Abstract
Cranial meningoceles/encephaloceles are congenital malformations characterised by protrusion of the meninges and/or brain parenchyma because of a skull defect. Meningoceles secondary to an intracranial neoplasm have not been reported in the published literature. We report a unique case of a 42-year-old man who presented with a sudden onset of altered sensorium. Transethmoidal meningocele secondary to an intraventricular epidermoid cyst was detected on imaging.
Background
A skull defect in association with herniated intracranial content is termed as cephalocele. If the herniation contains solely leptomeninges and cerebrospinal fluid (CSF), it is termed as meningocele. These are usually of developmental origin. Raised intracranial tension (ICT) may cause erosion of the skull base and may result in CSF leak. Nevertheless, the formation of secondary meningocele has not been reported in the published literature. We are reporting a case of intraventricular epidermoid cyst, a rare entity leading to a gradual increase in ICT with the development of secondary transethmoidal meningocele.
Case presentation
A 42-year-old male patient, who had a history of gradually progressive diminution of vision for 15 years, presented with a sudden onset of altered sensorium. Glasgow Coma Scale score was E3V4M6. Perception of light was absent in both eyes and fundoscopy revealed bilateral optic atrophy. No evidence of orbital or ocular inflammation was present.
Investigations
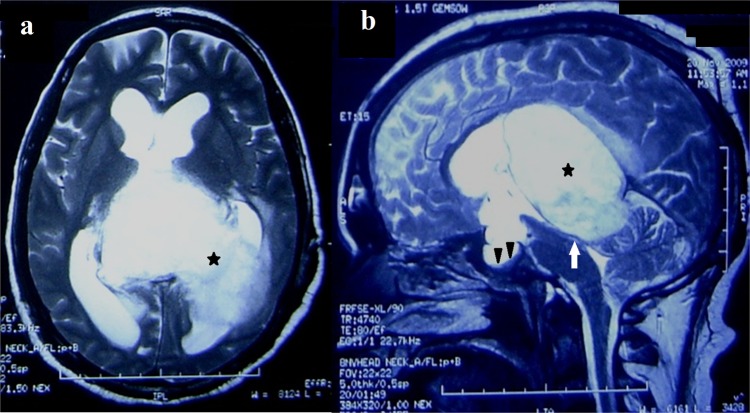
On CT, a large, non-enhancing space-occupying hypodense lesion of near CSF attenuation was noted filling the atrium and occipital horn of the left lateral ventricle (figure 1A). The lesion was causing expansion of the overlying lateral ventricle and compression over the posterior part of the third ventricle leading to obstructive hydrocephalus. Effacement of the extraventricular CSF space was noted owing to the dilated ventricular system. Based on the above findings, differential diagnosis of epidermoid and arachnoid cysts was performed. Another interesting finding was herniation of the CSF containing a sac into the nasal cavity through a defect in the cribriform plate consistent with transethmoidal meningocele (figure 1B).
Figure 1.
CT sagittal (A) and coronal (B) image showing herniation of meninges in the nasal cavity through the defect in the cribriform plate (arrow). A large hypodense lesion of near cerebrospinal fluid attenuation is also noted in the sagittal image (star).
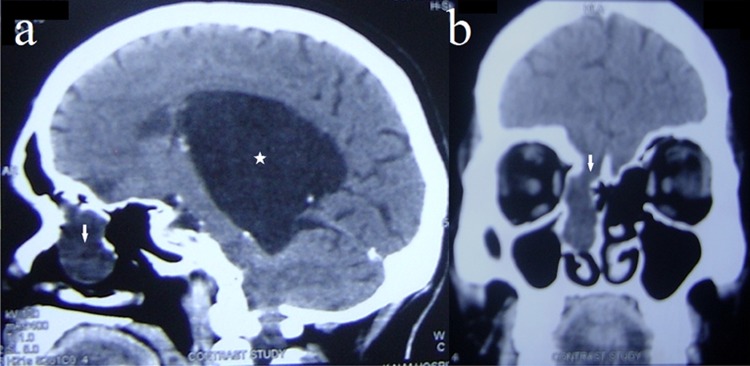
To determine the nature and extent of intraventricular mass lesion, MRI was performed which revealed an expansile mass lesion occupying the atrium and occipital horn of the left lateral ventricle (figure 2). The lesion was displaying signal intensities, isointense to CSF on T1, T2 and T2 fluid-attenuated inversion recovery with restriction on diffusion weighted images diagnostic of intraventricular epidermoid cyst. Compression of the aqueduct and posterior third ventricle was also noted with dilation of its infundibular recess causing compression of the pituitary gland and ballooning of sella (figure 2B). Pressure atrophy of brain parenchyma owing to the obstructive hydrocephalus was also demonstrated. Defect in the cribriform plate with herniation of meninges and CSF was noted without any parenchymal component diagnostic of transethmoidal meningocele (figure 3).
Figure 2.
T2-weighted axial and sagittal MR image shows a large hyperintense lesion in the atrium and occipital horn of the left lateral ventricle (star). Compression of the aqueduct and posterior third ventricle (arrow) is evident with dilation of the proximal part of the third and bilateral lateral ventricles. Enlarged sella and compressed pituitary gland is also seen (arrow heads).
Figure 3.
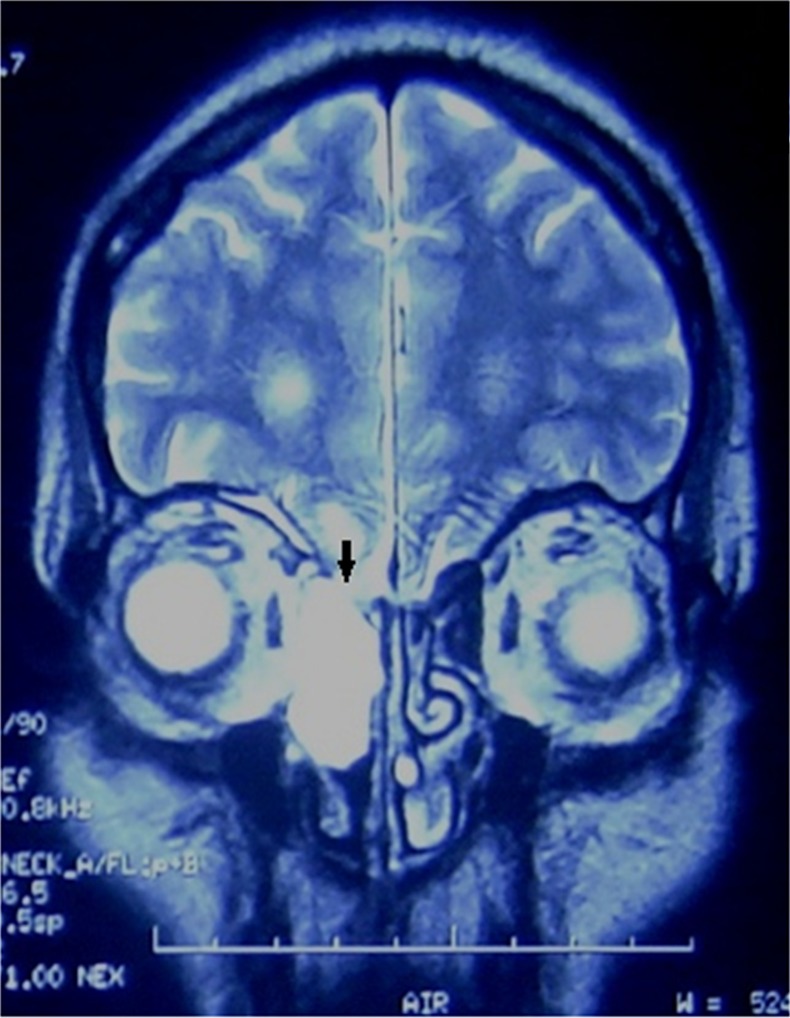
T2-weighted coronal MRI shows defect in the cribriform plate with herniation of cerebrospinal fluid containing the sac (arrow).
Treatment
Patient was operated under general anaesthesia. Transcortical-transventricular excision of intraventricular tumour was performed. Histopathology was consistent with epidermoid tumour. Since meningocele was asymptomatic, it was not operated upon. Postoperative period was uneventful and the patient was discharged on the 15th postoperative day with improved neurological status.
Discussion
Encephalocele refers to the developmental malformations, characterised by the herniation of neural tissue through a defect in skull.1 These may be characterised by the presence of merely meninges (meningocele), meninges with brain parenchyma (encephalomeningocele) or their communication with a ventricle (encephalomeningocystocele).2 Secondary development of meningocele as a consequence of raised ICT has rarely been reported in the published literature.
Elevated intracranial pressure secondary to tumours or hydrocephalus leads to progressive erosion and weakening of bone with the eventual development of a fracture and a CSF fistula resulting in CSF leak.3 4 Areas of CSF leakage correspond to the sites of congenital weakness in the cribriform plate, roof of ethmoid, parasellar region or the temporal bone.5 One very interesting fact is that dura mater is much more resistant as compared to the bones for raised ICT and there have been case reports in which the overlying bone has been entirely destroyed and the dura, although pushed through the hole formed in the skull, is still intact.6 These facts explain the formation of meningocele in our case. Another important fact that has to be kept in mind is that the cause of raised ICT in our case was an intraventricular epidermoid cyst, which is a slow growing tumour. Had it been an aggressive tumour, it would have caused rapid increase in the ICT and early presentation of the patient. Other features, also developed as a result of chronically raised ICT and demonstrated on imaging, were widening of sella, erosion of posterior clinoid processes and pressure atrophy of brain parenchyma. Endoscopic repair of the CSF fistula is the gold standard treatment for this condition, but emerging evidence supports the reduction of CSF pressure as an important adjuvant treatment in this type of patient population.7 8 Long-term follow-up appears mandatory in our case to look for the recurrence of epidermoid and to know the fate of the meningocele.
Learning points.
Cerebrospinal fluid (CSF) rhinorrhoea may be a secondary manifestation of the chronically raised intracranial tension (ICT).
CSF rhinorrhoea/meningocele, in these cases, usually respond well to the treatment of raised ICT.
Long-term follow-up is mandatory as ascending meningitis may be a life-threatening complication.
Footnotes
Contributors: DKS is the clinician involved in the management. DKS has prepared the manuscript under the supervision of RS with regards to NS.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Barkovich AJ, Chuang SH, Norman D. MR of neuronal migration anomalies. AJNR Am J Neuroradiol 1987;2013:1009–17 [Google Scholar]
- 2.Barkovich AJ, Kjos BO. Schizencephaly: correlation of clinical findings with MR characteristics. AJNR Am J Neuroradiol 1992;2013:85–94 [PMC free article] [PubMed] [Google Scholar]
- 3.Park JI, Strelzow VV, Friedman WH. Current management of cerebrospinal fluid rhinorrhea. Laryngoscope 1983;2013:1294–300 [DOI] [PubMed] [Google Scholar]
- 4.Vaezi A, Snyderman CH, Saleh HA, et al. Pseudomeningoceles of the sphenoid sinus masquerading as sinus pathology. Laryngoscope 2011;2013:2507–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Briant TD, Bird R. Extracranial repair of cerebrospinal fluid fistulae. J Otolaryngol 1982;2013:191–7 [PubMed] [Google Scholar]
- 6.Jupe MH. The reaction of the bones of the skull to intracranial lesions. Br J Radiol 1938;2013:146–64 [Google Scholar]
- 7.Wang EW, Vandergrift WA, III, Schlosser RJ. Spontaneous CSF leaks. Otolaryngol Clin North Am 2011;2013:845–56 [DOI] [PubMed] [Google Scholar]
- 8.Bryson E, Draf W, Hofmann E, et al. Management of occult malformations at the lateral skull base. Laryngorhinootologie 2005;2013:921–8 [DOI] [PubMed] [Google Scholar]