Abstract
Background
Reduced heart rate variability (HRV), a measure of cardiac autonomic dysfunction, is a risk factor for coronary artery disease. Diet can influence HRV but this association may be confounded by genetic and environmental factors.
Methods and Results
We administered the Willett Food Frequency Questionnaire to 276 middle-aged male twins. We derived a score measuring the extent to which an individual's diet conformed to the Mediterranean diet following a published algorithm. The higher the score, the greater the similarity to the Mediterranean diet. All twins underwent 24-hour ambulatory electrocardiogram recording. Time and frequency domain measures of HRV were calculated. Mixed-effects regression was used to partition the association into between- and within-twin pair differences. After adjusting for energy intake, other nutritional factors, shared genes and common environment, a one-unit higher score was significantly associated with 3.9%∼13% higher time and frequency domain HRV parameters. Further controlling for known cardiovascular risk factors and use of fish oil supplements and medications did not substantially change the estimates.
Conclusions
The Mediterranean dietary pattern is associated with higher HRV.
Keywords: diet, heart rate, cardiovascular diseases, epidemiology, twin
Introduction
The Mediterranean diet is associated with a reduction in cardiac death1-4 but the underlying mechanisms are poorly understood. Although individual healthy dietary components are associated with higher heart rate variability (HRV),5-9 a non-invasive measure of cardiac autonomic function,10-12 whether a whole dietary pattern resembling the Mediterranean diet is associated with higher HRV has not been addressed.
Autonomic dysfunction as measured by a lower HRV is an established risk factor for cardiac death.11, 13 In the general population, one standard deviation increment in frequency domains of HRV was associated with 24% -45% lower risk of coronary heart disease death.14 In patients with myocardial infarction, lower HRV was associated with at least twofold higher risk for all-cause death.15
Dietary habits are shared by individuals in the same family,16, 17 who may also share other genetically-determined cardiac risk factors. HRV has also been shown to be inherited to a certain degree.18 Thus, in this study, we examined whether conforming to the Mediterranean diet was associated with HRV in adult twins reared together, controlling for the potential confounding effects of family and genetic influences.
Subjects and Methods
Participants
The Twins Heart Study is an investigation of risk factors for subclinical cardiovascular disease; details have been published.18, 19 Briefly, this study included 180 pairs of monozygotic (MZ) and dizygotic (DZ) male twins asymptomatic of cardiovascular disease based on a 1990 survey from the Vietnam Era Twin Registry.18-21 All twin pairs were examined at the Emory University Hospital General Clinical Research Center between 2002 and 2006. The assessment included a comprehensive medical history, physical exam, biochemical measures, and ambulatory electrocardiogram recording (Holter); we also obtained updated information about symptomatic cardiovascular disease. We excluded 84 participants, including one man with no dietary data, six men reporting implausible energy intake (≥ 6000 or < 500 kcal/day),19, 20 eight men with plasma IL-6 levels above 10 pg/mL22 as this finding may imply acute inflammation that may affect HRV, and seventy-two men with HRV data not suitable for analysis (>20% interpolation or < 18 recorded hours).23 There was no participant with a history of atrial fibrillation or pacemaker. Some unpaired twins resulted from these exclusions; these were retained in the analyses in twin modeling because it allows full use of all available data.24 Therefore, our analyses were based on 276 men, including 65 MZ and 40 DZ twin pairs, and 33 MZ and 33 DZ unpaired twins. The study protocol was approved by the Institutional Review Board of Emory University and informed consent was obtained from all subjects.
Dietary Assessment and Mediterranean Diet Score
We used the Willett self-administered semi-quantitative food frequency questionnaire to collect dietary data over the previous 12 months.19, 20 Nutrient intake data were derived using the nutrient database of the US Department of Agriculture at the Channing Laboratory, Harvard University.19, 20 Portion sizes were converted into weight in grams, and daily food intake in grams was calculated by multiplying portion sizes in grams with food intake frequency. Combined food items containing two or more components were itemized based on the recipe.20
In observational epidemiological studies, the term Mediterranean diet is used to indicate a diet that contains elements of the originally defined Mediterranean diet.20 Thus, we ranked participants on the similarity of their diet to the originally described Mediterranean diet. We derived a score to measure the extent to which an individual's diet conformed to the Mediterranean diet following the Trichopoulou's algorithm, as previously described.19, 20 The score components were defined a priori3 (Supplemental Table). Seven desirable components incorporated into the score were: cereals, vegetables, fruits and nuts, legumes, fish, a high dietary ratio of monounsaturated to saturated fatty acids (as reflected by high olive oil consumption), and moderate alcohol consumption; two undesirable components were meat and dairy food products. The nine components were assumed to have equal weight. In order to conduct analyses stratified by zygosity, we used the zygosity-specific median of food intake (adjusted to 2500 kcal25) of the studied sample as the cutoff.3 A value of 1 was assigned to a high intake (≥ median) of each desirable component or a low intake (< median) of each undesirable food. All other intakes received a value of 0.3, 25 For alcohol, a value of 1 was assigned to moderate consumption, that is, an intake greater or equal to the median (1.91 gram/day, same for MZ and DZ twins) but below 33 gram per day; 19, 20 a value of 0 was assigned to either never or very-light drinking (≤1.91 gram/day) or excessive drinking (>33 gram/day). The score was the sum of all values from the nine components, ranging from 0 to 9; the higher the score, the more conforming to the Mediterranean diet.
Cardiac Autonomic Function Assessment
Detailed account of our HRV assessment in this sample has been previously described.18, 23 Briefly, participants wore an ambulatory electrocardiogram (SEER® Light ambulatory ECG recorder, three channel digital system, GE Healthcare) for 24 hours. Holter recordings were digitally sampled and analyzed for HRV in the time and frequency domains. Five time domain HRV measurements were included in the analysis: the standard deviation of all normal to normal (NN) R-R intervals (SDNN), the standard deviation of 5-minute average NN intervals (SDANN), the mean of the standard deviations of all NN intervals for all 5-minute segments of the entire recording (SDNNI), the square root of the mean of squares of successive NN interval differences (rMSSD), and the percentage of intervals above 50 ms different from preceding interval (pNN50). Additionally, six frequency domain HRV parameters were analyzed using power spectral analysis:13, 18, 23 total power (TotPow, < 0.40 ms2), ultra-low frequency (ULF, 0 ∼ 0.0033 ms2), very-low frequency (VLF, 0.0033 to < 0.04 ms2), low frequency (LF, 0.04 to < 0.15 ms2) and high frequency power (HF, 0.15 to < 0.40 ms2).
Known Cardiovascular Disease Risk Factors
Systolic and diastolic blood pressure, fasting plasma concentrations of glucose, triacylglycerols, and total, low- and high-density lipoprotein cholesterol were measured using the standard methods as previously described.19, 20 Hypertension was defined as systolic blood pressure ≥140 and/or diastolic blood pressure ≥90 mmHg, or current use of antihypertensive medicines. Diabetes was defined as a fasting plasma glucose concentration ≥6.99 mmol/L (126 mg/dL)26 or current treatment with insulin or oral antihyperglycemic agents. Smoking (never, former, and current smoking status), education, and marital status were collected using standardized questionnaires. Habitual physical activity was evaluated with the validated Baecke questionnaire.27 Waist and hip circumferences were measured to calculate the waist-to-hip ratio. Depressive symptoms were measured with the Beck Depression Inventory (BDI), which yielded a continuous score.28 Current use of β-blockers, aspirin, statins, antihypertensives, and antihyperglycemics was also recorded. Information on standard cardiovascular risk factors was used to derive a Framingham risk score.29
Statistical Analysis
The association between the Mediterranean diet and HRV was assessed by fitting linear regression models and examined at two levels:19, 20, 24 between-subject and within-pair. All HRV data were log-transformed to improve normality, and thus results were expressed as percent differences of the non-transformed values using the formula: [(expβ)−1] × 100 (%), where β is the regression coefficient and expβ returns the exponential value of the parameter.
We evaluated the overall association by treating twins as individuals while accounting for twin pair clustering by zygosity.19, 20 The score was analyzed primarily as a continuous variable and secondarily as an ordinal variable according to quartiles (0 to 3, 4, 5, and 6 to 9) with category midpoints as ordinal values.
We then performed within-pair analyses to examine differences in HRV measures between co-twins in each pair;24 by design, these analyses are free of familial confounding. 19, 20 We fitted mixed models for twins,19, 20, 24 including within-pair difference in Mediterranean diet score and covariates as fixed effects; and the twin pair as a random effect.19, 20 The percent difference calculated from the β coefficient for the within-pair effect represents the percent difference in outcome (HRV) per one-unit absolute difference in the score between co-twins. An analysis excluding unpaired twins provided similar within-pair results. This is expected since unpaired twins are naturally not considered in within-pair analyses and only contribute to between-pair effects reflecting shared factors between co-twins.24
We fit an initial model that include Mediterranean diet score and adjusted for nutritional factors not considered in the score, including total energy intake, potato and egg consumption.3 We further adjusted for sociodemographic factors (years of education and current marital status); lifestyle factors (waist-to-hip ratio and physical activity); cardiovascular risk factors (Framingham risk score29 and fasting plasma concentrations of triacylglycerols); use of fish oil supplement, β-blockers, and other medications (aspirin, statins, antihypertensives, and antihyperglycemics).
MZ twins share 100% of identical genes; DZ twins share on average 50%. Common environmental effects are assumed to contribute equally to the similarity in MZ and DZ twins. Therefore, the zygosity-specific associations were examined and interpreted as follows: if the association between Mediterranean diet score and HRV was similar in both DZ and MZ pairs, this would suggest the association is not due to confounding by either shared environmental factors or genetics; if the association was found in DZ pairs but not in MZ pairs, this would be an indication that genetic factors are potentially confounding the association between Mediterranean diet and HRV. More formally we included an interaction term in our models between Mediterranean diet score and zygosity; the significance of this parameter estimate was a direct test of the differential association between the score and HRV by zygosity. The heritability for conforming to the Mediterranean diet was calculated as the twice difference in the previously reported intraclass correlation coefficient19 between MZ and DZ twins. All analyses were conducted using SAS software version 9.1 (SAS Institute, Cary, NC). Significance levels were set at 0.05, two-sided.
Results
Participant Characteristics
Demographic and clinical characteristics of the sample are described in Table 1. The sample was 94% Non-Hispanic White, 3% African-American, and 3% other race/ethnic groups. This distribution reflected the racial distribution of the Vietnam Era Twin Registry. A higher Mediterranean diet score was associated with more years of education, less frequent smoking, lower depressive symptom score, and higher use of fish oil supplements.
Table 1. Sample characteristics according to the Mediterranean diet score.
| Variable | Mediterranean Diet Score | Trend P value* | |||
|---|---|---|---|---|---|
|
| |||||
| 0-3 (n = 78) | 4 (n = 58) | 5 (n = 65) | 6-9 (n = 75) | ||
| Age, y | 54 (51,56) | 55 (53,57) | 55 (52,56) | 55 (53,57) | 0.71 |
| Education, y | 13 (12,15) | 14 (13,16) | 15 (12,16) | 15 (13,16) | <0.0001 |
| Married, n (%) | 62 (80) | 45 (76) | 51 (78) | 64 (85) | 0.56 |
| Smoking | 0.008 | ||||
| Current smoker, n (%) | 20 (26) | 10 (17) | 9 (14) | 9 (12) | |
| Former smoker, n (%) | 36 (46) | 25 (43) | 27 (42) | 34 (45) | |
| Never, n (%) | 22 (28) | 23 (40) | 29 (45) | 32 (43) | |
| Body mass index, kg/m2 | 30.0 (26.3, 32.6) | 29.6 (26.3, 33.6) | 28.6 (26.6, 32.1) | 28.0 (26.6, 29.6) | 0.17 |
| Waist to hip ratio | 0.95 (0.92, 0.98) | 0.96 (0.92, 0.99) | 0.93 (0.90, 0.99) | 0.93 (0.90, 0.97) | 0.41 |
| Physical activity, unit | 7.20 (6.11, 8.20) | 7.27 (6.59, 8.63) | 7.40 (6.88, 8.30) | 7.52 (6.50, 8.21) | 0.24 |
| Total caloric intake, kcal | 1552 (1256, 2059) | 1453 (1056, 1793) | 1417 (1048, 1803) | 1369 (1082, 1641) | 0.07 |
| Clinical and biochemical features | |||||
| Depressive symptoms (BDI score), unit | 4 (1,9) | 2 (1,6) | 2 (0,6) | 2 (0,6) | 0.02 |
| Plasma glucose concentration, mmol/L | 5.44 (5.11, 5.83) | 5.49 (5.11, 6.16) | 5.38 (5.00, 5.66) | 5.44 (5.11, 5.83) | 0.35 |
| Systolic blood pressure, mm Hg | 132 (120, 142) | 125 (116, 138) | 126 (117, 138) | 128 (122, 139) | 0.88 |
| Diastolic blood pressure, mm Hg | 81 (73, 87) | 80 (73, 85) | 78 (70, 88) | 82 (77, 89) | 0.04 |
| Total triacylglycerols concentration, mmol/L | 1.98 (1.40, 2.79) | 1.60 (1.16, 2.26) | 1.74 (1.22, 2.44) | 1.84 (1.18, 2.60) | 0.92 |
| Total Cholesterol concentration, mmol/L | 4.79 (4.22, 5.44) | 4.71 (4.14, 5.44) | 4.71 (4.25, 5.54) | 4.97 (4.22, 5.39) | 0.47 |
| HDL-Cholesterol concentration, mmol/L | 0.96 (0.80, 1.14) | 1.01 (0.80, 1.24) | 1.01 (0.91, 1.17) | 0.91 (0.83, 1.09) | 0.83 |
| LDL-Cholesterol concentration, mmol/L | 3.24 (2.64, 3.76) | 3.13 (2.59, 3.57) | 3.13 (2.51, 3.76) | 3.16 (2.77, 3.86) | 0.55 |
| Take fish oil supplement, n (%) | 1 (1.3) | 1 (1.7) | 5 (7.7) | 8 (11.7) | 0.02 |
| Take β-blockers, n (%) | 7 (9) | 5 (9) | 2 (3) | 5 (7) | 0.46 |
| Take statins, n (%) | 21 (27) | 12 (21) | 16 (25) | 19 (25) | 0.83 |
| Take aspirin, n (%) | 14 (18) | 14 (24) | 16 (25) | 17 (23) | 0.51 |
| Take antihypertensives, n (%) | 16 (21) | 13 (22) | 14 (22) | 16 (21) | 0.96 |
| Take antihyperglycemics, n (%) | 5 (6.4) | 8 (13.8) | 6 (9.2) | 6 (8.0) | 0.83 |
Medians (25th, 75th percentile) for continuous variables and n (%) for categorical variables.
Test for trend across diet score groups. All P values are corrected for clustering within a twin pair according to the twin type using linear mixed models for continuous variables, and generalized estimating equation logistic models for dichotomous variables, and repeated proportional odds model with generalized estimating equation for the 3-level smoking variable. Medians presented are raw values.
Overall Associations between the Mediterranean Diet and HRV
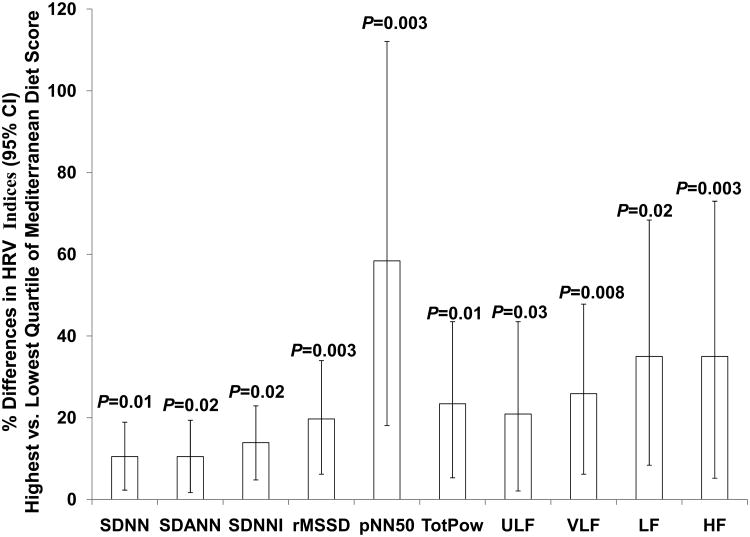
A higher score was positively associated with higher HRV including SDNN, SDNNI, rMSSD, pNN50, TotPow, ULF, VLF, and LF, respectively (all P<0.05) (Model 1, Table 2). Further adjustment for other variables did not change the magnitude of association for the time domain parameters but minimally altered the magnitude for the frequency domain measures (Model 2, Table 2). By using Mediterranean diet score as an ordinal variable, similar trends were found (Table 2). Figure 1 shows that HRV variables were 10% ∼ 58% higher in men in the highest score quartile than those in the lowest quartile (P<0.05 for all HRV indices).
Table 2. Associations Between the Mediterranean Diet Score and Heart Rate Variability in the Entire Sample.
| Outcome | Difference (%) (95% CI)per 1-unit increment in score*(n = 276) | P value | Means (95% CI) of Log-Transformed HRV Measures | P value§ | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| Diet Score = 0-3 (n =78) | Diet Score = 4 (n =58) | Diet Score = 5 (n =65) | Diet Score = 6-9 (n =75) | |||||||||||
| Time-domain | ||||||||||||||
| Model 1: Zygosity and nutritional factors not in the score adjusted† | ||||||||||||||
| SDNN, ms | 1.8 (0.2, 3.4) | 0.03 | 4.77 (4.71, 4.82) | 4.88 (4.81, 4.94) | 4.85 (4.79, 4.91) | 4.87 (4.81, 4.93) | 0.02 | |||||||
| SDANN, ms | 1.6 (−0.1, 3.3) | 0.07 | 4.60 (4.54, 4.66) | 4.69 (4.63, 4.76) | 4.66 (4.60, 4.73) | 4.69 (4.63, 4.75) | 0.04 | |||||||
| SDNNI, ms | 2.9 (1.2, 4.8) | 0.001 | 3.98 (3.91, 4.04) | 4.10 (4.03, 4.17) | 4.13 (4.06, 4.19) | 4.13 (4.06, 4.19) | 0.003 | |||||||
| rMSSD, ms | 3.9 (1.3, 6.5) | 0.003 | 3.37 (3.28, 3.45) | 3.58 (3.48, 3.67) | 3.55 (3.46, 3.64) | 3.55 (3.46, 3.64) | 0.005 | |||||||
| pNN50, % | 10.5 (3.6, 18) | 0.003 | 1.49 (1.27, 1.72) | 1.90 (1.66, 2.15) | 1.87 (1.63, 2.11) | 1.96 (1.74, 2.18) | 0.005 | |||||||
| Model 2: Multivariate adjusted‡ | ||||||||||||||
| SDNN, ms | 1.7 (0.1, 3.4) | 0.04 | 4.73 (4.63, 4.84) | 4.84 (4.74, 4.95) | 4.80 (4.70, 4.90) | 4.83 (4.73, 4.93) | 0.02 | |||||||
| SDANN, ms | 1.6 (−0.1, 3.4) | 0.07 | 4.55 (4.44, 4.67) | 4.65 (4.54, 4.77) | 4.61 (4.50, 4.72) | 4.65 (4.54, 4.75) | 0.03 | |||||||
| SDNNI, ms | 2.7 (1, 4.5) | 0.003 | 3.98 (3.87, 4.09) | 4.10 (3.99, 4.21) | 4.08 (3.98, 4.19) | 4.11 (4.01, 4.22) | 0.006 | |||||||
| rMSSD, ms | 3.8 (1.1, 6.4) | 0.005 | 3.42 (3.26, 3.58) | 3.60 (3.43, 3.76) | 3.57 (3.42, 3.73) | 3.59 (3.44, 3.75) | 0.007 | |||||||
| pNN50, % | 10.1 (3.2, 17.4) | 0.004 | 1.73 (1.32, 2.14) | 2.08 (1.66, 2.50) | 2.01 (1.61, 2.41) | 2.18 (1.78, 2.57) | 0.007 | |||||||
| Frequency-domain | ||||||||||||||
| Model 1: Zygosity and nutritional factors not in the score adjusted† | ||||||||||||||
| TotPow, ms2 | 4.5 (1.1, 7.9) | 0.009 | 9.29 (9.17, 9.41) | 9.54 (9.41, 9.67) | 9.51 (9.39, 9.63) | 9.53 (9.42, 9.65) | 0.003 | |||||||
| ULF, ms2 | 4.1 (0.4, 7.9) | 0.03 | 9.00 (8.87, 9.12) | 9.24 (9.10, 9.38) | 9.18 (9.05, 9.31) | 9.23 (9.10, 9.35) | 0.01 | |||||||
| VLF, ms2 | 5.5 (1.8, 9.5) | 0.004 | 7.41 (7.28, 7.54) | 7.65 (7.51, 7.79) | 7.72 (7.58, 7.85) | 7.67 (7.54, 7.80) | 0.01 | |||||||
| LF, ms2 | 7.9 (2.8, 13.3) | 0.002 | 6.40 (6.23, 6.57) | 6.65 (6.47, 6.84) | 6.80 (6.62, 6.98) | 6.74 (6.57, 6.91) | 0.02 | |||||||
| HF, ms2 | 4.5 (−1.2, 10.6) | 0.12 | 5.12 (4.93, 5.31) | 5.60 (5.39, 5.81) | 5.43 (5.23, 5.63) | 5.40 (5.21, 5.59) | 0.10 | |||||||
| Model 2: Multivariate adjusted‡ | ||||||||||||||
| TotPow, ms2 | 3.6 (0.2, 7.1) | 0.04 | 9.26 (9.05, 9.48) | 9.50 (9.29, 9.72) | 9.42 (9.22, 9.63) | 9.47 (9.27, 9.67) | 0.007 | |||||||
| ULF, ms2 | 3.0 (−0.6, 7.0) | 0.10 | 8.98 (8.74, 9.21) | 9.21 (8.97, 9.45) | 9.11 (8.88, 9.33) | 9.17 (8.95, 9.39) | 0.02 | |||||||
| VLF, ms2 | 4.8 (1.0, 8.7) | 0.012 | 7.45 (7.22, 7.68) | 7.69 (7.46, 7.93) | 7.68 (7.46, 7.90) | 7.68 (7.47, 7.90) | 0.02 | |||||||
| LF, ms2 | 7.7 (2.6, 13.1) | 0.003 | 6.35 (6.04, 6.66) | 6.56 (6.25, 6.87) | 6.66 (6.36, 6.95) | 6.66 (6.37, 6.95) | 0.01 | |||||||
| HF, ms2 | 4.7 (−1.0, 10.8) | 0.11 | 5.12 (4.77, 5.47) | 5.59 (5.23, 5.95) | 5.40 (5.07, 5.74) | 5.43 (5.11, 5.76) | 0.07 | |||||||
Values are % differences in geometric means (95% CI) calculated from the β coefficient of the diet score.
Total energy intake (continuous), egg consumption (continuous), potato consumption (continuous).
Demographic factors [education (continuous) and marital status (yes/no)]; lifestyle factors [physical activity (continuous), waist-to-hip ratio (continuous)]; coronary risk factors [Framingham risk score (continuous) and plasma triglycerides (continuous)]; use of fish oil supplements (yes/no), β-blockers (yes/no), and other medications (statins, aspirin antihypertensives, and antihyperglycemics) (yes/no).
Test for trend across diet groups.
Figure 1.
Overall associations based on the Mediterranean diet score quartiles after controlling for zygosity, nutritional, demographic, lifestyle, coronary risk factors, and use of fish oil supplement, β-blockers, and other medications.
The intraclass correlation coefficient of Mediterranean diet score was 0.26 for MZ and 0 for DZ as previously reported;19 thus, heritability was calculated as 52% for following the Mediterranean dietary pattern, suggesting genetic influences on this phenotype. Therefore, we conducted within-pair analyses that controlled for potential genetic confounding in the association between the diet and HRV. Within-pair analyses also controlled for environmental factors shared between co-twins.
Within-Pair Association between the Mediterranean Diet and HRV
Within-pair association between the score and HRV tended to be more pronounced in the DZ than in the MZ twin pairs. However, the interaction with zygosity was significant only for LF (P=0.047), implying possible genetic confounding for LF (Model 2, Table 3). In the pooled sample by zygosity for the other HRV parameters, a higher Mediterranean diet score was associated with a higher SDNNI, rMSSD, pNN50, TotPow, VLF, and HF, respectively, after controlling for shared genes and common environment (all P<0.05) (Model 1, Table 3). Full adjustment did not substantially change the results but the association for TotPow and HF became marginally statistically significant (0.05<P<0.1) (Model 2, Table 3).
Table 3. Within-Pair Percent Difference in Heart Rate Variability per 1-Unit Within-pair Difference in the Mediterranean Diet Score, Overall and by Zygosity*.
| MZ+DZ | MZ | DZ | Interaction withZygosity P value | ||||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| Within-pair Difference (%) (95% CI) | P value | Within-pair Difference (%) (95% CI) | P value | Within-pair Difference (%) (95% CI) | P value | ||
| Time domain | |||||||
| Model 1: Zygosity and nutritional factors not in the score adjusted† | |||||||
| SDNN, ms | 2.2 (0.2, 4.2) | 0.03 | 1.7 (−0.7, 4.2) | 0.16 | 2.8 (−1.0, 6.9) | 0.15 | 0.63 |
| SDANN, ms | 2.0 (−0.2, 4.2) | 0.07 | 1.7 (−1.0, 4.4) | 0.21 | 1.8 (−2.4, 6.1) | 0.40 | 0.93 |
| SDNNI, ms | 3.9 (1.7, 6.0) | 0.001 | 2.8 (0.3, 5.3) | 0.03 | 7.6 (3.3, 12.0) | 0.001 | 0.09 |
| rMSSD, ms | 4.2 (1.0, 7.5) | 0.01 | 2.8 (−1.1, 7.0) | 0.15 | 5.4 (−0.2, 11.3) | 0.06 | 0.43 |
| pNN50, % | 12.9 (4.0, 22.5) | 0.004 | 7.1 (−3.4, 19.0) | 0.19 | 22.0 (6.5, 39.9) | 0.005 | 0.13 |
| Model 2: Multivariate adjusted‡ | |||||||
| SDNN, ms | 1.9 (−0.1, 3.9) | 0.07 | 1.3 (−1.1, 3.7) | 0.28 | 1.2 (−2.4, 4.9) | 0.51 | 0.80 |
| SDANN, ms | 1.8 (−0.4, 4.0) | 0.11 | 1.3 (−1.3, 3.9) | 0.33 | 0.5 (−3.2, 4.4) | 0.79 | 0.95 |
| SDNNI, ms | 3.5 (1.3, 5.6) | 0.002 | 2.3 (−0.3, 4.9) | 0.08 | 5.2 (1.4, 9.2) | 0.009 | 0.17 |
| rMSSD, ms | 3.5 (0.2, 6.8) | 0.04 | 1.9 (−2.0, 5.9) | 0.34 | 1.8 (−4.2, 8.3) | 0.54 | 0.47 |
| pNN50, % | 11.1 (2.4, 20.4) | 0.01 | 4.8 (−5.4, 16.3) | 0.36 | 11.9 (−2.6, 28.4) | 0.11 | 0.20 |
| Frequency domain | |||||||
| Model 1: Zygosity and nutritional factors not in the score adjusted† | |||||||
| TotPow, ms2 | 4.9 (0.9, 9.2) | 0.02 | 4.1 (−0.3, 9.2) | 0.07 | 6.2 (−2.6, 15.1) | 0.17 | 0.80 |
| ULF, ms2 | 4.0 (−0.5, 8.7) | 0.08 | 3.0(-2.1, 8.8) | 0.24 | 4.1 (−5.0, 14.0) | 0.38 | 0.88 |
| VLF, ms2 | 7.1 (2.4, 12.0) | 0.003 | 6.2 (0.2, 11.4) | 0.04 | 12.7 (4.3, 22.6) | 0.004 | 0.26 |
| LF, ms2 | 13.0 (6.3, 20.0) | <0.0001 | 9.4 (1.2, 17.2) | 0.023 | 25.9 (12.7, 39.1) | <0.0001 | 0.052 |
| HF, ms2 | 7.4 (0.1, 15.1) | 0.047 | 3.0 (−5.7, 13.2) | 0.48 | 12.7 (0.4, 26.2) | 0.042 | 0.25 |
| Model 2: Multivariate adjusted‡ | |||||||
| TotPow, ms2 | 3.6 (−0.6, 7.8) | 0.095 | 2.0 (−2.4, 7.6) | 0.31 | 2.0 (−5.4, 10.8) | 0.53 | 0.95 |
| ULF, ms2 | 2.2 (−2.4, 7.1) | 0.34 | 1.0 (−4.4, 6.9) | 0.70 | 1.0 (−7.7, 9.7) | 0.88 | 0.91 |
| VLF, ms2 | 6.1 (1.5, 11.0) | 0.011 | 4.1 (−1.4, 10.0) | 0.14 | 9.4 (1.6, 17.8) | 0.02 | 0.36 |
| LF, ms2 | 13.1 (6.4, 20.3) | <0.0001 | 7.3 (−0.8, 16.2) | 0.08 | 19.7 (9.7, 31.3) | <0.0001 | 0.047 |
| HF, ms2 | 6.3 (−0.9, 14.0) | 0.09 | 2.0 (−7.0, 11.0) | 0.73 | 6.2 (−4.6, 19.2) | 0.24 | 0.25 |
Values are within-pair % geometric mean differences (95% CI) calculated from the β coefficient and expressed per 1-unit difference in the Mediterranean diet score comparing the twin with a higher score to his brother with a lower score.
Total energy intake (continuous), egg consumption (continuous), potato consumption (continuous).
Demographic factors [education (continuous) and marital status (yes/no)]; lifestyle factors [physical activity (continuous)] and waist-to-hip ratio (continuous)]; coronary risk factors [Framingham risk score (continuous) and plasma triglycerides (continuous)]; use of fish oil supplements (yes/no), β-blockers (yes/no), and other medications (statins, aspirin, antihypertensives, and antihyperglycemics) (yes/no).
After further controlling for inflammatory biomarkers (interleukin-6 and high sensitive C-reactive protein), the within-pair association between the score and HF became statistically significant [8.3% (95% CI: 1.0∼16.2%), P=0.03], while for other HRV measures it did not meaningfully change (data not shown). Similar results were also obtained after further controlling for depressive symptom score, after substituting the Framingham risk score for individual risk factors, and after excluding subjects with previous history of coronary heart disease (data not shown).
Discussion
We found a significantly positive association between a pattern of diet conforming to the Mediterranean diet and both time and frequency domain measures of HRV. After full adjustment, a one-unit higher Mediterranean diet score was associated with a 3.5% higher SDNNI, 3.5% higher rMSSD, 11.1% higher pNN50; and 6.1% higher VLF, independent of shared genes and common environment. We observed larger differences within DZ than MZ twin pairs in several HRV measures, implying a shared genetic pathway between the diet and HRV. However, because a significant interaction by zygosity was only found for LF, our results suggest that a shared genetic pathway does not entirely explain the association between Mediterranean diet and HRV.
This study is the first to demonstrate an association between the Mediterranean diet and HRV. Prior epidemiological investigations5-7, 9, 30 and randomized trials8 have documented an association between individual dietary components and HRV. For instance, green leafy vegetables;5 fish;6 marine6-8 and plant9 omega-3 fatty acids; and methyl-related nutrients30 are positively associated with HRV indices, including SDNN,7, 9, 30 SDNNI,7 rMSSD,7 pNN50,7 and HF.6-8 One study showed that fish and marine omega-3 fatty acids were inversely associated with 24-hour LF.6 In another study, postmenopausal women practicing a long-term ovo-lacto vegetarian diet had higher HF and increased baroreflex sensitivity compared to omnivore controls.31 Our results were generally in agreement with these previous reports, and for the first time demonstrate a link between Mediterranean diet and HRV.
Our study results have potential clinical significance. Prior studies have shown that reduced HRV is associated with poor outcomes in the general population14 and individuals with coronary artery disease.13 In our study, the highest quartile of the Mediterranean diet score compared with the lowest quartile was associated with 11% to 58% higher HRV in both frequency and time domains. Based on mortality studies, these differences would translate into 9% -14% reduction in cardiac mortality.14 In our study, the strongest associations were found for pNN50, considered by some a marker for parasympathetic activity; and for VLF and LF, which reflect overall balance of the sympathetic and parasympathetic limbs.11, 12
The mechanisms linking the Mediterranean diet to HRV are unknown. The dietary components characteristic of the Mediterranean diet, including food items,5, 6 nutrients,32 and diet-related biochemical reactions involving energy generation and nutrient metabolism,32 may all potentially affect HRV through modulating sympathetic and parasympathetic activity and central thermoregulatory control.
Genetic factors may influence food preference,33 perception of hunger,34 and food consumption frequency,35 and thus may impact consumption of specific foods that comprise a Mediterranean diet. Heritability was 20% ∼95% for HRV frequency domain measures in this study population,18 suggesting genetic influences on HRV. An interesting finding of our study is that genetic factors appear to play a role in the modulation LF by the Mediterranean diet. The Framingham Heart Study reported that chromosome 2 at 153 cM was related to LF.36 Our results warrant future research on how this or other genetic variations affect the influence of the Mediterranean diet on LF.
There are some limitations to our study.19, 20 Our sample only included middle-aged men predominantly white men, and therefore our results may not be generalizable to women and other ethnic groups. As our study is cross-sectional, cause and effect relations cannot be established. Furthermore, the Willett food-frequency questionnaire may underestimate absolute food and nutrient intakes. However, this questionnaire is appropriate for the investigation of the association between habitual diet and health after energy adjustment, and has been extensively used in epidemiological research.37 Finally, physical activity can affect HRV and therefore may confound the results; however, we adjusted for habitual physical activity in the analysis and controlled for physical activity during Holter recording by design.18, 23
In comparison with traditional observational epidemiological studies, our study had the advantage of controlling for potential genetic and environmental confounding, including, for example, familial factors such as parents' socioeconomic status, family health habits other than diet, and maternal/prenatal factors.
In conclusion, our study demonstrates for the first time a positive association between the Mediterranean dietary pattern and HRV. Our findings suggest that autonomic tone may be one of mechanisms linking the Mediterranean diet to a lower rate of cardiovascular events.
Supplementary Material
What is Known
The Mediterranean diet is associated with lower cardiovascular risk.
Lower heart rate variability, reflecting cardiac autonomic dysfunction, is a risk factor for cardiac death.
To date, no prior studies have explored the association between a whole diet conforming to the Mediterranean diet and cardiac autonomic function measured as heart rate variability.
What This Article Adds
Using a twin study design, for the first time, we found that the more an individual's diet conformed to the Mediterranean diet, the greater the heart rate variability, indicating better cardiac autonomic function.
This positive association was independent of genes, shared environmental factors, and known cardiovascular risk factors; this means that, whether or not a person has an adverse genetic background or other risk factors for cardiovascular disease, this person would be likely to have better cardiac autonomic function if he or she follows a diet similar to the Mediterranean diet.
Acknowledgments
We gratefully acknowledge the continued cooperation and participation of the members of the Vietnam Era Twin Registry. Without their contribution, this research would not have been possible.
Funding/Support: This work was supported by NIH (R01 HL68630, R01 AG026255, and K24 HL077506 to Dr. Vaccarino; and K24 RR023356 to Dr. Ziegler); the American Heart Association (0245115N to Dr. Vaccarino), the Emory University Hospital General Clinical Research Center (M01-RR00039), and the Intramural Funding of Indiana University Department of Applied Health Science (to Dr. Dai). The United States Department of Veterans Affairs has provided financial support for the development and maintenance of the Vietnam Era Twin Registry. Numerous organizations have provided invaluable assistance, including: Veterans Affairs Cooperative Studies Program; Department of Defense; National Personnel Records Center, National Archives and Records Administration; the Internal Revenue Service; NIH; National Opinion Research Center; National Research Council, National Academy of Sciences; the Institute for Survey Research, Temple University.
Footnotes
Conflict of Interest Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr Jun Dai, Dept of Applied Health Science, School of Health, Physical Education and Recreation, Indiana Univ, Bloomington, IN; Indiana Ctr for Vascular Biology and Med, Indianapolis, IN.
Dr Rachel Lampert, Section of Cardiovascular Med, Yale Univ School of Med.
Dr Peter W. Wilson, Dept of Med, Division of Cardiology, Yale, CT; Emory Program in Cardiovascular Outcomes Research and Epidemiology (EPICORE), Emory Univ School of Med, Atlanta, GA; Dept of Epidemiology, Rollins School of Public Health, Emory Univ, Atlanta, GA; Ctr of Epidemiology and Genomic Med, Atlanta VA Medical Ctr, Atlanta, GA.
Dr Jack Goldberg, Vietnam Era Twin Registry, Seattle VA Epidemiologic Research and Information Ctr and the Dept of Epidemiology, School of Public Health, Univ of Washington, Seattle, WA.
Dr Thomas R. Ziegler, Dept of Med, Division of Endocrinology, Metabolism and Lipids, Emory Univ School of Med, Atlanta, GA; Nutrition and Health Sciences Graduate Program, Emory Univ, Atlanta, GA.
Dr Viola Vaccarino, Dept of Med, Division of Cardiology, Yale, CT; Emory Program in Cardiovascular Outcomes Research and Epidemiology (EPICORE), Emory Univ School of Med, Atlanta, GA; Dept of Epidemiology, Rollins School of Public Health, Emory Univ, Atlanta, GA; Nutrition and Health Sciences Graduate Program, Emory Univ, Atlanta, GA.
References
- 1.Mitrou PN, Kipnis V, Thiebaut AC, Reedy J, Subar AF, Wirfalt E, Flood A, Mouw T, Hollenbeck AR, Leitzmann MF, Schatzkin A. Mediterranean Dietary Pattern and Prediction of All-Cause Mortality in a US Population: Results From the NIH-AARP Diet and Health Study. Arch Intern Med. 2007;167:2461–2468. doi: 10.1001/archinte.167.22.2461. [DOI] [PubMed] [Google Scholar]
- 2.Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009;119:1093–1100. doi: 10.1161/CIRCULATIONAHA.108.816736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348:2599–2608. doi: 10.1056/NEJMoa025039. [DOI] [PubMed] [Google Scholar]
- 4.Dalziel K, Segal L, de Lorgeril M. A mediterranean diet is cost-effective in patients with previous myocardial infarction. J Nutr. 2006;136:1879–1885. doi: 10.1093/jn/136.7.1879. [DOI] [PubMed] [Google Scholar]
- 5.Park SK, Tucker KL, O'Neill MS, Sparrow D, Vokonas PS, Hu H, Schwartz J. Fruit, vegetable, and fish consumption and heart rate variability: the Veterans Administration Normative Aging Study. Am J Clin Nutr. 2009;89:778–786. doi: 10.3945/ajcn.2008.26849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mozaffarian D, Stein PK, Prineas RJ, Siscovick DS. Dietary Fish and ω-3 Fatty Acid Consumption and Heart Rate Variability in US Adults. Circulation. 2008;117:1130–1137. doi: 10.1161/CIRCULATIONAHA.107.732826. [DOI] [PubMed] [Google Scholar]
- 7.Christensen JH, Skou HA, Fog L, Hansen V, Vesterlund T, Dyerberg J, Toft E, Schmidt EB. Marine n-3 fatty acids, wine intake, and heart rate variability in patients referred for coronary angiography. Circulation. 2001;103:651–657. doi: 10.1161/01.cir.103.5.651. [DOI] [PubMed] [Google Scholar]
- 8.Ninio DM, Hill AM, Howe PR, Buckley JD, Saint DA. Docosahexaenoic acid-rich fish oil improves heart rate variability and heart rate responses to exercise in overweight adults. Br J Nutr. 2008;100:1097–1103. doi: 10.1017/S0007114508959225. [DOI] [PubMed] [Google Scholar]
- 9.Christensen JH, Schmidt EB, Molenberg D, Toft E. Alpha-linolenic acid and heart rate variability in women examined for coronary artery disease. Nutr Metab Cardiovasc Dis. 2005;15:345–351. doi: 10.1016/j.numecd.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Akselrod S, Gordon D, Ubel FA, Shannon DC, Berger AC, Cohen RJ. Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-beat cardiovascular control. Science. 1981;213:220–222. doi: 10.1126/science.6166045. [DOI] [PubMed] [Google Scholar]
- 11.Lahiri MK, Kannankeril PJ, Goldberger JJ. Assessment of autonomic function in cardiovascular disease: physiological basis and prognostic implications. J Am Coll Cardiol. 2008;51:1725–1733. doi: 10.1016/j.jacc.2008.01.038. [DOI] [PubMed] [Google Scholar]
- 12.Taylor JA, Carr DL, Myers CW, Eckberg DL. Mechanisms underlying very-low-frequency RR-interval oscillations in humans. Circulation. 1998;98:547–555. doi: 10.1161/01.cir.98.6.547. [DOI] [PubMed] [Google Scholar]
- 13.Bigger JT, Jr, Fleiss JL, Steinman RC, Rolnitzky LM, Kleiger RE, Rottman JN. Frequency domain measures of heart period variability and mortality after myocardial infarction. Circulation. 1992;85:164–171. doi: 10.1161/01.cir.85.1.164. [DOI] [PubMed] [Google Scholar]
- 14.Tsuji H, Larson MG, Venditti FJ, Jr, Manders ES, Evans JC, Feldman CL, Levy D. Impact of reduced heart rate variability on risk for cardiac events. The Framingham Heart Study. Circulation. 1996;94:2850–2855. doi: 10.1161/01.cir.94.11.2850. [DOI] [PubMed] [Google Scholar]
- 15.Bigger JT, Jr, Fleiss JL, Rolnitzky LM, Steinman RC. Frequency domain measures of heart period variability to assess risk late after myocardial infarction. J Am Coll Cardiol. 1993;21:729–736. doi: 10.1016/0735-1097(93)90106-b. [DOI] [PubMed] [Google Scholar]
- 16.Rankinen T, Bouchard C. Genetics of food intake and eating behavior phenotypes in humans. Annu Rev Nutr. 2006;26:413–434. doi: 10.1146/annurev.nutr.26.061505.111218. [DOI] [PubMed] [Google Scholar]
- 17.Maynard M, Gunnell D, Ness AR, Abraham L, Bates CJ, Blane D. What influences diet in early old age? Prospective and cross-sectional analyses of the Boyd Orr cohort. Eur J Public Health. 2006;16:316–324. doi: 10.1093/eurpub/cki167. [DOI] [PubMed] [Google Scholar]
- 18.Vaccarino V, Lampert R, Bremner JD, Lee F, Su S, Maisano C, Murrah NV, Jones L, Jawed F, Afzal N, Ashraf A, Goldberg J. Depressive symptoms and heart rate variability: evidence for a shared genetic substrate in a study of twins. Psychosom Med. 2008;70:628–636. doi: 10.1097/PSY.0b013e31817bcc9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dai J, Miller AH, Bremner JD, Goldberg J, Jones L, Shallenberger L, Buckham R, Murrah NV, Veledar E, Wilson PW, Vaccarino V. Adherence to the Mediterranean diet is inversely associated with circulating interleukin-6 among middle-aged men: a twin study. Circulation. 2008;117:169–175. doi: 10.1161/CIRCULATIONAHA.107.710699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dai J, Jones DP, Goldberg J, Ziegler TR, Bostick RM, Wilson PW, Manatunga AK, Shallenberger L, Jones L, Vaccarino V. Association between adherence to the Mediterranean diet and oxidative stress. Am J Clin Nutr. 2008;88:1364–1370. doi: 10.3945/ajcn.2008.26528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goldberg J, Curran B, Vitek ME, Henderson WG, Boyko EJ. The Vietnam Era Twin Registry. Twin Res. 2002;5:476–481. doi: 10.1375/136905202320906318. [DOI] [PubMed] [Google Scholar]
- 22.Ridker PM, Rifai N, Stampfer MJ, Hennekens CH. Plasma concentration of interleukin-6 and the risk of future myocardial infarction among apparently healthy men. Circulation. 2000;101:1767–1772. doi: 10.1161/01.cir.101.15.1767. [DOI] [PubMed] [Google Scholar]
- 23.Lampert R, Bremner JD, Su S, Miller A, Lee F, Cheema F, Goldberg J, Vaccarino V. Decreased heart rate variability is associated with higher levels of inflammation in middle-aged men. Am Heart J. 2008;156:759 e751–757. doi: 10.1016/j.ahj.2008.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carlin JB, Gurrin LC, Sterne JA, Morley R, Dwyer T. Regression models for twin studies: a critical review. Int J Epidemiol. 2005;34:1089–1099. doi: 10.1093/ije/dyi153. [DOI] [PubMed] [Google Scholar]
- 25.Trichopoulou A, Kouris-Blazos A, Wahlqvist ML, Gnardellis C, Lagiou P, Polychronopoulos E, Vassilakou T, Lipworth L, Trichopoulos D. Diet and overall survival in elderly people. Bmj. 1995;311:1457–1460. doi: 10.1136/bmj.311.7018.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barr RG, Nathan DM, Meigs JB, Singer DE. Tests of glycemia for the diagnosis of type 2 diabetes mellitus. Ann Intern Med. 2002;137:263–272. doi: 10.7326/0003-4819-137-4-200208200-00011. [DOI] [PubMed] [Google Scholar]
- 27.Pols MA, Peeters PH, Bueno-De-Mesquita HB, Ocke MC, Wentink CA, Kemper HC, Collette HJ. Validity and repeatability of a modified Baecke questionnaire on physical activity. Int J Epidemiol. 1995;24:381–388. doi: 10.1093/ije/24.2.381. [DOI] [PubMed] [Google Scholar]
- 28.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 29.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 30.Baccarelli A, Cassano PA, Litonjua A, Park SK, Suh H, Sparrow D, Vokonas P, Schwartz J. Cardiac autonomic dysfunction: effects from particulate air pollution and protection by dietary methyl nutrients and metabolic polymorphisms. Circulation. 2008;117:1802–1809. doi: 10.1161/CIRCULATIONAHA.107.726067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fu CH, Yang CC, Lin CL, Kuo TB. Effects of long-term vegetarian diets on cardiovascular autonomic functions in healthy postmenopausal women. Am J Cardiol. 2006;97:380–383. doi: 10.1016/j.amjcard.2005.08.057. [DOI] [PubMed] [Google Scholar]
- 32.Millis RM, Austin RE, Bond V, Faruque M, Goring KL, Hickey BM, Blakely R, Demeersman RE. Effects of high-carbohydrate and high-fat dietary treatments on measures of heart rate variability and sympathovagal balance. Life Sci. 2009;85:141–145. doi: 10.1016/j.lfs.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 33.Wardle J, Cooke L. Genetic and environmental determinants of children's food preferences. Br J Nutr. 2008;99(1):S15–21. doi: 10.1017/S000711450889246X. [DOI] [PubMed] [Google Scholar]
- 34.de Castro JM. Heritability of hunger relationships with food intake in free-living humans. Physiol Behav. 1999;67:249–258. doi: 10.1016/s0031-9384(99)00065-7. [DOI] [PubMed] [Google Scholar]
- 35.Heitmann BL, Harris JR, Lissner L, Pedersen NL. Genetic effects on weight change and food intake in Swedish adult twins. Am J Clin Nutr. 1999;69:597–602. doi: 10.1093/ajcn/69.4.597. [DOI] [PubMed] [Google Scholar]
- 36.Singh JP, Larson MG, O'Donnell CJ, Tsuji H, Corey D, Levy D. Genome scan linkage results for heart rate variability (the Framingham Heart Study) Am J Cardiol. 2002;90:1290–1293. doi: 10.1016/s0002-9149(02)02865-5. [DOI] [PubMed] [Google Scholar]
- 37.Subar AF, Thompson FE, Kipnis V, Midthune D, Hurwitz P, McNutt S, McIntosh A, Rosenfeld S. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: the Eating at America's Table Study. Am J Epidemiol. 2001;154:1089–1099. doi: 10.1093/aje/154.12.1089. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.