Abstract
The second branchial cleft cyst may arise anywhere from the tonsillar fossa to the supraclavicular area. It usually lies along the anterior border of the sternocleidomastoid muscle or deep into the muscle. Occurrence of the second branchial cleft cyst in the parapharyngeal space is extremely uncommon. We report one such case of second branchial cleft cyst arising from the parapharyngeal space and discuss its differential diagnosis and treatment modalities in detail.
Background
Branchial cleft cysts are the most common neck masses in adults. Mostly these cysts arise from second branchial cleft and occur in the neck, anterior to the sternocleidomastoid muscle at the mandibular angle.1 Rarely these cysts may be present in the parapharyngeal space. The parapharyngeal space is a deep potential neck space, with inverted pyramid in shape and extends from the base of the skull to the hyoid bone below. The parapharyngeal space is divided into two parts by styloid process and its attachments. The preoperative differentiation between the prestyloid and poststyloid lesion is important not only for differential diagnosis but also to guide for the best surgical approach. We report a rare case of prestyloid parapharyngeal branchial cyst being excised via a transcervical approach without any complications.
Case presentation
A 35-year-old woman presented with symptoms of gradual onset, progressive difficulty in swallowing and heaviness in throat for 5 months. She had received antibiotics and anti-inflammatory drugs for these complaints at a local facility, with no relief in symptoms. After oropharyngeal examination, we observed a fluctuating mass on the left lateral pharyngeal wall pushing the left tonsil anteriorly, extending till the midline and covered with normal mucosa. Neurological symptoms were absent and cranial nerve examination was normal.
Investigations
Axial images of contrast-enhanced MRI neck revealed a 54 mm×34 mm×23 mm well-defined, homogeneous, cystic mass in the left parapharyngeal space, displacing the carotid sheath/its structures on the posterolateral side (figure 1). The cystic mass was compressing the left tonsil anteriorly causing severe narrowing of oropharyngeal passage. Vertically, the cyst extended from the skull base to the hyoid bone level as represented on magnetic resonance coronal images (figure 2). The mass showed T1 and T2 hyperintense contents with no evidence of fat suppression. No significant postcontrast enhancement was seen. The surrounding muscle/fat planes and ipsilateral parotid gland were normal. Fine needle aspiration cytology of the cystic mass showed a variable number of mature squamous cells, few acellular squamous and cellular debris in a proteinaceous background. A preoperative diagnosis of a benign cystic lesion possibly a branchial cleft cyst was entertained.
Figure 1.
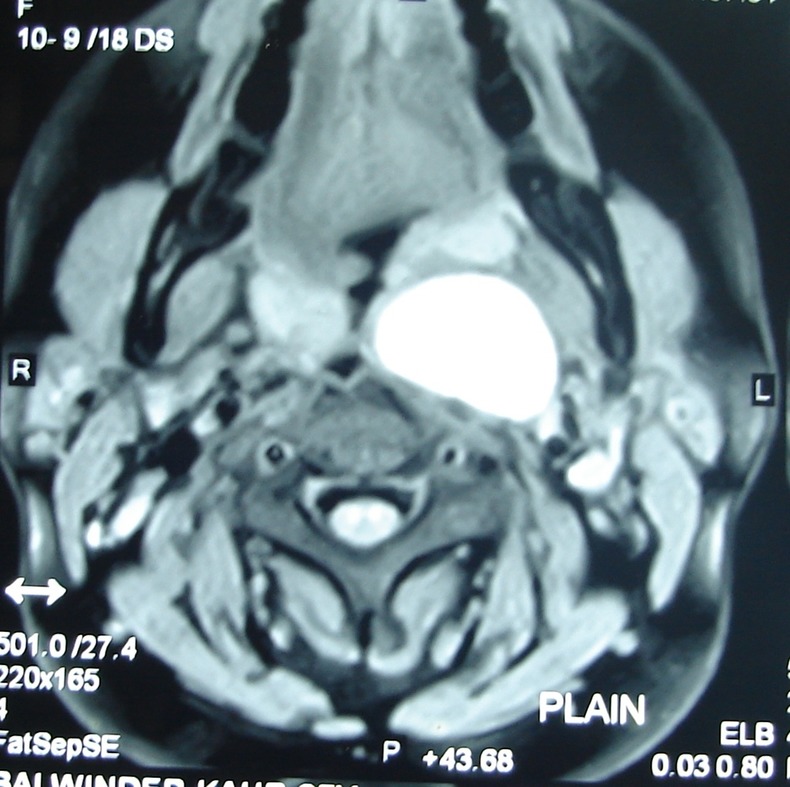
Axial section of contrast-enchanced MRI scan, showing a 54 mm×34 mm×23 mm cystic mass in the left parapharyngeal space.
Figure 2.
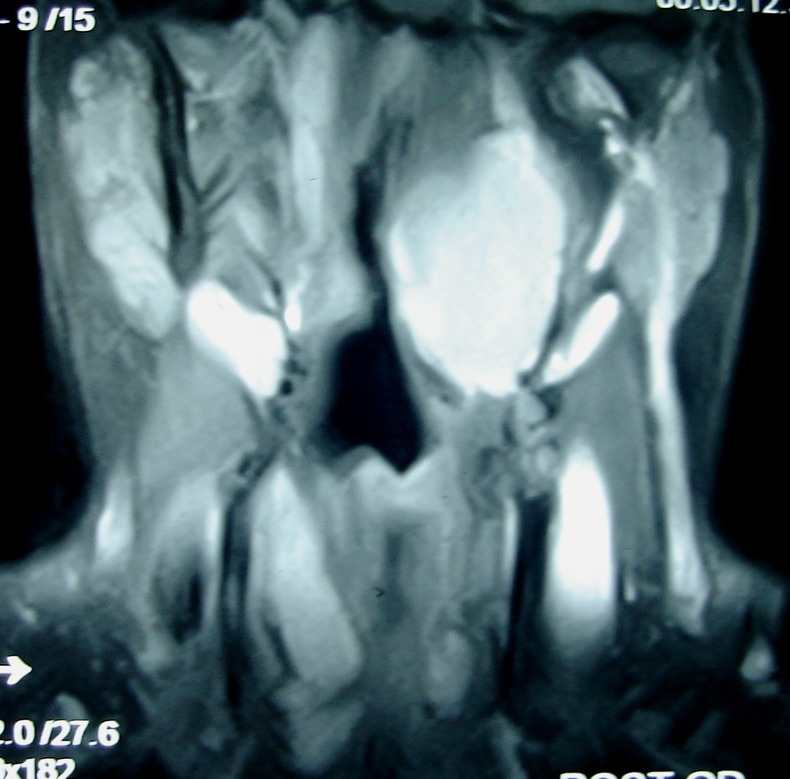
Coronal section of contrast-enchanced MRI scan showing the same cyst occupying the left parapharyngeal space from below the skull base to the hyoid bone with severe narrowing of oropharyngeal passage.
Differential diagnosis
The other possibilities which were considered in such a clinical presentation included parapharyngeal Schwannomas with cystic degeneration, minor salivary gland tumours and rarely carotid artery anomalies. However such cases can be easily identified on the radioimaging, as the former two masses are rarely completely cystic and have good enhancement of the solid portion. Furthermore, the origin of the lesion, whether from within the carotid space (Schwannomas) or within the prestyloid parapharyngeal space (minor salivary gland tumours) and their differential enhancement on T1/T2-weighted images helps narrow down the odds of the correct preoperative diagnosis. The paragangliomas are hypervascular lesions and show arterial enhancement on contrast-enhanced CT (CECT). The loss of fat plane between the mass and the parotid gland suggests a mass arising from the deep lobe of parotid, like pleomorphic adenoma. The carotid body tumour typically splays the carotid bifurcation, the vagal Schwannoma will displace the internal jugular vein laterally and internal carotid artery medially, while the Schwannoma from cervical sympathetic chain will displace carotid sheath structures anteriorly. The metastatic lymph node in parapharyngeal space are usually multiple with periadenitis or extranodal extension and often evident primarily. Lymphangiomas usually present in early childhood and show the signal intensity of a multiloculated cystic lesion on MRI.
Treatment
Total excision of the neck mass was performed via a transcervical submandibular approach. A 5 cm×3 cm×2 cm, well-circumscribed, whitish ovoid mass was identified and removed from the left parapharyngeal space (figure 3).
Figure 3.

Intraoperative picture showing white shining cyst being removed completely with its attached fibrosed duct.
Outcome and follow-up
After gross examination the mass was cystic and contained thick whitish pus. Histopathological evaluation of the mass revealed a stratified squamous epithelial-lined fibrocollagenous cyst wall with lymphoid infiltrate, consistent with a branchial cleft cyst. The mass was identified as an infected second branchial cleft cyst.
Discussion
Second branchial cleft remnants account for the majority of branchial cleft abnormalities. During the embryonic stage, the second arch overgrows the second, third and fourth branchial clefts resulting in expansion of the second branchial cleft into an elongated common cavity, called the cervical sinus of His, which is obliterated shortly after its formation. Diverse degrees of incomplete closure of the sinus lead to various anomalies of the second branchial cleft.1 Anomalies occur anywhere along a distinct tract extending from the outer opening at the anterior border of sternocleidomastoid (junction of the middle and lower third), passing between the internal and external carotid arteries, superficial to cranial nerves IX and XII and entering the tonsillar fossa.2
Bailey classified second branchial cysts into four types.3 Type I presents below the platysma and cervical fascia, anterior to the sternocleidomastoid muscle. Type II is the most common and arises from persisting cervical sinus. They typically lie on the great vessels of the neck. The type III cyst courses between the internal and external carotid arteries and extends to the lateral wall of the pharynx. The type IV cyst, a columnar-lined cyst lying against the pharyngeal wall, is thought to form from a remnant of the pharyngeal pouch.
The parapharyngeal space is a very rare location for a branchial cleft cyst. This rare location superior to the tonsillar fossa can best be explained by the fact that a second branchial cleft cyst can have an associated tract that passes to the palatine tonsil. Because this tract passes through the caudal parapharyngeal space, cysts that occur in this location are usually classified as second cleft anomalies.4
The parapharyngeal space may be divided into two compartments on the basis of its relationship to the styloid process. The prestyloid compartment contains the minor or ectopic salivary gland, branches of the mandibular division of the trigeminal nerve, internal maxillary artery, ascending pharyngeal artery and pharyngeal venous plexus, whereas poststyloid compartment contains the internal carotid artery, internal jugular vein, cranial nerves IX–XII, cervical sympathetic chain and glomus bodies.5
Parapharyngeal cysts expand to the least-resistant soft tissue planes, appear as submucosal lateral pharyngeal masses protruding intraluminally into oropharynx medially, or extend to the skull base superiorly. The most common symptom on presentation is of heaviness of throat because of a bulge in the pharynx. Palsy of cranial nerves IX, X, XI or XII is rarely seen in benign tumours or cysts. Presence of palsy may suggest direct infiltration by local malignancies, metastatic lymph nodes or mechanical compression of nerves because of marked enlargement of the cyst following superimposed infection.6 When the infection advances to abscess formation, it must be drained or it will rupture spontaneously.
Imaging is done to differentiate primary parapharyngeal space lesions from more common, deep lobe parotid lesions that have infiltrated the space secondarily to decide the suitable surgical approach.7 An MRI can accomplish this by revealing the fat plane between the normal parotid gland and a mass arising from the parapharyngeal space.
The differential diagnosis of a parapharyngeal mass includes cystic Schwannomas and minor salivary gland tumours. The anteromedial displacement of the internal carotid artery is present with Schwannomas suggesting an origin within the carotid space.8 Pleomorphic adenomas originating within the prestyloid parapharyngeal space show heterogeneous, intermediate signal intensity on T1-weighted images and intermediate-to-high signal intensity on T2-weighted images, thus differentiating from hyper-intense branchial cleft cyst, even though they also posteriorly displace the internal carotid artery.7 8 Additionally, the complete cystic change is very rare in pleomorphic adenoma and Schwannoma.
Different conservative methods have been used in the treatment of branchial cysts: a repeated aspiration of the cystic fluid, incision and drainage, marsupialisation and injection of sclerosing agents. These methods give only temporary relief in symptoms because these cysts often recur and ultimately require surgery.9
The transoral or transpalatal route is used in selected anteriorly placed cysts that are not palpable in the neck or parotid region.10 Four approaches through the external route are available: the submandibular route, total parotidectomy with retromandibular dissection, a combination of the above with a mandibulotomy and a midline mandibulotomy. The mandibulotomy approach may cause injury to the inferior alveolar nerve or teeth and may require tracheotomy. Moreover, 80% of parapharyngeal space lesions are benign; thus the route of surgical removal should carefully consider the morbidity or potential adverse results from the surgical procedure itself.11 12 Thus, these various approaches are to be used judiciously depending upon the nature, location, extent and vascularity of the mass.
Learning points.
The differential diagnosis of a cystic lesion within the parapharyngeal space should include an atypical second branchial cleft cyst.
Complete surgical excision is the treatment of choice for preventing recurrence and the transcervical submandibular approach provides the most complete exposure.
Footnotes
Contributors : MG is the ENT surgeon who has diagnoised and managed the patient along with valuable inputs from MG in case management and drafting this manuscript. Both the authors have critically analysed the text, images and contributed significantly in shaping the final manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Choi SS, Zalzal GH. Branchial anomalies: a review of 52 cases. Laryngoscope 1995;2013:909–13 [DOI] [PubMed] [Google Scholar]
- 2.Papay FA, Kalucis C, Eliachar I, et al. Nasopharyngeal presentation of second branchial cleft cyst. Otolaryngol Head Neck Surg 1994;2013:232–4 [DOI] [PubMed] [Google Scholar]
- 3.Bailey H. Branchial cysts and other essays on surgical subjects in the facio-cervical region. London: Lewis, 1929 [Google Scholar]
- 4.Som PM, Brandwein MS, Silvers A. Nodal inclusion cysts of the parotid gland and parapharyngeal space: a discussion of lymphoepithelial, AIDS-related parotid, and branchial cysts, cystic Warthin's tumors, and cysts in Sjogren's syndrome. Laryngoscope 1995;2013:1122–8 [DOI] [PubMed] [Google Scholar]
- 5.Shin JH, Lee HK, Kim SY, et al. Imaging of parapharyngeal space lesions: focus on the prestyloid compartment. Am J Roentgeol 2001;2013:1465–70 [DOI] [PubMed] [Google Scholar]
- 6.Shin JH, Lee HK, Kim SY, et al. Parapharyngeal second branchial cyst manifesting as cranial nerve palsies: MR findings. Am J Neuroradiol 2001;2013:510–12 [PMC free article] [PubMed] [Google Scholar]
- 7.Som PM, Sacher M, Stollman AL, et al. Common tumors of the parapharyngeal space: refined imaging diagnosis. Radiology 1988;2013:81–5 [DOI] [PubMed] [Google Scholar]
- 8.Tom BM, Rao VM, Guglielmo F. Imaging of the parapharyngeal space: anatomy and pathology. Crit Rev Diagn Imaging 1991;2013:315–56 [PubMed] [Google Scholar]
- 9.Bilgen C, Ogut F, Celtiklioglu F. A new case of a branchial cyst of the parapharyngeal space. ENT 2001;2013:387–9 [PubMed] [Google Scholar]
- 10.Guneri A, Gunbay MU, Guneri EA, et al. Management of parapharyngeal space cysts. J Laryngol Otol 1994;2013:795–7 [DOI] [PubMed] [Google Scholar]
- 11.Malone JP, Agrawal A, Schuller DE. Safety and efficacy of transcervical resection of parapharyngeal space neoplasms. Ann Otol Rhinol Laryngol 2001;2013:1093–8 [DOI] [PubMed] [Google Scholar]
- 12.Cohen SM, Burkey BB, Netterville JL. Surgical management of parapharyngeal space masses. Head Neck 2005;2013:669–75 [DOI] [PubMed] [Google Scholar]


