Abstract
A 48-year-old man presented with long-standing symptoms of major depression in the absence of markedly abnormal neurological findings or structural brain alterations. Antidepressive treatment, including medication and psychotherapy, had not led to significant improvement. The EEG, cerebrospinal fluid (CSF) analysis, fluorodeoxyglucose-positron emission tomography and neuropsychological testing showed pathological findings. An epileptic state provided further evidence for an organic encephalopathy. Extensively elevated thyroid-antibodies in the serum and CSF, as well as the rapid and sustained recovery after intravenous treatment with prednisolone, pointed to the diagnosis of a primarily psychiatric manifestation of a steroid responsive encephalopathy associated with autoimmune thyroiditis (SREAT).
Background
Hashimoto's encephalopathy commonly presents with neurological signs such as cognitive impairment, seizures, delirium or stroke-like symptoms. Here, we describe the case of a 48-year-old man who initially, and for a long period of time, presented only with symptoms of major depression which resolved rapidly under steroid treatment.
Case presentation
The successful 48-year-old pharmacist stopped working in spring 2002 after having gradually developed a depressed mood, anxiety, tiredness, disturbed sleep and difficulty in concentrating. He was described as slightly disorganised and behaved more aggressive towards his wife and children. Routine diagnostics and cranial CT were normal. Apart from recurrent deep venous thromboses, his somatic and psychiatric history was empty. Within 1 year, his condition deteriorated to an extent that involuntary hospitalisation was ordered by a court due to acute suicidal tendencies. In the local psychiatric hospital, the diagnosis of depression was confirmed and antidepressive treatment with citalopram was started. After 3 weeks without response, he was transferred to our University Department for further evaluation and treatment.
Investigations
On admission in April 2003, the clinical examination was normal, except for pronounced diaphoresis and a slight tremor of the upper extremities. The patient's mood was depressed and he complained of slight concentration and memory difficulties. After around 30 min of coherent conversation, he surprisingly insisted of having been hospitalised since 1 year. A clock drawing test was abnormal (figure 1A).
Figure 1.
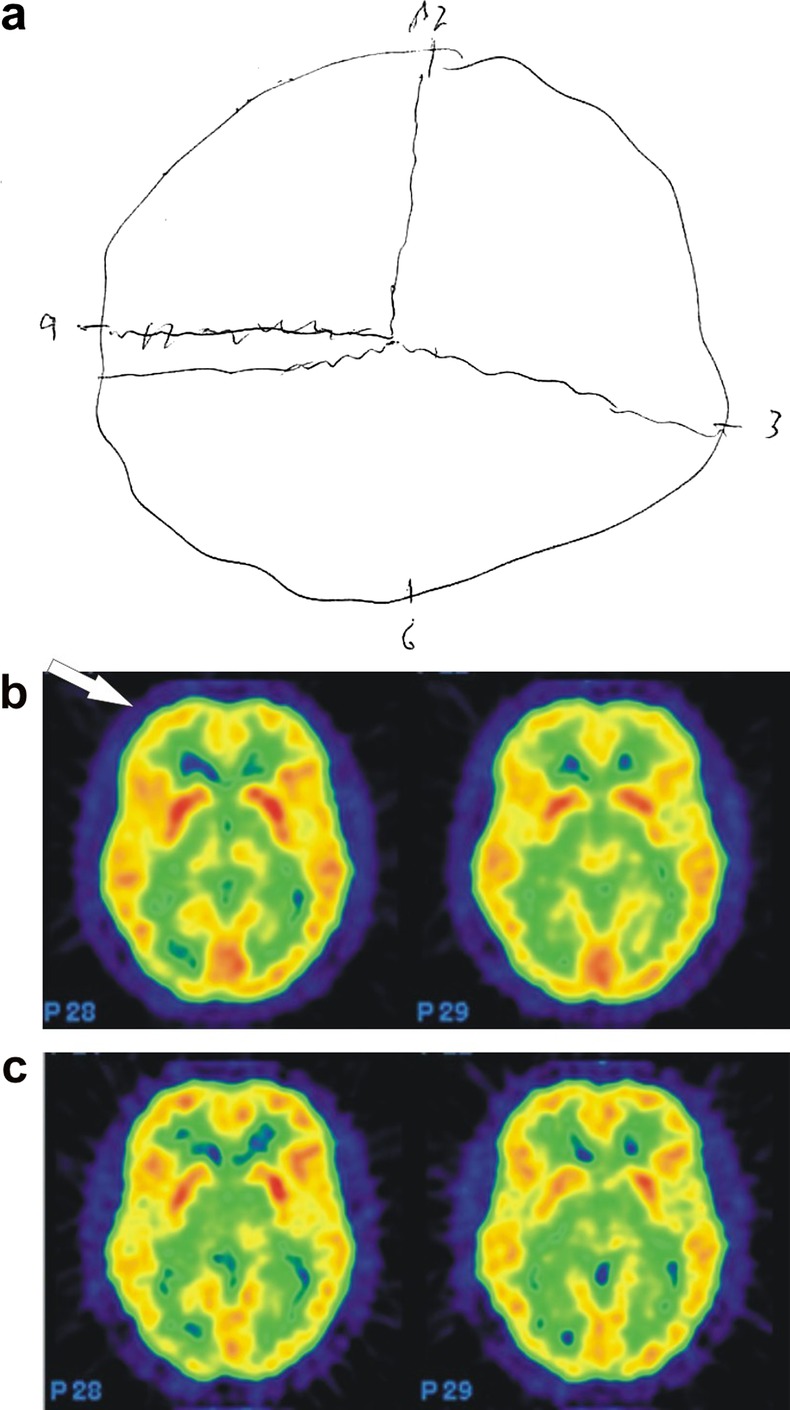
Clock drawing test and positron emission tomography (PET) of the brain. (A) Patient's attempt to draw a clock showing ‘10 min past 11’. (B) PET before treatment showing frontal and fronto-basal hypometabolisms (arrow). (C) Normalised PET of the same region 4 months after treatment and clinical remission.
The EEG showed a generalised slowing and dysrhythmic theta activity. Protein was moderately increased in the cerebrospinal fluid (960 mg/l) with normal cell count and electrophoresis. Antinuclear antibodies and protein 14-3-3 were negative. MRI of the brain revealed a slight enhancement in the fronto-parietal white matter. N-acetyl-aspartate and myoinositol, markers for neuronal integrity, were decreased in the magnetic resonance spectroscopy in voxels of the parietal and occipital-parietal cortices. Frontal and fronto-basal hypometabolisms were found in 18F-fluoro-d-glucose positron emission tomography (figure 1B). Neuropsychological testing, including the Consortium to Establish a Registry for Alzheimer's Disease (CERAD) and Trailmaking Tests, revealed impaired memory, attention and visual-spatial performance.
The clinical course was complicated by an epileptic state requiring transient intensive care treatment. Thyroid peroxidase (TPO) antibodies were >3000 U/ml (normal range 0–200) and thyroglobulin (TG) antibodies were 1370 U/ml (normal range 0–200). The patient had no history of thyroid disorder and all other thyroid parameters, ultrasound, thyroid scan and fine needle biopsy were normal.
Differential diagnosis
As described above, the initial major differential diagnosis was major depression. The ineffectiveness of standard treatment and the occurrence of neuropsychological symptoms led to further investigation of different forms of organic encephalopathy. The excessive elevation of thyroid-related antibodies pointed to the diagnosis of SREAT. Critically, previous descriptions of this syndrome have focused primarily on neurological symptoms. Relevant differential diagnoses would comprise Creutzfeldt-Jakob disease, different types of dementia and limbic encephalitis.1
Treatment
Following treatment guidelines, the intravenous treatment with prednisolone 150 mg over 3 days caused an impressive and rapid clinical recovery.
Outcome and follow-up
EEG, PET (figure 1C), MR-spectroscopy and neuropsychological testing returned to normal. The thyroid-related antibodies decreased slowly without reaching normal levels (November 2011: TPO antibodies 962 U/ml, TG antibodies 238 U/ml). Prednisolone was gradually reduced to 5 mg and supplemented with azathioprine. The patient has now remained in remission for 9 years.
Discussion
Hashimoto's encephalopathy (HE) is a rare but possibly underdiagnosed disorder characterised by high serum antithyroid antibody levels together with signs of encephalopathy.2 In our case, functional neuroimaging revealed distinct cortical dysfunction and possible neuronal damage in the absence of pronounced MRI findings and might reflect autoimmune vasculitis.3 Antithyroid antibodies remained elevated many years after clinical remission, suggesting that additional processes are implicated in the pathophysiology of this disorder which should therefore be named more precisely ‘Steroid-responsive encephalopathy associated with autoimmune thyroiditis’ (SREAT).4 Our report re-emphasises the potential of a primarily psychiatric manifestation of SREAT5 even in the absence of obvious neurological symptoms or thyroid pathology.
Learning points.
Consider steroid-responsive encephalopathy associated with autoimmune thyroiditis as a differential diagnosis for various psychiatric syndromes, including depression.
Pay specific attention to discrete neurological impairments in patients with psychiatric syndromes.
Keep immunomodulatory medication in mind for the treatment of atypical psychiatric syndromes.
Footnotes
Contributors: ClN, MB and ChN were responsible for the clinical evaluation and the treatment of the patient. All authors discussed the case and conceptualised the manuscript. ClN, LF and ChN prepared the manuscript and all authors approved the final draft of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Mocellin R, Walterfang M, Velakoulis D. Hashimoto's encephalopathy: epidemiology, pathogenesis and management. CNS Drugs 2007;2013:799–811 [DOI] [PubMed] [Google Scholar]
- 2.Chong JY, Rowland LP, Utiger RD. Hashimoto encephalopathy: syndrome or myth? Arch Neurol 2003;2013:164–71 [DOI] [PubMed] [Google Scholar]
- 3.Nolte KW, Unbehaun A, Sieker H, et al. Hashimoto encephalopathy: a brainstem vasculitis? Neurology 2000;2013:769–70 [DOI] [PubMed] [Google Scholar]
- 4.Castillo P, Woodruff B, Caselli R, et al. Steroid-responsive encephalopathy associated with autoimmune thyroiditis. Arch Neurol 2006M;2013:197–202 [DOI] [PubMed] [Google Scholar]
- 5.Cohen L, Mouly S, Tassan P, et al. A woman with a relapsing psychosis who got better with prednisone. Lancet 1996;2013:1228 [Google Scholar]


