Abstract
Vesicocutaneous fistulas (VCF) are a rare complication of radical radiotherapy to the pelvis. Timely diagnosis and management are often difficult and complex. We report the unusual case of a 64-year-old gentleman who presented to the emergency department with worsening sepsis and profuse discharge from a cutaneous opening in the left groin. This presentation was 6 weeks following the completion of external beam radiotherapy for apical margin-positive prostate cancer (pT3a). A diagnosis of a VCF was confirmed after CT scanning of the abdomen and pelvis with contrast. Urinary diversion was achieved by a temporary urethral catheter insertion. Full resolution of this gentleman's symptoms was accomplished. In this article, we present a non-invasive approach to the management of VCF. This case raises intricate management issues in the atypical development of an early urinary tract fistula postradiotherapy.
Background
Vesicocutaneous fistulas (VCF) are a very rare complication following radiotherapy for prostate cancer. The condition is infrequently reported in the literature. Early diagnosis and management are difficult and complicated. Thus, every case reported will aid our knowledge of the condition.
Case presentation
A 64-year-old construction worker presented to the accident and emergency department with fevers and a copious discharge from a cutaneous opening in his left groin. This was 6 weeks following completion of adjuvant external beam radiotherapy after a radical retropubic prostatectomy for margin-positive prostate cancer (pT3a). He had no urinary voiding difficulties. On examination, he was feverish and systemically unwell. There was a large (1 cm×0.5 cm) wound in the left groin (figure 1). The surrounding skin was inflamed and macerated. Profusely exudating from the site was straw coloured fluid with some blood staining. Over the previous weeks, he had become progressively lethargic and had noticed increasing groin discomfort aggravated by micturition. He subsequently developed boggy groin swellings.
Figure 1.

Left groin large (1 cm×0.5 cm) superficial opening of a vesicocutaneous fistula tract in the left groin.
Investigations
Full blood count showed a neutrophilia. Serum renal function tests were normal. Urinalysis suggested the presence of infection. Cross-sectional imaging with a CT scan of the abdomen and pelvis with contrast demonstrated a communication between the bladder and the cutaneous openings (figure 2). There was no obvious tumour recurrence. A diagnosis of a VCF was made.
Figure 2.

Transverse CT scan of the pelvis and upper legs. Demonstration of the collection in the left upper leg and vesicocutaneous fistula.
Treatment
He was started on parenteral intravenous antibiotics to treat sepsis. A urethral catheter was inserted to divert urine and encourage groin wound healing. The patient was reviewed at regular intervals in the outpatient clinic for catheter change and meticulous wound packing. Within 3 months, the cutaneous openings of the fistulous tract had completely healed over by secondary intention and the urinary leak ceased. MRI pelvis with fistula protocol was performed to confirm this. No evidence of perianal or groin fistulae was seen. The catheter was removed.
Outcome and follow-up
However, 6 weeks later, he re-presented with symptoms identical to his first presentation. Again, a similar management strategy was immediately put into effect, with urinary catheterisation for diversion and drainage, and starting of antibiotic therapy. This patient was strongly opposed to the idea of surgical intervention. They elected to have a trial of non-operative management, and catheterisation was continued as above.
Again, the patient's wounds healed within 3 months of urethral catheter insertion. However, the catheter remained in situ for a further 1 year. For a second time, MRI pelvis with fistula protocol was performed and the fistulae appeared to be fully healed (figure 3). There has been no recurrence of the fistulae to date.
Figure 3.
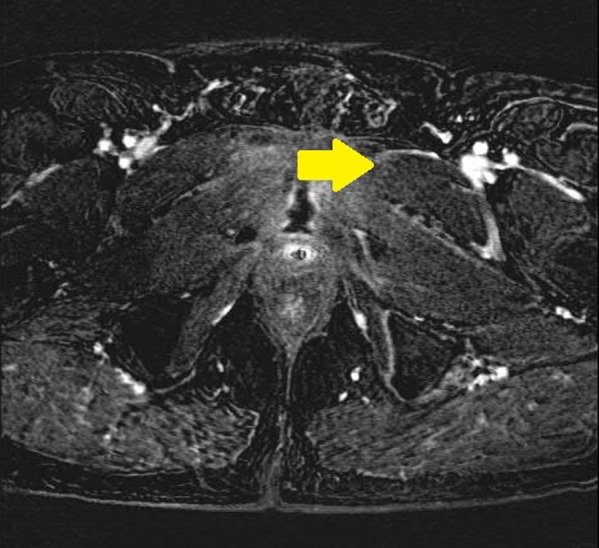
Transverse MRI pelvis with fistula protocol MRI after prolonged catheterisation demonstrating resolution fistula tract.
Discussion
The debate over the utility of adjuvant radiotherapy in treating men with prostate cancer who have undergone radical prostatectomy with adverse prognostic indicators has raged for decades. Evidence is now mounting that adjuvant radiotherapy improves survival for men with pT3 prostate cancer, a prostate-specific antigen (PSA) level greater than 10 ng/mL before radical retropubic prostatectomy (RRP) or extra-capsular extension without infiltration of the seminal vesicles.1 A recent randomised control trial has demonstrated that adjuvant radiotherapy within 18 weeks of surgery significantly reduced the risk for PSA recurrence and metastasis and significantly increased survival, compared with a wait-and-see approach to radiotherapy. For men with undetectable PSA postoperatively and pT3 disease, the 5-year biochemical progression-free survival was 72% in the group treated with adjuvant radiation therapy and 54% in the wait-and-see group.1 It is now expected that more men will be offered adjuvant radiotherapy post RRP. It is quite likely that there will be an increase in the associated complications of adjuvant radiotherapy. To our knowledge, we are the first to report the non-operative management of early VCF related to adjuvant radiotherapy for pT3 prostate cancer in the literature.
Fistula formation following radiotherapy for prostate cancer is rare but has been reported in approximately 0.3–3% of patients after brachytherapy2 and in 0–0.6% of those treated with external beam radiotherapy (EBRT).3 This outcome is classified as a grade 4 complication according to the toxicity criteria of the Radiation Therapy Oncology Group. The majority of fistulas reported in the literature are rectourethral and rectovesical (RVF). The occurrence of VCF is extremely infrequent.3 4 The mean duration from radiation to the onset of symptoms of a fistula is 32 months for RVF and between 36 and 49 months for VCF.3 Fistula formation following radiation therapy is thought to be related to progressive microvascular injury and stromal fibrosis, resulting in mucosal erosions, ulcers and perforations.3 This case is the first to report early fistula formation postadjuvant radiotherapy.
The main principle in the management of urinary fistula is to keep the bladder void, thereby preventing any raised intravesical pressure and urinary leakage. Various surgical options for fistula management have been reported.5 Factors influencing the type surgical procedure chosen include anatomic level of the fistula, underlying predisposing factors for VCF development, presence of malignancy and baseline patient performance status.6 VCF may be repaired in a one-stage procedure (fistulectomy) with or without cystoscopic assistance. Placement of an interposing myocutaneous or omental flap to aid wound healing is recommended. In the setting of radiation-induced VCF, urinary diversion procedures are the mainstay of management, whether conservative or surgical.5 In relatively fit patients, like this 64-year-old gentleman, a primary surgical repair may be tempting. However, a safe reconstructive procedure cannot be guaranteed in such circumstances. Tissue healing in a previously irradiated field will be severely compromised and surgery is likely to result in further morbidity.7 Furthermore, following external beam radiotherapy and a history of recent surgery, pelvic tissue planes would be difficult to discern. The operative choice in this case would be diversion with ileal conduit with cystectomy.8 This option was discussed with the gentleman in our case, but he refused radical treatment in favour of a wait-and-see approach. In this report, the patient had complete resolution of his symptoms within 1 year of indwelling urethral catheterisation, thereby avoiding a potentially morbid operation.
Despite the successful resolution of symptoms in this case, we cannot advocate this approach for all patients, and it is clear that the treatment of VCF must be tailored to the patient's need after careful consideration of their physical condition and disease status.
Learning points.
Vesicocutaneous fistulas (VCF) are a rare complication of radical radiotherapy to the pelvis.
It can present with profuse discharge from cutaneous openings in both groins.
Following radiation therapy is thought to be related to progressive microvascular injury and stromal fibrosis.
Conservative treatment appears to be unsuccessful, unless there is permanent bladder drainage with a urethral catheter.
Surgical management includes fistulectomy with or without cystoscopic assistance and placement of an interposing myocutaneous or omental flap or ileal conduit diversion.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Wiegel T, Bottke D, Steiner U, et al. Phase III postoperative adjuvant radiotherapy after radical prostatectomy compared with radical prostatectomy alone in pT3 prostate cancer with postoperative undetectable prostate-specific antigen: ARO 96-02/AUO AP 09/95. J Clin Oncol 2009;2013:2924–30 [DOI] [PubMed] [Google Scholar]
- 2.Stone NN, Stock RG. Complications following permanent prostate brachytherapy. Eur Urol 2002;2013:427–33 [DOI] [PubMed] [Google Scholar]
- 3.Huang EH, Pollack A, Levy L, et al. Late rectal toxicity: dose-volume effects of conformal radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys 2002;2013:1314–21 [DOI] [PubMed] [Google Scholar]
- 4.Moreira SG, Seigne JD, Ordorica RC, et al. Devastating complications after brachytherapy in the treatment of prostate adenocarcinoma. BJU Int 2004;2013:31–5 [DOI] [PubMed] [Google Scholar]
- 5.Lentz SS, Homesley HD. Radiation-induced vesicosacral fistula: treatment with continent urinary diversion. Gynecol Oncol 1995;2013:278–80 [DOI] [PubMed] [Google Scholar]
- 6.Meng E, Chuang F, Wu S, et al. Fistula involving urinary bladder: experience with the management of 23 cases. J Urol ROC 2004;2013:121–5 [Google Scholar]
- 7.Lau KO, Cheng C. A case report—delayed vesicocutaneous fistula after radiation therapy for advanced vulvar cancer. Ann Acad Med Singapore 1998;2013:705–6 [PubMed] [Google Scholar]
- 8.Chrouser KL, Leibovich BC, Sweat SD, et al. Urinary fistulas following external radiation or permanent brachytherapy for the treatment of prostate cancer. J Urol 2005;2013:1953–7 [DOI] [PubMed] [Google Scholar]


