Abstract
AIM: To assess adalimumab’s efficacy with concomitant azathioprine (AZA) for induction and maintenance of clinical remission in Japanese Crohn’s disease (CD) patients.
METHODS: This retrospective, observational, single-center study enrolled 28 consecutive CD patients treated with adalimumab (ADA). Mean age and mean disease duration were 38.1 ± 11.8 years and 11.8 ± 10.1 years, respectively. The baseline mean Crohn’s disease activity index (CDAI) and C-reactive protein were 177.8 ± 82.0 and 0.70 ± 0.83 mg/dL, respectively. Twelve of these patients also received a concomitant stable dose of AZA. ADA was subcutaneously administered: 160 mg at week 0, 80 mg at week 2, followed by 40 mg every other week. Clinical response and remission rates were assessed via CDAI and C-reactive protein for 24 wk.
RESULTS: The mean CDAI at weeks 2, 4, 8, and 24 was 124.4, 120.2, 123.6, and 135.1, respectively. The CDAI was significantly decreased at weeks 2 and 4 with ADA and was significantly suppressed at 24 wk with ADA/AZA. Overall clinical remission rates at weeks 4 and 24 were 66.7% and 63.2%, respectively. Although no statistically significant difference in C-reactive protein was demonstrated, ADA with AZA resulted in a greater statistically significant improvement in CDAI at 24 wk, compared to ADA alone.
CONCLUSION: Scheduled ADA with concomitant AZA may be more effective for clinical remission achievement at 24 wk in Japanese Crohn’s disease patients.
Keywords: Crohn’s disease, Adalimumab, Immunomodulator, Azathioprine, Inflammatory bowel disease
Core tip: In this study, the authors found that adalimumab (ADA) treatment with concomitant azathioprine usage significantly suppressed the Crohn’s disease activity index and increased the remission rate at 24 wk after the initiation of therapy, compared with ADA treatment alone.
INTRODUCTION
Tumor necrosis factor-α (TNF-α) is a proinflammatory cytokine implicated in the pathogenesis of inflammatory bowel disease (IBD)[1-3]. Thus far, a variety of therapeutic approaches have been used to inhibit TNF-α in patients with IBD, including infliximab (IFX), which was the first biologic agent approved for the treatment of IBD[4]. IFX is a mouse and human chimeric immunoglobulin G1 (IgG1) monoclonal antibody directed against TNF-α; it binds to both the soluble and transmembrane forms of TNF-α and is effective as both an induction and maintenance therapy in patients with Crohn’s disease (CD), including patients who have draining fistulas[5-8]. However, IFX has a 25% murine fraction that has potent immunogenicity and can cause the formation of human anti-chimeric antibodies (HACA)[9]. Furthermore, this potent immunogenicity may lead to the loss of efficacy, hypersensitivity reactions, or infusion reactions[10].
Adalimumab (ADA) is the second biologic agent approved for use in the treatment of IBD. It is a subcutaneously administered, recombinant, fully human, IgG1 monoclonal antibody that binds with a high affinity and specificity to TNF-α and was found to be effective in refractory CD patients who were either naïve to or previously treated with IFX[11-15]. Combination therapy with IFX and an immunosuppressant demonstrated increased efficacy compared with nonconcomitant use of immunosuppressants[16,17]. Nonetheless, limited data are available for ADA. In the pivotal registration study of ADA (Crohn’s trial of the fully Human antibody ADA for Remission Maintenance, CHARM), post-hoc analysis did not detect an impact of coadministration of immunosuppressants on the remission rates achieved at 1 year[12]. Ardizzone et al[18] reported that ADA with concomitant immunosuppressant treatment was not associated with the loss of response or the need for dose escalation. However, Reenaers et al[19] reported that there may be a benefit from using immunosuppressive drugs during the first semester of initiating ADA treatment, with a slight decrease in ADA failure and lower need for ADA dosage escalation.
In Japan, ADA was approved for the treatment of CD; however, only limited data have been collected on its optimal usage. Therefore, this study aimed to assess the impact of ADA with concomitant azathioprine (AZA) therapy on the rate of clinical remission during maintenance with ADA in CD patients at the Osaka Medical College Hospital during routine clinical practice.
MATERIALS AND METHODS
Study participants
Between November 2010 and March 2012, about 28 CD patients who were diagnosed by clinical, endoscopic, and histological criteria and who received ADA at the Osaka Medical College Hospital, Osaka, Japan, were consecutively enrolled in this retrospective, observational, single-center study. The patients were informed about the potential risks and benefits of ADA therapy and were provided and signed informed consent forms before all procedures. The medical records of all participating patients were reviewed by two senior investigators (Ishida K and Inoue T) for the following information: demographics; disease duration; disease location; prior surgical history; perianal disease presence; smoking behavior; previous IFX treatment and response to IFX treatment; Crohn’s disease activity index (CDAI); C-reactive protein (CRP) levels; and concomitant medications (corticosteroids, AZA, mesalazine, and elemental diet).
All patients received 160 mg of ADA subcutaneously at week 0, 80 mg at week 2, followed by 40 mg every other week. A clinical response was defined as a ΔCDAI > 70 points, whereas a clinical remission was defined as a CDAI < 150 points. The loss of response to IFX was defined as a loss of therapeutic efficacy after > 2 IFX infusions.
Statistical analysis
Categorical data were compared by the χ2 test or the Fisher’s exact test, and continuous variables were compared by the Student t test. The results were expressed as the mean ± SD. P values less than 0.05 were considered to be statistically significant. All calculations were made using the StatView system (SAS Institute, Cary, NC, United States).
RESULTS
Patient characteristics
ADA was administered to 28 consecutive patients with CD from November 2011 to March 2012 at the Osaka Medical College Hospital (male-to-female ratio: 22/6; age at presentation: 38.1 ± 11.8 years; and disease duration: 11.8 ± 10.1 years). The patients’ baseline characteristics and demographics are listed in Table 1. According to the Montreal classification, patients presented with CD in the following locations: about 10.7% (3/28) in an isolated ileal location; 17.9% (5/28) in an isolated colonic location; and 71.4% (20/28) in an ileocolonic location. Of the patients, 60.7% (17/28) had a history of bowel resection, 57.1% had perianal disease, and 17.9% had an associated fistulizing disease. Two patients (7.1%) were current smokers.
Table 1.
Baseline characteristics of all patients who received adalimumab for treatment of Crohn’s disease n (%)
| Adalimumab | Combination | Total | |
| n = 16 | n = 12 | n = 28 | |
| Gender | |||
| Male | 13 (81.3) | 9 (75.0) | 22 (78.6) |
| Female | 3 (18.7) | 3 (25.0) | 6 (21.4) |
| Age at presentation1 (yr) | 43.1 ± 11.8 | 31.4 ± 8.3a | 38.1 ± 11.8 |
| Disease duration1 (yr) | 13.6 ± 11.5 | 9.3 ± 7.6 | 11.8 ± 10.1 |
| Location of disease | |||
| Isolated ileal | 2 (12.5) | 1 (8.3) | 3 (10.7) |
| Isolated colonic | 4 (25.0) | 1 (8.3) | 5 (17.9) |
| leocolonic | 10 (62.5) | 10 (83.3) | 20 (71.4) |
| Previous resection | 10 (62.5) | 7 (58.3) | 17 (60.7) |
| Perianal disease | 10 (62.5) | 6 (50) | 16 (57.1) |
| Current smokers | 1 (6.3) | 1 (8.3) | 2 (7.1) |
| Previous anti-infliximab treatment | 10 (62.5) | 7 (58.3) | 17 (60.7) |
| Primary nonresponse | 0 (0.0) | 1 (8.3) | 1 (3.6) |
| Secondary loss of response | 8 (50.0) | 6 (50.0) | 14 (50.0) |
| Allergic reaction | 1 (6.3) | 0 (0.0) | 1 (3.6) |
| Others | 1 (6.3) | 0 (0.0) | 1 (3.6) |
| CDAI at initiation of adalimumab therapy1 | 195.4 ± 89.2 | 152.2 ± 65.8 | 177.8 ± 82.0 |
| CDAI > 150 at initiation of adalimumab therapy, n | 9 | 7 | 16 |
| CRP at initiation of adalimumab therapy1 | 0.72 ± 0.92 | 0.66 ± 0.73 | 0.70 ± 0.83 |
Data are expressed as mean ± SD. CDAI: Crohn’s disease activity index.
P < 0.05 vs adalimumab.
Seventeen (60.7%) patients had previously taken IFX, and f patients did not have a response to IFX, including no primary response in one patient and emergent allergic reaction in another patient. Twelve of the 28 patients were treated with ADA and a concomitant stable dose of AZA throughout the observational period. The mean CDAI and mean CRP at baseline were 177.8 ± 82.0 and 0.70 ± 0.83 mg/dL, respectively.
Clinical efficacy of ADA therapy
The overall clinical response and remission rates are shown in Table 2. The rates of clinical remission at weeks 2, 4, 8, and 24 were 60%, 66.7%, 69.6%, and 63.2%, respectively. The mean CDAI of all patients at weeks 2, 4, 8, and 24 was 124.4 ± 60.2, 120.0 ± 66.8, 123.6 ± 73.5, and 135.1 ± 74.4, respectively. The CDAI was significantly decreased commencing 2 wk after the initiation of ADA treatment and remained low for 24 wk (Table 2).
Table 2.
Clinical efficacy of adalimumab therapy
| Week | 0 | 2 | 4 | 8 | 24 |
| n | 27 | 25 | 24 | 23 | 19 |
| CDAI | 177.8 ± 82.0 | 124.4 ± 60.2a | 120.0 ± 66.8a | 123.6 ± 73.5a | 135.1 ± 74.4a |
| Remission | 37% | 60% | 66.70% | 69.60% | 63.20% |
Remission: Crohn’s disease activity index (CDAI ) < 150 points.
P < 0.05 vs week 0.
Impact of ADA/AZA on the clinical remission compared to ADA maintenance
Regarding the concomitant use of immunosuppressive agents, 12 patients (42.9%) were treated with a stable dose of AZA (50.0 ± 21.3 mg/d, 1.0 ± 0.5 mg/kg/d) before the initiation of ADA. The concomitant use of AZA was well tolerated, with only minor side effects. Although there were no statistically significant differences seen until 12 wk into ADA and AZA treatment (compared with ADA treatment), combinational therapy with ADA and AZA significantly increased the clinical remission rate (Figure 1) and reduced the CDAI, compared with nonconcomitant use at week 24 (Figure 2A).
Figure 1.
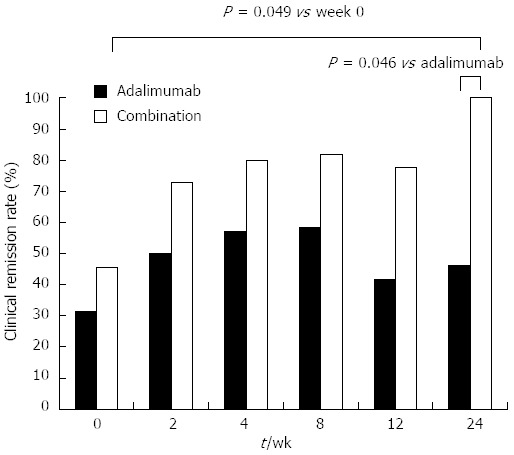
Clinical remission rate. Combinational therapy with adalimumab and azathioprine significantly increased the clinical remission rate vs nonconcomitant use at week 24.
Figure 2.
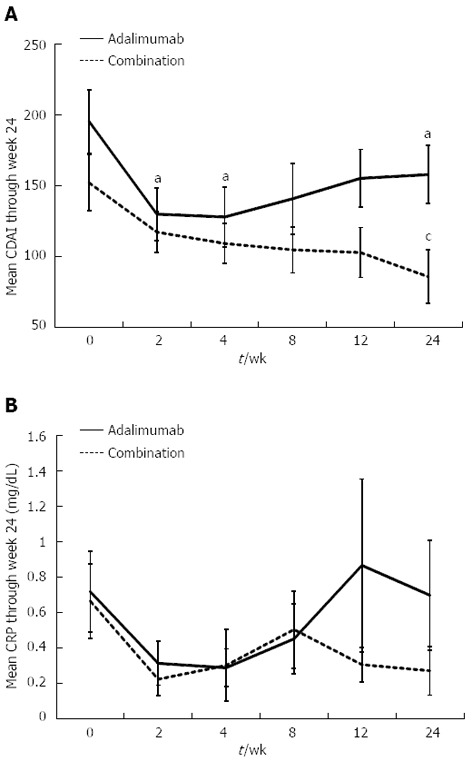
Mean Crohn’s disease activity index and C-reactive protein through week 24. A: Combinational therapy with adalimumab (ADA) and azathioprine (AZA) significantly reduced the Crohn’s disease activity index (CDAI), compared with nonconcomitant use at week 24. aP < 0.05 vs week 0; cP < 0.05 vs adalimumab; B: The concomitant use of AZA tended to maintain low C-reactive protein (CRP) levels for 24 wk (CRP levels at weeks 0 and 24 were 0.66 ± 0.73 and 0.27 ± 0.44, respectively, P = 0.09).
Sixteen of the 28 patients were found to have increased CRP serum levels (> 0.25 mg/dL) before starting ADA therapy. The mean serum CRP of all of the patients at weeks 2, 4, 8, and 24 were 0.27 ± 0.40, 0.28 ± 0.51, 0.46 ± 0.69, and 0.51 ± 0.94 mg/dL, respectively. ADA significantly reduced the CRP levels at weeks 2 and 4 after the initiation of treatment. The concomitant use of AZA tended to maintain low CRP levels for 24 wk, even though the result was not statistically significant (CRP levels at weeks 0 and 24 were 0.66 ± 0.73 and 0.27 ± 0.44 mg/dL, respectively; P = 0.09, Figure 2B).
DISCUSSION
The effectiveness of AZA in CD patients treated with IFX has been clearly reported by many investigators. However, few reports have demonstrated the benefits of ADA and AZA combination therapy. In this study, we analyzed the use of ADA and AZA in patients with mild to moderate CD at our clinical practice and found that scheduled ADA with concomitant use of AZA was more effective in inducing and maintaining remission for 24 wk after the initiation of ADA treatment, compared with ADA monotherapy. Although ADA monotherapy was also able to induce and maintain clinical remission from 2 to 24 wk compared to the baseline, the effects of the combination therapy were better. Since previous IFX nonresponse and previous treatment with an anti-TNF agent were reported to be associated with a decreased clinical efficacy and a loss of response[20], we also compared the CDAI between anti-TNF-naïve patients and anti-TNF-treated patients in this study, but there was no significant difference.
ADA is a human monoclonal IgG1 antibody that has demonstrated efficacy in the induction and maintenance of clinical remission in patients with moderate to severe CD and is useful in patients who have lost responsiveness to IFX[11-15]. IFX, a chimeric anti-TNF-α antibody, has potent immunogenicity; repeated administration of IFX could result in the development of antibodies that may lead to the loss of response[21]. Although no consensus has yet been established on the appropriateness of concomitant immunomodulators with anti-TNF-α antibody therapy for CD[22-24], immunosuppressants were shown to inhibit the development of HACA[10]. Moreover, since the clearance of IFX is affected by the presence of HACA, IFX serum levels were significantly higher in patients with concomitant immunosuppressive therapy, as this concomitant usage reduces the frequency of HACA formation[4,25]. Sokol et al[17] assessed the efficacy of immunosuppressants with scheduled IFX in patients with IBD and reported that IBD flare-ups, perianal complications, and switching to ADA were less frequently observed in patients with combined immunosuppressant and biologic agent use than in those patients who were not concomitantly treated with immunosuppressants[22]. Furthermore, in the SONIC study, Colombel et al[16] compared the efficacy and safety of IFX monotherapy and IFX plus AZA combination therapy for CD and showed that the combination therapy provided a significantly greater benefit than that of IFX monotherapy at weeks 26 and 50. These studies suggest that combination therapy with IFX and AZA may have an added benefit in maintaining the remission of CD. With regard to ADA, a substantial proportion of patients, including previously treated anti-TNF-α patients and anti-TNF-α treatment-naïve patients, needed dose escalation during ADA treatment[12,26]. However, concomitant immunosuppressive therapy was not associated with a loss of response or a need for dose escalation and did not influence the development of ADA antibodies[27-29]. Recently, Reenaers et al[19] reported that usage of ADA with immunosuppressive drugs, such as AZA, during the first semester of initiating ADA demonstrated a slight decrease in ADA failure and a lower need for ADA dose escalation. Moreover, the presence of anti-ADA antibodies and a low serum ADA concentration have been reported to be associated with a diminished clinical response in rheumatoid arthritis patients, and the concomitant use of an immunomodulator significantly suppresses the concentration of anti-ADA antibodies[30,31]. Interestingly, in this study, AZA in the presence of ADA provides better efficacy in patients it has previously failed. However, some patients with IFX had not early received concomitant AZA. Therefore, we consider that ADA and AZA combination therapy may be more effective than ADA monotherapy via the inhibition of the development of anti-ADA antibodies. Prospective studies, combined with anti-ADA antibody and ADA trough level measurements, are required[19].
In this study, we found that ADA treatment with concomitant AZA usage significantly suppressed the CDAI and increased the remission rate at 24 weeks after the initiation of therapy, compared with ADA treatment alone. Furthermore, these results were not consistent with previous reports showing that the efficacy of ADA is independent of the use of concomitant immunosuppression[27-29]. One possible explanation for this discrepancy is that these previous studies assessed the efficacy of ADA in patients with moderate to severe CD, whereas the present study included mild to moderate CD patients. Notably, the CDAI at the beginning of this study was relatively low (177.8 ± 82.0). Since the CDAI scores were gradually increasing, some patients were switched from IFX treatment to ADA treatment, even though their CDAI scores were still in remission (CDAI < 150 at the initiation of ADA treatment). Indeed, Zheng et al[32] evaluated the efficacy of AZA in controlling the relapse of disease in patients with CD for at least 6 months and showed that AZA treatment decreased the CDAI from 187.3 ± 23.4 to 96.1 ± 13.5. Actually, the finding of a significant efficacy with ADA plus AZA combination therapy compared to ADA monotherapy is revealed only after week 24 in this study. Generally, thiopurines require a lag time of approximately 6 mo before expressing full activity. Taken together, we consider that the combination of ADA and AZA may have an added benefit in inducing long-term remission compared with ADA alone, even though ADA has shown less immunogenicity compared with IFX.
Our study had some major limitations. The patients were not randomized between ADA monotherapy and ADA plus AZA combination therapy. Also, the mean age was significantly different between these two groups due to the nature of retrospective study. Therefore, these two groups were not strictly comparable. In addition, the patient numbers were limited, as we only analyzed the data in our own hospital. Moreover, recent studies have revealed that Japanese and Caucasian CD patients genetically differ, as Japanese CD patients lack the polymorphism in the NOD2 gene[33-36]. Genetic differences might have affected the results in this study. An additional, larger, long-term multicenter study should be conducted to determine the effect of combination therapy with ADA and AZA for patients with CD.
So far, there have been few reports demonstrating that CD patients could achieve a better clinical remission with ADA and immunomodulator combination therapy, compared with ADA monotherapy[19,37]. This study may help physicians decide whether to use combination therapy. In conclusion, scheduled ADA with concomitant AZA is more effective for clinical remission achievement at 24 wk in Japanese CD patients. Although further long-term studies evaluating the efficacy of combination therapy with ADA and AZA are required, our data suggest that ADA with concomitant AZA therapy may provide clinical benefit in inducing long-term remission.
COMMENTS
Background
The benefits of azathioprine (AZA) in Crohn’s disease (CD) with infliximab as scheduled anti-tumor necrosis factor-α maintenance therapy have been established but remain unclear with adalimumab (ADA).
Research frontiers
So far, there have been few reports demonstrating that CD patients could achieve better clinical remission with ADA and immunomodulator combination therapy, compared with ADA monotherapy.
Innovations and breakthroughs
This is the first study reported in Asia on the effect of ADA with concomitant AZA for induction and maintenance of clinical remission in CD patients. The results of this study showed that ADA treatment with concomitant AZA usage significantly suppressed the Crohn’s disease activity index and increased the remission rate at 24 wk after the initiation of therapy, compared with ADA treatment alone.
Applications
Although further long-term studies evaluating the efficacy of combination therapy with ADA and AZA are required, this study suggests that ADA with concomitant AZA therapy may provide clinical benefit in inducing long-term remission. The results of this study may help physicians decide whether to use combination therapy.
Peer review
This is an interesting small retrospective, observational, study assessing the effect of effects of ADA treatment with concomitant AZA in CD patients.
Footnotes
P- Reviewers Actis GC, de Boer NKH, Chermesh I S- Editor Gou SX L- Editor A E- Editor Zhang DN
References
- 1.Van Deventer SJ. Tumour necrosis factor and Crohn's disease. Gut. 1997;40:443–448. doi: 10.1136/gut.40.4.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Podolsky DK. Inflammatory bowel disease. N Engl J Med. 2002;347:417–429. doi: 10.1056/NEJMra020831. [DOI] [PubMed] [Google Scholar]
- 3.Reimund JM, Wittersheim C, Dumont S, Muller CD, Kenney JS, Baumann R, Poindron P, Duclos B. Increased production of tumour necrosis factor-alpha interleukin-1 beta, and interleukin-6 by morphologically normal intestinal biopsies from patients with Crohn's disease. Gut. 1996;39:684–689. doi: 10.1136/gut.39.5.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sandborn WJ, Targan SR. Biologic therapy of inflammatory bowel disease. Gastroenterology. 2002;122:1592–1608. doi: 10.1053/gast.2002.33426. [DOI] [PubMed] [Google Scholar]
- 5.Targan SR, Hanauer SB, van Deventer SJ, Mayer L, Present DH, Braakman T, DeWoody KL, Schaible TF, Rutgeerts PJ. A short-term study of chimeric monoclonal antibody cA2 to tumor necrosis factor alpha for Crohn's disease. Crohn's Disease cA2 Study Group. N Engl J Med. 1997;337:1029–1035. doi: 10.1056/NEJM199710093371502. [DOI] [PubMed] [Google Scholar]
- 6.Hanauer SB, Feagan BG, Lichtenstein GR, Mayer LF, Schreiber S, Colombel JF, Rachmilewitz D, Wolf DC, Olson A, Bao W, et al. Maintenance infliximab for Crohn's disease: the ACCENT I randomised trial. Lancet. 2002;359:1541–1549. doi: 10.1016/S0140-6736(02)08512-4. [DOI] [PubMed] [Google Scholar]
- 7.Present DH, Rutgeerts P, Targan S, Hanauer SB, Mayer L, van Hogezand RA, Podolsky DK, Sands BE, Braakman T, DeWoody KL, et al. Infliximab for the treatment of fistulas in patients with Crohn's disease. N Engl J Med. 1999;340:1398–1405. doi: 10.1056/NEJM199905063401804. [DOI] [PubMed] [Google Scholar]
- 8.Sands BE, Anderson FH, Bernstein CN, Chey WY, Feagan BG, Fedorak RN, Kamm MA, Korzenik JR, Lashner BA, Onken JE, et al. Infliximab maintenance therapy for fistulizing Crohn's disease. N Engl J Med. 2004;350:876–885. doi: 10.1056/NEJMoa030815. [DOI] [PubMed] [Google Scholar]
- 9.Hanauer SB, Wagner CL, Bala M, Mayer L, Travers S, Diamond RH, Olson A, Bao W, Rutgeerts P. Incidence and importance of antibody responses to infliximab after maintenance or episodic treatment in Crohn's disease. Clin Gastroenterol Hepatol. 2004;2:542–553. doi: 10.1016/s1542-3565(04)00238-1. [DOI] [PubMed] [Google Scholar]
- 10.Baert F, Noman M, Vermeire S, Van Assche G, D' Haens G, Carbonez A, Rutgeerts P. Influence of immunogenicity on the long-term efficacy of infliximab in Crohn's disease. N Engl J Med. 2003;348:601–608. doi: 10.1056/NEJMoa020888. [DOI] [PubMed] [Google Scholar]
- 11.Hanauer SB, Sandborn WJ, Rutgeerts P, Fedorak RN, Lukas M, MacIntosh D, Panaccione R, Wolf D, Pollack P. Human anti-tumor necrosis factor monoclonal antibody (adalimumab) in Crohn's disease: the CLASSIC-I trial. Gastroenterology. 2006;130:323–33; quiz 591. doi: 10.1053/j.gastro.2005.11.030. [DOI] [PubMed] [Google Scholar]
- 12.Colombel JF, Sandborn WJ, Rutgeerts P, Enns R, Hanauer SB, Panaccione R, Schreiber S, Byczkowski D, Li J, Kent JD, et al. Adalimumab for maintenance of clinical response and remission in patients with Crohn's disease: the CHARM trial. Gastroenterology. 2007;132:52–65. doi: 10.1053/j.gastro.2006.11.041. [DOI] [PubMed] [Google Scholar]
- 13.Hinojosa J, Gomollón F, García S, Bastida G, Cabriada JL, Saro C, Ceballos D, Peñate M, Gassull MA. Efficacy and safety of short-term adalimumab treatment in patients with active Crohn's disease who lost response or showed intolerance to infliximab: a prospective, open-label, multicentre trial. Aliment Pharmacol Ther. 2007;25:409–418. doi: 10.1111/j.1365-2036.2006.03232.x. [DOI] [PubMed] [Google Scholar]
- 14.Sandborn WJ, Hanauer S, Loftus EV, Tremaine WJ, Kane S, Cohen R, Hanson K, Johnson T, Schmitt D, Jeche R. An open-label study of the human anti-TNF monoclonal antibody adalimumab in subjects with prior loss of response or intolerance to infliximab for Crohn's disease. Am J Gastroenterol. 2004;99:1984–1989. doi: 10.1111/j.1572-0241.2004.40462.x. [DOI] [PubMed] [Google Scholar]
- 15.Seiderer J, Brand S, Dambacher J, Pfennig S, Jürgens M, Göke B, Ochsenkühn T. Adalimumab in patients with Crohn's disease--safety and efficacy in an open-label single centre study. Aliment Pharmacol Ther. 2007;25:787–796. doi: 10.1111/j.1365-2036.2007.03253.x. [DOI] [PubMed] [Google Scholar]
- 16.Colombel JF, Sandborn WJ, Reinisch W, Mantzaris GJ, Kornbluth A, Rachmilewitz D, Lichtiger S, D'Haens G, Diamond RH, Broussard DL, et al. Infliximab, azathioprine, or combination therapy for Crohn's disease. N Engl J Med. 2010;362:1383–1395. doi: 10.1056/NEJMoa0904492. [DOI] [PubMed] [Google Scholar]
- 17.Sokol H, Seksik P, Carrat F, Nion-Larmurier I, Vienne A, Beaugerie L, Cosnes J. Usefulness of co-treatment with immunomodulators in patients with inflammatory bowel disease treated with scheduled infliximab maintenance therapy. Gut. 2010;59:1363–1368. doi: 10.1136/gut.2010.212712. [DOI] [PubMed] [Google Scholar]
- 18.Ardizzone S, Cassinotti A, Manes G, Porro GB. Immunomodulators for all patients with inflammatory bowel disease? Therap Adv Gastroenterol. 2010;3:31–42. doi: 10.1177/1756283X09354136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reenaers C, Louis E, Belaiche J, Seidel L, Keshav S, Travis S. Does co-treatment with immunosuppressors improve outcome in patients with Crohn's disease treated with adalimumab? Aliment Pharmacol Ther. 2012;36:1040–1048. doi: 10.1111/apt.12076. [DOI] [PubMed] [Google Scholar]
- 20.Kiss LS, Szamosi T, Molnar T, Miheller P, Lakatos L, Vincze A, Palatka K, Barta Z, Gasztonyi B, Salamon A, et al. Early clinical remission and normalisation of CRP are the strongest predictors of efficacy, mucosal healing and dose escalation during the first year of adalimumab therapy in Crohn's disease. Aliment Pharmacol Ther. 2011;34:911–922. doi: 10.1111/j.1365-2036.2011.04827.x. [DOI] [PubMed] [Google Scholar]
- 21.Cassinotti A, Travis S. Incidence and clinical significance of immunogenicity to infliximab in Crohn's disease: a critical systematic review. Inflamm Bowel Dis. 2009;15:1264–1275. doi: 10.1002/ibd.20899. [DOI] [PubMed] [Google Scholar]
- 22.Lakatos PL, Kiss LS. Current status of thiopurine analogues in the treatment in Crohn's disease. World J Gastroenterol. 2011;17:4372–4381. doi: 10.3748/wjg.v17.i39.4372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lichtenstein GR, Diamond RH, Wagner CL, Fasanmade AA, Olson AD, Marano CW, Johanns J, Lang Y, Sandborn WJ. Clinical trial: benefits and risks of immunomodulators and maintenance infliximab for IBD-subgroup analyses across four randomized trials. Aliment Pharmacol Ther. 2009;30:210–226. doi: 10.1111/j.1365-2036.2009.04027.x. [DOI] [PubMed] [Google Scholar]
- 24.Sandborn WJ, Feagan BG, Stoinov S, Honiball PJ, Rutgeerts P, Mason D, Bloomfield R, Schreiber S. Certolizumab pegol for the treatment of Crohn's disease. N Engl J Med. 2007;357:228–238. doi: 10.1056/NEJMoa067594. [DOI] [PubMed] [Google Scholar]
- 25.Vermeire S, Noman M, Van Assche G, Baert F, D'Haens G, Rutgeerts P. Effectiveness of concomitant immunosuppressive therapy in suppressing the formation of antibodies to infliximab in Crohn's disease. Gut. 2007;56:1226–1231. doi: 10.1136/gut.2006.099978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bultman E, de Haar C, van Liere-Baron A, Verhoog H, West RL, Kuipers EJ, Zelinkova Z, van der Woude CJ. Predictors of dose escalation of adalimumab in a prospective cohort of Crohn's disease patients. Aliment Pharmacol Ther. 2012;35:335–341. doi: 10.1111/j.1365-2036.2011.04946.x. [DOI] [PubMed] [Google Scholar]
- 27.Billioud V, Sandborn WJ, Peyrin-Biroulet L. Loss of response and need for adalimumab dose intensification in Crohn's disease: a systematic review. Am J Gastroenterol. 2011;106:674–684. doi: 10.1038/ajg.2011.60. [DOI] [PubMed] [Google Scholar]
- 28.Karmiris K, Paintaud G, Noman M, Magdelaine-Beuzelin C, Ferrante M, Degenne D, Claes K, Coopman T, Van Schuerbeek N, Van Assche G, et al. Influence of trough serum levels and immunogenicity on long-term outcome of adalimumab therapy in Crohn's disease. Gastroenterology. 2009;137:1628–1640. doi: 10.1053/j.gastro.2009.07.062. [DOI] [PubMed] [Google Scholar]
- 29.West RL, Zelinkova Z, Wolbink GJ, Kuipers EJ, Stokkers PC, van der Woude CJ. Immunogenicity negatively influences the outcome of adalimumab treatment in Crohn's disease. Aliment Pharmacol Ther. 2008;28:1122–1126. doi: 10.1111/j.1365-2036.2008.03828.x. [DOI] [PubMed] [Google Scholar]
- 30.Bartelds GM, Wijbrandts CA, Nurmohamed MT, Stapel S, Lems WF, Aarden L, Dijkmans BA, Tak PP, Wolbink GJ. Clinical response to adalimumab: relationship to anti-adalimumab antibodies and serum adalimumab concentrations in rheumatoid arthritis. Ann Rheum Dis. 2007;66:921–926. doi: 10.1136/ard.2006.065615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bartelds GM, Krieckaert CL, Nurmohamed MT, van Schouwenburg PA, Lems WF, Twisk JW, Dijkmans BA, Aarden L, Wolbink GJ. Development of antidrug antibodies against adalimumab and association with disease activity and treatment failure during long-term follow-up. JAMA. 2011;305:1460–1468. doi: 10.1001/jama.2011.406. [DOI] [PubMed] [Google Scholar]
- 32.Zheng JJ, Chu XQ, Shi XH, Zhou CL, Seng BW. Efficacy and safety of azathioprine maintenance therapy in a group of Crohn's disease patients in China. J Dig Dis. 2008;9:84–88. doi: 10.1111/j.1751-2980.2008.00327.x. [DOI] [PubMed] [Google Scholar]
- 33.Tanabe T, Yamaguchi N, Matsuda K, Yamazaki K, Takahashi S, Tojo A, Onizuka M, Eishi Y, Akiyama H, Ishikawa J, et al. Association analysis of the NOD2 gene with susceptibility to graft-versus-host disease in a Japanese population. Int J Hematol. 2011;93:771–778. doi: 10.1007/s12185-011-0860-5. [DOI] [PubMed] [Google Scholar]
- 34.Ahuja V, Tandon RK. Inflammatory bowel disease in the Asia-Pacific area: a comparison with developed countries and regional differences. J Dig Dis. 2010;11:134–147. doi: 10.1111/j.1751-2980.2010.00429.x. [DOI] [PubMed] [Google Scholar]
- 35.Zheng CQ, Hu GZ, Zeng ZS, Lin LJ, Gu GG. Progress in searching for susceptibility gene for inflammatory bowel disease by positional cloning. World J Gastroenterol. 2003;9:1646–1656. doi: 10.3748/wjg.v9.i8.1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sugimura M, Kinouchi Y, Takahashi S, Aihara H, Takagi S, Negoro K, Obana N, Kojima Y, Matsumoto K, Kikuchi T, et al. CARD15/NOD2 mutational analysis in Japanese patients with Crohn's disease. Clin Genet. 2003;63:160–162. doi: 10.1046/j.0009-9163.2002.00174.x. [DOI] [PubMed] [Google Scholar]
- 37.Martín-de-Carpi J, Pociello N, Varea V. Long-term efficacy of adalimumab in paediatric Crohn's disease patients naïve to other anti-TNF therapies. J Crohns Colitis. 2010;4:594–598. doi: 10.1016/j.crohns.2010.04.002. [DOI] [PubMed] [Google Scholar]


