Abstract
The aim of the paper is to report the case of a boy affected by cystic fibrosis, with non-ABPA-related recurrent wheezing and frequent pulmonary exacerbation during childhood, who had been inhaling 7% NaCl+0.1% hyaluronic acid (HA) as a maintenance therapy. We reviewed patient database and, analysing a 7-year follow-up, considered pulmonary exacerbation, antibiotic and steroid courses, pulmonary function (forced expiratory volume in one second; FEV1) and microbiological data. After starting 7% NaCl+0.1% HA treatment, we observed a dramatic decrease of oral antibiotic need (0.55 courses/month during the pretreatment period against 0.10 courses/month in the treatment period), associated with a good initial recovery and a stability of FEV1. In our opinion this case could suggest an extended indication for inhaled 7% NaCl+0.1% HA use in CF, not only in patients who did not tolerate hypertonic saline, but also in patients with coexistent asthma-like symptoms.
Background
Cystic fibrosis (CF) is a genetic disorder caused by a defective chloride-ion transport protein, CF transmembrane conductance regulator (CFTR), which causes the production of thick mucus secretions, especially in the lungs.1 CFTR mutations lead to decreased airway surface liquid (ASL) and mucociliary clearance deficiency.2 Many studies demonstrated that inhaled hypertonic saline (HS) improves lung function in CF,3 4 accelerating mucociliary clearance and expanding ASL. Cough, bronchospasm and throat irritation are some of the adverse events described after HS inhalation: these could significantly reduce treatment compliance.5
Hyaluronic acid (HA) is a polysaccharide present in human tissues; inhaled HA has been tested not only in CF but also in asthma.6 HA blocks acute bronchoconstriction caused by neutrophil elastase7 and, regulating fluid balance in the lung interstitium, facilitates ventilation and gas exchange. In addition, the inhaled solution of HS+0.1% HA has a higher pleasantness compared with HS alone.8
Wheezing is a common occurrence in people with CF, but no guidelines have been postulated about the clinical management of this case category. In addition, HA treatment actually does not have clear indications in CF.
Case presentation
The authors report the case of a boy affected by CF, Caucasian ethnicity, aged 13 years, sweat test: Cl− 103 mEq/l; Genotype: F508del/G542X; exocrine pancreatic insufficiency. The patient has been chronically colonised by methicillin resistant Staphylococcus aureus (MRSA) from the age of 7 years till 1 year ago, with repeated positivity of throat swab for Candida albicans. During the last 12 months throat swabs were always found to be positive for methicillin sensitive Staphylococcus aureus. Culture tests were always negative for Pseudomonas aeruginosa. Nutritional status was good, body mass index being 20.12 (60th centile, Standard Rolland-Cachera). During early childhood, the patient developed recurrent upper respiratory tract infections (URI), associated with asthma-like symptoms.
Investigations
Paper radioimmunosorbent test (PRIST) 437 kU/l with a positive prick test and radioallergosorbent test (RAST) for Dermatophagoides farinae, Dermatophagoides pteronyssinus, cat epithelium and birch, negative for Aspergillus spp. Forced expiratory volume in one second (FEV1)+16% pred. postinhalation of salbutamol 200 μg.
Differential diagnosis
Treatment
Since the age of 4 years, the patient started oral antihistaminic treatment (cetirizine 0.15 mg/kg once a day) and inhaled maintenance therapy with corticosteroid (budesonide 0.5 mg twice a day) and bronchodilator (salbutamol 2.5 mg twice a day).
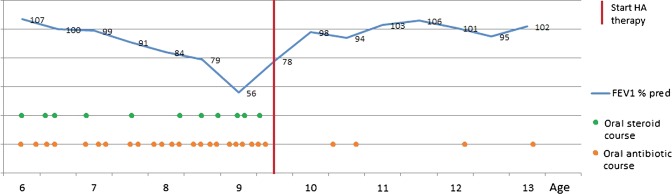
Given the recurrent URI, associated with wheezing, the patient required frequent courses of oral antibiotics, usually amoxicillin+clavulanic acid or trimethoprim+sulfamethoxazole and oral steroid therapy (betamethasone, 0.1–0.2 mg/kg) (figure 1).
Figure 1.
Hyaluronic acid improves ‘pleasantness’ and tolerability of nebulised hypertonic saline in a cohort of patients with cystic fibrosis.
From May to July 2008, the patient started on inhaled 7% NaCl therapy, preceded by salbutamol spray 200 μg; during the 3 months therapy, we did not observe any improvement in pulmonary function (stable FEV1 values) and exacerbations frequency, with a progressive intolerance to the treatment (onset of cough and bronchospasm).
In March 2009, we started the patient on aerosolised 7% NaCl+0.1% HA (Hyaneb—5 ml once a day, preceded by salbutamol spray 200 μg). This therapy is still going on and has been well-tolerated by first doses. Other maintenance therapies have not been modified.
Outcome and follow-up
We considered a 7-year follow-up:
During the first 42 months of observation the patient underwent 23 oral antibiotic courses (0.55 courses/month), of which 11 with concomitant oral steroid therapy (0.26 courses/month).
During last 42 months (after the start of HS+HA therapy), we observed a significant decrease of respiratory exacerbation and antibiotic therapy recurrence (four antibiotic courses; 0.10 courses/month), with no more use of oral steroids.
From the beginning of the treatment, we observed a gradual increase of FEV1 during the first few months (from 78% pred. to 103%), with a subsequent stabilisation to values around 100% of pred. Last FEV1 102% (figure 1). Last PRIST 271 kU/l. Probably as a result of the lower use of antibiotics, no more positivity for C. albicans or other fungi has been found. From starting of the HS+HA treatment, no other therapy or lifestyle changes took place and puberty has not yet occurred.
Discussion
Non-ABPA-related bronchial hyper-reactivity is a possible finding in people with CF; patients with ‘coexistent asthma’ could be defined by recurrent episodes of wheezing clinically responsive to bronchodilator therapy.9 These patients may undergo several antibiotic courses during childhood and this might lead to clinical and microbiological consequences. Actually there is no evidence in literature about treatment and clinical management of these patients.
HA is a biopolymer with several functions in human tissues, such as barrier effects, water homeostasis and mucociliary clearance. HA presents capacity to link and retain water molecules and to modify tissue morphogenesis,10 cells’ growth and hydratation, because of its influence on interstitial volume and membrane permeability. Aerosolised HA has been tested in patients with asthma against exercise-induced bronchoconstriction; in these few studies, results have not been unique and actually HA has a very limited use in asthma.
To date, in literature there are few works about HS+HA in CF and those are mainly focused on pleasantness. In our centre, we use HS+HA in patients who did not tolerate HS; in the described case, we observed, besides a good tolerance, also a dramatic decrease of antibiotic courses recurrence, with no more oral steroid course, and, after a good initial recovery (+25% FEV1), a stability of pulmonary function.
As reported in a recent large study, FEV1 decline in patient with CF persistently infected with MRSA is about −2.06% predicted/year,11 while in our patient during the last 3 years we observed little increase of FEV1 (about +1,33% predicted/year).
In conclusion, we think that this case suggests a possible indication for inhaled HA particularly symptomatic patients with CF with asthma-like symptoms and allergic sensitisations. Further studies will be critical to define HA indications and utility in CF.
Learning points.
Management of wheezing people with cystic fibrosis.
New therapeutic strategy in people with cystic fibrosis and asthma-like symptoms.
A possible defined indication for inhaled hyaluronic acid in cystic fibrosis
Footnotes
Contributors: F-C, A-N and F-F analysed the data and wrote the paper. R-C revised the paper. She is the guarantor.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Davies J, Rosenthal M, Bush A. Severe small airways disease resistant to medical treatment in a child with cystic fibrosis. J R Soc Med 1996;2013:172P–3P [PMC free article] [PubMed] [Google Scholar]
- 2.Welsh MJ, Smith AE. Molecular mechanisms of CFTR chloride channel dysfunction in cystic fibrosis. Cell 1993;2013:1251–4 [DOI] [PubMed] [Google Scholar]
- 3.Elkins MR, Bye PT. Inhaled hypertonic saline as a therapy for cystic fibrosis. Curr Opin Pulm Med 2006;2013:445–52 [DOI] [PubMed] [Google Scholar]
- 4.Turino GM, Cantor O. Hyaluronan in respiratory injury and repair. Am J Respir Crit Care Med 2003;2013:1169–75 [DOI] [PubMed] [Google Scholar]
- 5.Ratjen F. Inhaled hypertonic saline produces small increases in lung function in patients with cystic fibrosis. J Pediatr 2006;2013:142. [DOI] [PubMed] [Google Scholar]
- 6.Kunz LIZ, van Rensen ELJ, Sterk PJ. Inhaled hyaluronic acid against exercise-induced bronchoconstrinction in asthma. Pulm Pharmacol Ther 2006;2013:286–91 [DOI] [PubMed] [Google Scholar]
- 7.Scuri M, Abraham WM. Hyaluronan blocks human neutrophil elastase (HNE)-induced airway responses in sheep. Pulm Pharmacol Ther 2003;2013:335–40 [DOI] [PubMed] [Google Scholar]
- 8.Buonpensiero P, De Gregorio F, Sepe A, et al. Adv Ther 2010;2013:870–8 [DOI] [PubMed] [Google Scholar]
- 9.Van Asperen PP, Manglick P, Allen H. Mechanisms of bronchial hyperreactivity in cystic fibrosis. Pediatr Pulmonol 1988;2013:139–44 [DOI] [PubMed] [Google Scholar]
- 10.Laurent UBG, Reed RK. Turnover of hyaluronan in the tissues. Adv Drug Deliv Rev 1991;2013:237–56 [Google Scholar]
- 11.Sanders DB, Bittner RC, Rosenfeld M, et al. Failure to recover to baseline pulmonary function after cystic fibrosis pulmonary exacerbation. AM J Respir Crit Care Med 2010;2013:627–32 [DOI] [PMC free article] [PubMed] [Google Scholar]


