Abstract
Newly arrived Mexican immigrants generally report better health in the United States than do native-born Americans, but this health advantage erodes over time. At issue is whether this advantage is illusory – or a product of disease that goes undiagnosed in Mexico but is discovered after immigration. Using the National Health and Nutrition Survey we compare clinical to self-reported diagnosed disease prevalence. We find that diagnosed prevalence is 47 percent lower among recent Mexican immigrants than among natives for both diabetes and hypertension, and that undiagnosed disease explains one third of this recent immigrant advantage for diabetes and one fifth for hypertension. The remaining health advantage might be explained by immigrant selectivity (how migrants differ from those in Mexico who stayed) or assimilation (the process of integration into the U.S.). Since undiagnosed disease can have adverse health consequences, medical practice should emphasize disease detection among new arrivals as part of routine doctor or hospital visits.
Introduction
There are 42 million foreign-born residents in the United States, accounting for 13 percent of the current size of the American population. Two-thirds of America’s population growth between 1995 and 2050 will be directly or indirectly due to immigration.1 As a result, the health status of Americans will increasingly reflect the health status of recent immigrants and their descendants. It is important then to monitor the health of the foreign-born population and its implications for the U.S. health care system.
Differences in health status of Mexican immigrants and native-born Americans have generated significant research in past decades. A key stylized fact is that upon arrival into the United States, Mexican immigrants report being in better health than do native-born Americans, but this health advantage disappears the longer they stay in the United States.2,3,4 This phenomenon — often called the “Healthy Immigrant Effect” — has been studied by researchers from many disciplines and has also been shown in other major immigrant-receiving countries. The effect is robust in measures of self-reported general health status (from excellent to poor) and in the presence of health conditions and activity limitations.3,4 Mexican immigrants are also found to have lower rates of mortality than Mexican and non-Mexican heritage Americans.5,6,7
The reasons underlying the Healthy Immigrant Effect have been a source of considerable debate. One explanation is based on selective immigration and return-migration: If healthy immigrants are more likely to come to the U.S. or unhealthy immigrants more likely to return to their home country, we will observe that immigrants are generally healthier than native-born Americans.2,8,9 Another explanation uses assimilation: If immigrants are exposed to a more harmful environment or adopt a more harmful lifestyle – say through diet and exercise – than they had in their native country, their health status could decline over time in the U.S.3,8,10,11,12
One possible explanation receiving less attention stems from improved health care access as a consequence of immigration. The hypothesis is that immigrants from countries with poor access to health services may come with pre-existing, undiagnosed health problems. Upon arrival in the U.S., they are exposed to a more accessible health care system and become more aware of these conditions. If so, improved care access can explain part of the initial immigrant health advantage as well as its subsequent erosion. One important difference between this hypothesis and others is that it implies immigrants might not truly be in better physical health than natives — a finding with important implications for health policy.
This article focuses on the Healthy Immigrant Effect with respect to diabetes and hypertension, two prevalent chronic diseases in the Mexican American population. We use direct measures of undiagnosed disease — through clinical and laboratory tests — to investigate if these patterns can be explained by disease awareness. We measure awareness as the fraction of those with the disease (defined as those who either self-reported they were doctor-diagnosed or who are above the clinical thresholds) who report being told by a doctor that they have the disease.
Study Data and Methods
Data
This research uses yearly data from the National Health and Nutrition Examination Survey (NHANES) from 1988–1994 and from 1999–2008. The survey examines a nationally representative sample of about 5,000 persons each year. To have sufficient sample sizes to investigate patterns for different immigrant groups, we pool data from different years. NHANES provides crucial information about respondents’ immigrant status and characteristics.
The key advantage of NHANES is that, in addition to self-reported data, it assesses health status through comprehensive physical examinations and laboratory tests (blood, urine, and swabs) conducted around the same time as the home interview by a physician in a mobile health center. This allows us to identify health conditions that respondents didn’t know they had but surface through clinical testing.
Diabetes and Hypertension Prevalence Measures
We investigate clinical prevalence, diagnosed prevalence, and awareness of hypertension and diabetes, using the following specific measures:
Self-reported disease status: a person has a diagnosed condition (hypertension or diabetes) if in NHANES she reports that a doctor told her that she had the disease.
Clinical hypertension: following the literature,13,14 we use the mean of the second and third reading of systolic and diastolic blood pressure measured during the physical exam. Based on standard definitions, we consider a person to be hypertensive if he or she has over 140 mmHg systolic or over 90 mmHg diastolic pressure.15,16,17
Clinical diabetes: we follow the standard convention by using values of glycosylated hemoglobin (HbA1c) equal or greater than 6.5 percent.18,19 HbA1c is highly correlated with fasting plasma glucose levels and is a frequently used measure of clinical diabetes in academic studies.19,20
Total prevalence: a person is considered to have either condition if she reported that a doctor told her she had the condition or had a clinical value above the diagnostic threshold.
Awareness: a person has undiagnosed disease if she did not report being previously diagnosed but an examination subsequently reveals it.
A non-trivial fraction of clinical values is missing from the final pooled dataset: 9.8 percent for clinical diabetes and 8.7 percent for clinical hypertension (see Appendix Table A).21 These missing values are due to refusals of laboratory or physical exams, or to conditions that prevent the exam from being performed. (Examples are rashes, open wounds, or if blood had been drawn from participant within the previous week). Self-reported prevalence of diabetes and hypertension are not statistically different in a comparison of those with and without clinical values missing. Other studies using NHANES reported similar fractions of missing values.22
Risk Factors
In addition to years since immigration, we use as covariates the following risk factors — age, race, years of education, income, having health insurance, smoking, and being overweight or obese. Dummies for low, middle, and high income are constructed by dividing respondents into three equal year-specific income terciles in each NHANES. Each respondent is categorized into low, middle or high income relative to other respondents in the same survey year avoiding complications due to inflation or income increases over time. Health insurance refers to coverage by any insurance type (public, employer provided, or individual) and smoking to whether respondents currently smoke. NHANES measures respondents’ height and weight during the physical test so that body mass index (BMI) can be computed; with it, an objective assessment can be made of whether the respondent is obese (BMI>=30) or overweight (BMI>=25 and <30).
Immigrant Status
Mexican immigrants are those born in Mexico. Mexican Americans are born in the U.S. but who define themselves as Mexican Americans in the ethnicity question and who are presumably second-generation immigrants or higher. Our definitions are conventional, though there is always some imprecision in defining ancestry because of mixed heritage in family backgrounds and different propensities to claim a particular heritage.1 An important variable for analysis is tenure in the U.S., derived from a question asking the year foreign-born respondents came to the United States “to stay”.
Analysis
We estimate Ordinary Least Squares (OLS) models — weighted to account for the NHANES design – to explain diagnosed, undiagnosed, and total hypertension and diabetes prevalence as a function of individual characteristics. We use repeated cross-sectional analysis with several NHANES survey waves. Our main interest is differences in total disease prevalence, diagnosis, and awareness between native-born Americans of non-Mexican heritage, Mexican Americans, Mexican-born immigrants, and recent versus non-recent Mexican immigrants.
Raw comparisons of disease prevalence might be misleading due to differences in risk factors across groups, as shown in Appendix Table B. We control for individual characteristics in a multivariate regression framework (see Appendix Table C).21 Based on our estimated models, we calculate predicted probabilities of being hypertensive or diabetic for different subgroups holding individual characteristics constant (Exhibits 2 to 5). For example, to compare the characteristic-adjusted diabetes total prevalence rate between non-Mexican Native-born Americans and Mexican immigrants, we used our OLS estimates to predict the probability of being hypertensive or diabetic for each of the two groups if both groups had individual characteristics equal to the sample mean. Therefore, differences in predicted probabilities presented in the figures cannot be attributed to measured differences between groups (in this case non-Mexican native-born Americans and Mexican immigrants) in characteristics included in the model.
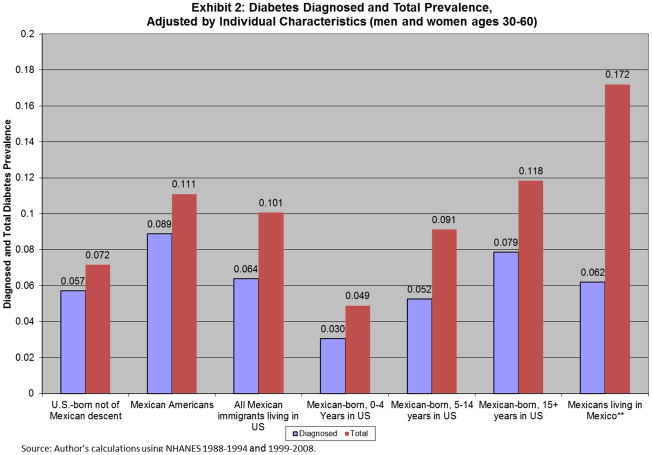
Exhibit 2. Diabetes Diagnosed and Total Prevalence, Adjusted by Individual Characteristics (men and women ages 30–60).
SOURCE: Authors’ calculations using NHANES and the 2000 Mexican National Health Survey (for Diabetes levels among Mexicans in Mexico).
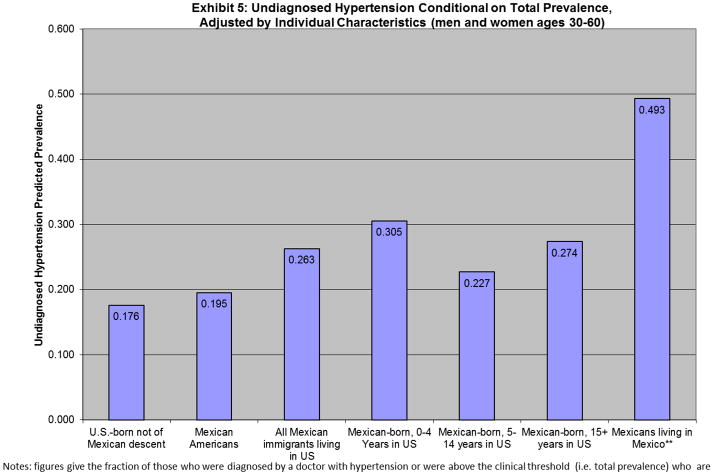
Exhibit 5.
Undiagnosed Hypertension Conditional on Total Prevalence, Adjusted by Individual Characteristics (men and women ages 30–60).
SOURCE: Authors’ calculations using NHANES and the 2000 Mexican National Health Survey (for Hypertension levels among Mexicans in Mexico).
Notes: figures give the fraction of those who were diagnosed by a doctor with hypertension or were above the clinical threshold (i.e. total prevalence) who are not aware they have hypertension.
Our sample is restricted to males and females ages 30–60 years of age. Prevalence of hypertension and diabetes for individuals over 30 are high enough to make analysis feasible with NHANES sample sizes. Moreover, we restrict the sample to people below 60 to avoid the possibility of negative health selection of older immigrants, as people who move to the U.S. when they are above 60 often do so to take advantage of better treatment here.2,18 Our analysis applies only to Mexican immigrants who come to the United States within this age group.
Limitations
There are several limitations to this research. The primary limitation is lack of panel data tracking immigrants from time of their arrival well into their stay in the U.S. Because of this, we relied on synthetic cohort techniques to trace average experiences of immigrants over time. Synthetic cohorts follow groups of people in population studies in different years allowing groups to age by differences in calendar time between years of population studies. Rather than tracking the same group from one year to the next, synthetic cohorts capture different groups of people (eg. immigrants) who lived in this country for different time intervals– hopefully simulating what happens if they were tracked over time. Cohort effects in prevalence and diagnosis of disease could affect these synthetic cohort patterns. We tested for cohort effects in our sample of new entrants and did not find any statistically significant differences, but sample sizes are relatively small.
Since we focus on the Mexican immigrant experience, we are limited by standard complexities of defining Mexican heritage. Our data for people living in Mexico are not strictly comparable to data for Mexicans living in the U.S. due to a different test for clinical diabetes (fasting glucose instead of HbA1C) for a population in Mexico who largely did not follow instructions to fast. Finally, because we rely on observational data, this study can identify strong suggestive correlations but not strict causal links.
Study Results
Socioeconomic Differences by Country of Origin and Time in U.S
Appendix Table B shows summary statistics for immigrants born in Mexico and immigrants born elsewhere, along with U.S.-born people of Mexican descent (Mexican Americans) and U.S.-born people not of Mexican descent.21 The data for Mexican immigrants are presented by length of tenure in the U.S. All differences across groups discussed below have been found to be statistically significant at the 0.05 level. While standard demographics (age and gender) of these populations are generally similar, Mexican immigrants on average have fewer years of education, lower income, and a lower probability of having health insurance than both Mexican and non-Mexican Americans as well as immigrants from other countries. While Mexican immigrants are more likely to be overweight than other immigrants, their smoking and obesity rates are about the same.
Compared to all other groups, Mexican immigrants are significantly less likely to be covered by health insurance. The gap is large for Mexican immigrants in the U.S for less than five years) — only 23 percent have health insurance compared to 86 percent of native-born Americans of non-Mexican heritage and 77 percent of Mexican Americans. These low rates of health insurance, which do grow over time as the length of stay increases, are due largely to the undocumented status of many recent Mexican immigrants.23
Because risk factors such as age and overweight/obese are related to diabetes and hypertension prevalence, differences across U.S.-born residents and Mexican immigrants in Appendix Table B emphasize the importance of taking these factors into account when comparing prevalence across groups.21 In any year Mexicans immigrants are younger compared to native-born Americans of Mexican or Non-Mexican heritage — which should lead to lower disease prevalence, but they are significantly more likely to be uninsured.
Diabetes and Hypertension prevalence
Exhibit 1 displays alternative measures of diabetes and hypertension prevalence for our demographic groups. These figures are simple weighted averages for each group not adjusted for differences in individual characteristics shown in Appendix Table B (for adjusted figures see Exhibits 2 to 5).21 The data in this exhibit provide suggestive evidence that undiagnosed disease may partly explain the Healthy Immigrant Effect for diabetes and hypertension among Mexican immigrants. To illustrate for diabetes, 58.5 percent of immigrants with diabetes in their first four years in the U.S. are undiagnosed compared to 29.5 percent for those here for fifteen or more years.
Exhibit 1.
Diabetes and Hypertension Prevalence, men and women ages 30–60
| U.S.- born not of Mexican descent | Mexican Americans | Immigrants not born in Mexico
|
Immigrants born in Mexico | ||||
|---|---|---|---|---|---|---|---|
| All Mexican- born immigrants | 0–4 years in US | 5–14 years in US | 15 or more years in US | ||||
|
|
|||||||
| Diabetes Prevalence | |||||||
| Diagnosed, % | 5.8 | 8.9** | 6.5 | 6.6 | 1.8 | 5.0 | 9.0** |
| Clinical, % | 5.2 | 9.2** | 6.5* | 8.3** | 3.8 | 6.2 | 10.8** |
| Total Prevalence, % | 7.2 | 11.3** | 8.8* | 10.5** | 4.7 | 8.6 | 13.3** |
| Undiagnosed, as a % of Total Prevalence | 21.3 | 22.6 | 24.1 | 33.7** | 58.5* | 38.2* | 29.5 |
| Hypertension Prevalence | |||||||
| Diagnosed, % | 26.0 | 25.2 | 18.4** | 13.7** | 10.0** | 11.8** | 15.9** |
| Clinical, % | 13.0 | 14.5 | 11.9 | 8.5** | 5.3* | 6.6** | 10.5 |
| Total Prevalence, % | 31.4 | 30.9 | 24.0** | 18.6** | 14.6** | 16.0** | 21.3** |
| Undiagnosed, as a % of Total Prevalence | 17.9 | 19.6 | 22.6* | 28.8** | 33.3 | 28.2* | 28.6* |
| Sample Size | 14,124 | 2,081 | 2,137 | 2,666 | 365 | 883 | 1,418 |
Notes: averages weighted using survey weights for the different subgroups, pooled data from NHANES 1988–1994 and 1999–2008. Diagnosed prevalence is the fraction who had a doctor diagnose the disease, clinical prevalence is the fraction above the HbA1c (or blood pressure readings) clinical threshold. Total prevalence is the fraction either diagnosed or above the clinical threshold. Undiagnosed is the fraction all diabetics (or hypertensive) who have not been diagnosed. Subscripts denote figures that are statistically different than the means for U.S.-born not of Mexican descent. + significant at 10%;
significant at 5%;
significant at 1%.
Source: Author’s calculations using NHANES 1988–1994 and 1999–2008.
For each of these two diseases, this exhibit shows four measures of disease prevalence: diagnosed (based on self-reports), clinical (based on physical or laboratory exams), total (either self-reported or clinical) and the percent undiagnosed (the fraction of total prevalence not diagnosed).
The numbers for diagnosed prevalence of both diseases show the already documented “effect” — recent Mexican immigrants in the U.S. for less than five years report being in much better health upon arrival than their native-born American counterparts but this health advantage erodes over time as length of stay in the U.S. increases. The fraction of recent Mexican immigrants reporting ever being diagnosed with diabetes (1.8 percent) or hypertension (10.0 percent) is significantly lower than the same fraction for Mexican and non-Mexican Americans, but increases as we focus on Mexican immigrants in the United States longer.
Examining clinical diagnosis, however, the Healthy Immigrant Effect is attenuated. Even though recent Mexican immigrants still appear to be healthier, relative differences are not as large. Clinical diabetes prevalence for all recent Mexican immigrants is 3.8 percent, about three-quarters of diabetes prevalence of native-born Americans of non-Mexican descent (5.2%). Total disease prevalence — which includes diagnosed and undiagnosed disease — paints a picture where recent Mexican immigrants are not as healthy as traditional measures (diagnosed prevalence) suggest.
Finally, undiagnosed prevalence as a fraction of total prevalence is significantly larger among immigrants from Mexico, a country where access to health care among the poor is arguably much worse than in the United States. The fraction is particularly high among recent Mexican immigrants. Fifty-nine percent of recent Mexican immigrants who are diabetic are undiagnosed and a third who are hypertensive are undiagnosed. Comparable rates for native-born Americans are about a fifth for both diabetes and hypertension. Moreover, for Mexican immigrants, undiagnosed disease as a fraction of total prevalence decreases steeply for diabetes the longer they stay in the U.S. The patterns in Exhibit 1 suggest that lower disease awareness among Mexican immigrants – and increases in awareness with time in the U.S. — may be important when interpreting the Healthy Immigrant Effect.
Disease prevalence analysis
We analyzed determinants of diagnosed, total, and undiagnosed diabetes and hypertension prevalence by estimating Ordinary Least Squares (OLS) models investigating factors related to these prevalence measures. Estimated parameters of OLS models are presented in the Online Appendix.21 Since the main patterns of our interest concern comparisons between Mexican immigrants and native-born Americans of Mexican and non-Mexican heritage, we restricted the sample to respondents in these groups, dropping immigrants from countries other than Mexico who constituted 9 percent of the total sample. Native-born Americans of non-Mexican descent are the excluded group in these models, and we include dummy variables for Mexican Americans and three groups of Mexican immigrants based on their time since immigration (0–4, 5–14, and 15 or more years since immigration).
The other co-variates are age, gender (1= male), race (1=black), three education and income groups (in both cases the left-out group is the lowest category), dummy variables for being a smoker, being overweight, and being obese, and sets of dummy variables indicating the NHANES survey year in which a respondent participated. The first four columns of Online Appendix Table C show estimated results for diagnosed and total disease prevalence for diabetes and hypertension.21 Results are consistent with previous research on the importance of certain risk factors for diabetes and hypertensive prevalence.14,18 For both diseases, diagnosed and total prevalence declines as education or income increases or as age decreases, and is higher among black respondents and among men (especially for total prevalence). Being overweight or obese are strongly related to the probability of reporting being diagnosed or having the condition. Of particular interest, respondents who are not covered by health insurance are less likely to be diagnosed for either diabetes or hypertension.
These regressions show that Mexican Americans are more likely to have diabetes but no more likely to be hypertensive than are native-born Americans not of Mexican descent. Recent Mexican immigrants have a diagnosed diabetes prevalence 2.7 percentage points lower than native-born Americans of non-Mexican heritage. This compares to a 4 percentage point lower rate in the raw data in Exhibit 1, indicating that attributes in the regressions can explain only part of the Healthy Immigrant Effect for diabetes among recent Mexican immigrants.
If we perform the same calculation for diagnosed hypertension, we find that co-variates in the model accounts for only part of the Healthy Immigrant Effect for recent Mexican immigrants. Compared to the raw difference of 16 percentage points in Exhibit 1, our model predicts a 13 percentage point lower diagnosed hypertension among recent Mexican immigrants.
We looked more directly at the role of undiagnosed diabetes and hypertension and factors related to it by restricting the sample to those who either have total diabetes or hypertension (diagnosed or undiagnosed)and constructing a dummy variable for those undiagnosed. We present these OLS analysis in the last two columns of Online Appendix Table C.21
Mexican immigrants, especially recent Mexican immigrants, who are either diabetic or hypertensive are more likely to have been undiagnosed than both Mexican Americans and U.S. born people of non-Mexican heritage. The enhanced probability of having undiagnosed diabetes or hypertension declines among Mexican immigrants in the U.S. fourteen years or more – though the probability declines more steeply for those with diabetes. For both diseases, having health insurance is a strong predictor of being diagnosed. Previous research on factors related to undiagnosed diabetes and hypertension found similar results.15,19
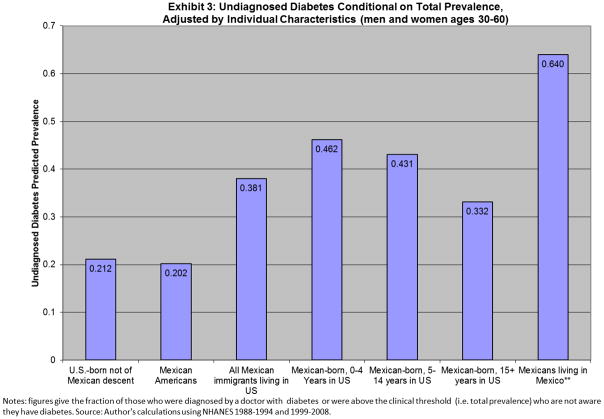
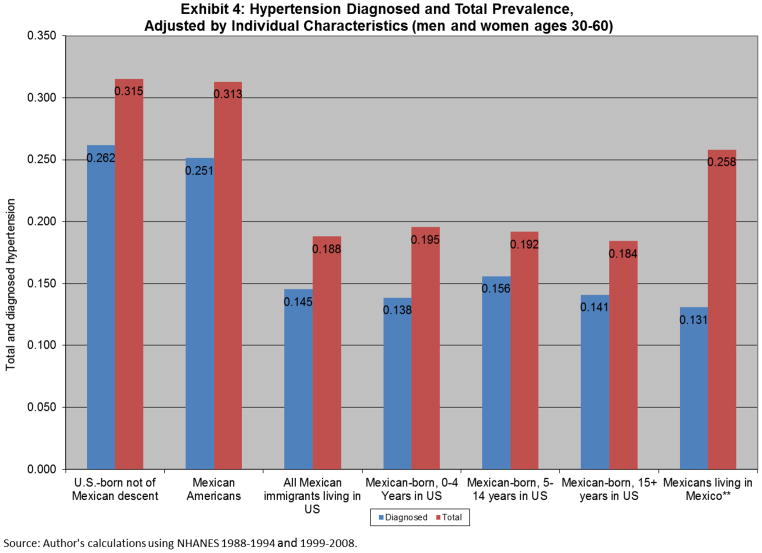
Simulations
Based on these estimated prevalence models in Online Appendix C,21 we computed predicted probabilities of being diagnosed and having diabetes or hypertension, adjusted for all attributes in the models. Results are displayed graphically in Exhibits 2–3 for diabetes and Exhibits 4–5 for hypertension.
Exhibit 3. Undiagnosed Diabetes Conditional on Total Prevalence, Adjusted by Individual Characteristics (men and women ages 30–60).
SOURCE: Authors’ calculations using NHANES and the 2000 Mexican National Health Survey (for Diabetes levels among Mexicans in Mexico).
Notes: figures give the fraction of those who were diagnosed by a doctor with diabetes or were above the clinical threshold (i.e. total prevalence) who are not aware they have diabetes.
Exhibit 4.
Hypertension Diagnosed and Total Prevalence, Adjusted by Individual Characteristics (men and women ages 30–60).
SOURCE: Authors’ calculations using NHANES and the 2000 Mexican National Health Survey (for Hypertension levels among Mexicans in Mexico).
Exhibit 2 shows predicted diagnosed and total diabetes prevalence for our demographic groups. The blue bars show predicted probabilities of having diagnosed diabetes. Since predictions are adjusted for all included individual characteristics in Online Appendix Exhibit C,21 differences in included characteristics between groups cannot explain differences in disease prevalence in this figure. For comparative purposes, the final two bars in Exhibit 2 show data on diagnosed and total diabetes for a random sample of Mexicans living in Mexico in the same age group (the 2000 Mexican National Health Survey). One caution in interpreting data on total diabetes prevalence for the Mexican sample is that, although fasting glucose was used, much of the sample did not fast in the last twelve hours. A 12-hour fast is normally required for an accurate measure.
For those born in the United States, these characteristic adjusted figures closely follow the raw prevalences shown in Exhibit 1, which is not surprising as characteristics of groups are not that different (see Appendix Table B). The major effect of these adjustments occurs among Mexican immigrants and among these Mexican immigrants those who most recently came to the US.
Consider first the most recent Mexican immigrants. Their diagnosed diabetes rate in Exhibit 1 was 1.8 percent, 4.1 percentage points less than our comparison group of Mexican Americans (5.9 percent). Adjusted for all characteristics in the model, we predict a diagnosed rate for recent Mexican immigrants of 3 percent, 2.7 percentage points less than the comparison group of Native born Americans not of Mexican descent. Attributes included in the model explain part but not all the low rate of diagnosed diabetes among recent Mexican immigrants.
We find similar but more attenuated patterns for Mexican immigrants who have stayed longer in the U.S. The characteristic adjusted increase in diagnosed diabetes as time since immigration increases is considerably smaller. Our raw numbers in Exhibit 1 indicated that diagnosed diabetes increased from 1.8 percent to 9.0 percent while our attribute adjusted rates in Exhibit 2 indicate a rise in diagnosed diabetes from 3.0 percent to 7.9 percent. Thus, a significant part but, once again, not all increases in diagnosed diabetes for Mexican immigrants as time passes reflects a larger likelihood that diabetes will be diagnosed.
Total diabetes prevalence is higher among Mexican Americans and Mexican immigrants than among native-born Americans who are not of Mexican descent, indicating that Mexicans generally have higher risk for diabetes. Adjusted prevalence data for Mexican immigrants also reveal a significant amount of undiagnosed diabetes, more so than exists among Mexican Americans. This view is supported by the high prevalence of diabetes and the large fraction of diabetics who are undiagnosed in our sample of Mexicans living in Mexico in the last two columns.
To calculate how much of the recent immigrant advantage in diabetes is explained by undiagnosed disease, we can compare diagnosed and total rates for Mexican born with less than five years in the US and U.S.-born not of Mexican descent in Exhibit 2. The covariate-adjusted advantage in diagnosed prevalence is 2.7 percentage points, or 47 percent of the U.S.-born prevalence (0.027/0.057). In contrast, the advantage in total prevalence (taking into account undiagnosed disease) is only 2.3 percentage points, or 32 percent (0.023/0.072). Therefore, undiagnosed disease explains about a third of the total recent immigrant advantage.
Exhibit 3 presents graphically our characteristic adjusted fraction of diabetics who are undiagnosed. The percent of diabetics who are undiagnosed is about the same among the US-born population whether they are of Mexican descent or other heritage. These similar rates have been shown to be the result of the NIH campaign to reduce undiagnosed disease in minority groups.18 In sharp contrast, adjusted rates of undiagnosed diabetes for all sub-sets of Mexican immigrants are much higher, especially for recent Mexican immigrants. The fraction of diabetics undiagnosed among recent Mexican immigrants is 2.3 times higher than for Mexican Americans with similar characteristics. This graph is consistent with the hypothesis that undiagnosed disease falls with time in the country. The final column suggests that undiagnosed diabetes is an even larger problem among non-migrants who stayed in Mexico.
Exhibits 4 and 5 provide an identical analysis for hypertension. The final two columns in Exhibit 4 present data on diagnosed and total hypertension prevalence for a random sample of Mexicans living in Mexico in the same age group (the 2000 Mexican National Health Survey using the same criteria for diagnosed and clinical prevalence). Compared to Mexican immigrants living in the U.S., undiagnosed hypertension is an even more severe problem among those living in Mexico (50 percent of hypertensives are undiagnosed). Mexican immigrants to the U.S. are positively selected in terms of their hypertension status. No matter what the duration of immigration, total prevalence of hypertension is lower among Mexican immigrants than among Mexicans living in their native country.
We can use figures in Exhibit 4 for recent Mexican immigrants and U.S.-born not of Mexican descent to calculate how much of the recent immigrant advantage in hypertension is explained by differences in disease awareness. The self-reported hypertension advantage, given by the diagnosed rates, is 12.4 percentage points, or 47 percent of the diagnosed prevalence among U.S.-born (0.124/0.262). In contrast, the total hypertension advantage (taking into account undiagnosed hypertension) is 0.120 or 38 percent of total prevalence for non-Mexican natives (0.120/0.315). Therefore, differences in undiagnosed hypertension explain one fifth of the recent immigrant advantage.
Exhibit 5 shows that for hypertension, the percent undiagnosed is higher for Mexican immigrants than for the US-born population of either Mexican or non-Mexican heritage, but it is much lower than among those living in Mexico. At least for hypertension, Mexican immigrants are positively selected in that their true hypertension rates are much lower than rates for those living in Mexico. In addition, Mexican immigrants have lower rates of undiagnosed hypertension (compared to non-migrants in Mexico) even though those rates of undiagnosed hypertension are higher than those of Native-born Americans of either Mexican or non-Mexican descent.
Discussion
Our diabetes and hypertension analysis suggests that the primary “healthy immigrant” patterns for Mexican immigrants still remains when we use a more comprehensive measure of diabetes and hypertension prevalence that takes into account large levels of undiagnosed disease among Mexican immigrants. However, the magnitude of the Healthy Immigrant Effect is lessened once these comprehensive measures of prevalence are used. Undiagnosed disease explains about one third of the recent immigrant advantage for diabetes and one fifth for hypertension. These trends indicate that large levels of undiagnosed disease are a significant component of our understanding of the health of Mexican immigrants in the U.S.
The “Healthy Immigrant Effect” that remains after accounting for undiagnosed disease is consistent with a large literature that documents that Mexican immigrants in the U.S. have lower mortality rates than native-born Americans5,6,7 and might be explained by changing immigrant selectivity across cohorts or immigrant assimilation to the American lifestyle.12,13
Our analysis of undiagnosed diabetes reveals that lack of disease awareness is a serious problem among recent Mexican immigrants: almost half of recent migrants with diabetes are unaware they have the disease, an undiagnosed prevalence 2.3 times higher than among Mexican Americans with similar characteristics. In the case of hypertension, positive selection is evident among Mexicans coming to the U.S., with Mexican immigrants having hypertension prevalence significantly lower than the prevalence for the Mexican population in Mexico.
This research quantifies effects of immigration on disease awareness. Doing so is important given the growth of the foreign-born population and potential effects of immigrant health to the U.S. health care system. Our results reveal that Mexican immigrants are not as healthy as previously thought when undiagnosed disease is taken into account, particularly with respect to diabetes. The large differences in disease awareness point to the importance of screening recent immigrants to avoid late diagnosis and any potential costs of delayed treatment. Recent research suggests that disparities in awareness might translate into disparities in health.24,25
While we find little evidence that health insurance plays much of a role in preventing these diseases, we did find that having health insurance was an important factor in promoting awareness of both hypertension and diabetes. Awareness is the first step toward effective treatment, especially in populations with high rates of undiagnosed disease. Providing health insurance to undocumented immigrants is a complex subject that begins with rules on whom should be eligible to receive benefits, a subject on which this paper provides no insight. If benefits are to be provided, assistance in disease diagnosis should surely top the list of most cost-effective benefits.
Supplementary Material
ONLINE APPENDIX TABLE A (table)
Missing Observations
SOURCE: NHANES 1988–1994 and 1999–2008
ONLINE APPENDIX TABLE B (table)
Socioeconomic Differences by Country of Origin and Time in the US, Men and Women Ages 30–60
SOURCE: NHANES 1988–1994 and 1999–2008
Notes: averages weighted using survey weights for the different subgroups, pooled data from NHANES 1988–1994 and 1999–2008. Age is measured in years of age. All other variables are the fraction of people in that attribute in the specific sample indicated in the columns. Subscripts denote figures that are statistically different than the means for U.S.-born not of Mexican descent. + significant at 10%; * significant at 5%; ** significant at 1%.
ONLINE APPENDIX TABLE C (table)
Models for Diagnosed, Total and Undiagnosed Disease Probabilities, men and women ages 30–60, U.S. and Mexican-born
SOURCE: NHANES 1988–1994 and 1999–2008
Notes: LPM estimates. All regressions use survey weights. Reference categories: U.S-born not of Mexican descent, female, non-Black, less than 12 years of education, low income, no Health Insurance, non-smoker, not overweight or obese, NHANES year 1988–1991. Robust standard errors in brackets. *** p<0.01, ** p<0.05, * p<0.1.
Notes
- 1.Smith JP, Edmonson B, editors. The new Americans: economic, demographic and fiscal effects of immigration. Washington: National Academies Press; 1997. [Google Scholar]
- 2.Jasso G, Massey DS, Rosenzweig MR, Smith JP. Immigrant health selectivity and acculturation. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical perspectives on racial and ethnic differences in health in late life. Washington: National Academies Press; 2004. pp. 227–66. [PubMed] [Google Scholar]
- 3.Stephen EH, Foote K, Hendershot GE, Schoenborn CA. Health of the foreign-born population. Advance Data from Vital and Health Statistics. 1994;241:1–10. [PubMed] [Google Scholar]
- 4.Antecol H, Bedard K. Unhealthy assimilation: why do immigrants converge to American health status levels? Demography. 2006;43(2):337–60. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- 5.Hayes-Bautista DE. The Latino health research agenda in the twenty-first century. In: Suárez-Orozco MM, Páez MM, editors. Latinos: Remaking America. Cambridge, MA: Harvard University Press; 2002. pp. 215–35. [Google Scholar]
- 6.Markides KS, Eschbach K. Aging, migration, and mortality: current status of research on the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. 2005;60:68–75. doi: 10.1093/geronb/60.special_issue_2.s68. [DOI] [PubMed] [Google Scholar]
- 7.Palloni A. Paradox lost: explaining the Hispanic adult mortality advantage? Demography. 2004;41(3):385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- 8.Marmot MG, Syme SL. Acculturation and coronary heart disease in Japanese-Americans. Am J Epidemiol. 1976;104:225–47. doi: 10.1093/oxfordjournals.aje.a112296. [DOI] [PubMed] [Google Scholar]
- 9.Palloni A, Arias E. CDE Working Paper No 2003-01. Center for Demography and Ecology, University of Wisconsin-Madison; 2003. A re-examination of the Hispanic mortality paradox. [Google Scholar]
- 10.Kasl SV, Berkman L. Health consequences of the experiences of migration. Ann Rev Publ Health. 1983;4:69–90. doi: 10.1146/annurev.pu.04.050183.000441. [DOI] [PubMed] [Google Scholar]
- 11.Allen Michele L, Elliott Marc N, Morales Leo S, Diamant Allison L, Hambarsoomian Katrin, Schuster Mark A. Adolescent Participation in Preventive Health Behaviors, Physical Activity, and Nutrition: Differences Across Immigrant Generations for Asians and Latinos Compared With Whites. Amer J Public Health. 2007;97(2):337–43. doi: 10.2105/AJPH.2005.076810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perez-Escamilla R, Predrag P. The Role of Acculturation in Nutrition, Lifestyle, and Incidence of Type 2 Diabetes among Latinos. J Nutr. 2007;137(4):860–70. doi: 10.1093/jn/137.4.860. [DOI] [PubMed] [Google Scholar]
- 13.Johnston DW, Propper C, Shields MA. Comparing subjective and objective measures of health: evidence from hypertension for the income/health gradient. J Health Econ. 2009;28:540–52. doi: 10.1016/j.jhealeco.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 14.Chatterji P, Joo H, Lahiri K. NBER Working Paper No 16578. 2010. Beware of unawareness: Racial/ethnic disparities in awareness of chronic diseases. [Google Scholar]
- 15.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness and management. Arch Intern Med. 2005;165:2098–104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 16.Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE. Understanding social disparities in hypertension prevalence, awareness and control: the role of neighborhood context. Soc Sci Med. 2007;65:1853–66. doi: 10.1016/j.socscimed.2007.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Angell SY, Garg RK, Gwynn RC, Bash L, Thorpe L, Frieden TR. Prevalence, awareness, treatment and predictors of control of hypertension in New York City. Circ, Cardiovasc Quality and Outcomes. 2008;1:46–53. doi: 10.1161/CIRCOUTCOMES.108.791954. [DOI] [PubMed] [Google Scholar]
- 18.Smith JP. Nature and causes of trends in male diabetes prevalence, undiagnosed diabetes, and the socioeconomic status health gradient. PNAS. 2007;104(33):13225–31. doi: 10.1073/pnas.0611234104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldman N, Lin I, Weinstein M, Lin Y. Evaluating the quality of self-reports of hypertension and diabetes. J Clin Epidemiol. 2003;56:148–54. doi: 10.1016/s0895-4356(02)00580-2. [DOI] [PubMed] [Google Scholar]
- 20.Gregg E, Cheng Y, Cadwell B, Imperatore G, Williams D, Flegal K, Narayan K, Venkat K, Williamson D. Secular trends in cardiovascular disease risk factors according to Body Mass Index in US Adults. J Am Med Assoc. 2005;293:1868–74. doi: 10.1001/jama.293.15.1868. [DOI] [PubMed] [Google Scholar]
- 21.Please refer to online appendix for further information. To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 22.Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. Am J Public Health. 2007;97(7):1305–10. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goldman D, Smith JP, Sood N. Immigrants and the cost of medical care. Health Aff (Millwood) 2006;25(6):1700–11. doi: 10.1377/hlthaff.25.6.1700. [DOI] [PubMed] [Google Scholar]
- 24.Cutler DM, Lleras-Muney A. Understanding differences in health behaviors by education. J Health Econ. 2010;29:1–28. doi: 10.1016/j.jhealeco.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aizer A, Stroud L. NBER Working Paper No 15840. 2010. Education, knowledge and the evolution of disparities in health. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ONLINE APPENDIX TABLE A (table)
Missing Observations
SOURCE: NHANES 1988–1994 and 1999–2008
ONLINE APPENDIX TABLE B (table)
Socioeconomic Differences by Country of Origin and Time in the US, Men and Women Ages 30–60
SOURCE: NHANES 1988–1994 and 1999–2008
Notes: averages weighted using survey weights for the different subgroups, pooled data from NHANES 1988–1994 and 1999–2008. Age is measured in years of age. All other variables are the fraction of people in that attribute in the specific sample indicated in the columns. Subscripts denote figures that are statistically different than the means for U.S.-born not of Mexican descent. + significant at 10%; * significant at 5%; ** significant at 1%.
ONLINE APPENDIX TABLE C (table)
Models for Diagnosed, Total and Undiagnosed Disease Probabilities, men and women ages 30–60, U.S. and Mexican-born
SOURCE: NHANES 1988–1994 and 1999–2008
Notes: LPM estimates. All regressions use survey weights. Reference categories: U.S-born not of Mexican descent, female, non-Black, less than 12 years of education, low income, no Health Insurance, non-smoker, not overweight or obese, NHANES year 1988–1991. Robust standard errors in brackets. *** p<0.01, ** p<0.05, * p<0.1.