoolchildren during influenza season: effect on school absenteeism, parental absenteeism from work and secondary illness in families. Arch Pediatr Adolesc Med. 2002;156:986–991. doi: 10.1001/archpedi.156.10.986. [DOI] [PubMed] [Google Scholar]
- 13.Longini IM, Jr, Nizam A, Xu S, Ungchusak K, Hanshaoworakul W, Cummings DAT, Halloran ME. Containing pandemic influenza at the source. Science. 2005;309:1083–1087. doi: 10.1126/science.1115717. [DOI] [PubMed] [Google Scholar]
- 14.Ferguson NM, Cummings DAT, Cauchemez S, Fraser C, Riley S, Meeyai A, Iamsirithaworn S, Burke DS. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature. 2005;437:209–214. doi: 10.1038/nature04017. [DOI] [PubMed] [Google Scholar]
- 15.Germann TC, Kadau K, Longini IM, Jr, Macken CA. Mitigation strategies for pandemic influenza in the United States. Proc Natl Acad Sci USA. 2006;103:5935–5940. doi: 10.1073/pnas.0601266103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Welliver R, Monto AS, Carewicz O, Schatteman E, Hassman M, Hedrick J, Jackson HC, Huson L, Ward P, Oxford JS, Oseltamivir Post-Exposure Prophylaxis Investigator Group Effectiveness of oseltamivir in preventing influenza in household contacts: a randomized controlled trial. JAMA. 2001;285:748–754. doi: 10.1001/jama.285.6.748. [DOI] [PubMed] [Google Scholar]
- 17.Hayden FG, Belshe R, Villanueva C, Lanno R, Hughes C, Small I, Dutkowski R, Ward P, Carr J. Management of influenza in households: a prospective, randomized comparison of oseltamivir treatment with or without post-exposure prophylaxis. J Infect Dis. 2004;189:440–449. doi: 10.1086/381128. [DOI] [PubMed] [Google Scholar]
- 18. [3 March 2012]. Available from http://www.who.int/influenza/gisrslaboratory/flunet/en.
- 19.Democratis J, Pareek M, Stephenson I. Use of neuraminidase inhibitors to combat pandemic influenza. J Antimicrobl Chemother. 2006;58:911–915. doi: 10.1093/jac/dkl376. [DOI] [PubMed] [Google Scholar]
- 20.Lipsitch M, Cohen T, Murray M, Levin BR. Antiviral resistance and the control of pandemic influenza. PLoS Med. 2007;4:e15. doi: 10.1371/journal.pmed.0040015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Regoes RR, Bonhoeffer S. Emergence of drug-resistant influenza virus: population dynamical considerations. Science. 2006;312:389–391. doi: 10.1126/science.1122947. [DOI] [PubMed] [Google Scholar]
- 22.Strong M, Burrows J, Stedman E, Redgrave P. Adverse drug effects following oseltamivir mass treatment and prophylaxis in a school outbreak of 2009 pandemic influenza A(H1N1) in June 2009, Sheffield, United Kingdom. Euro Surveill. 2010 May 13;15(19) pii/19565. [PubMed] [Google Scholar]
- 23.Rajatonirina S, Heraud JM, Randrianasolo L, Razanajatovo N, et al. Pandemic influenza A(H1N1) 2009 virus outbreak among boarding school pupils in Madagascar: compliance and adverse effects of prophylactic oseltamivir treatment. J Infect Dev Ctries. 2011 Mar 21;5(3):156–162. doi: 10.3855/jidc.1318. [DOI] [PubMed] [Google Scholar]