Abstract
Juvenile ossifying fibroma (JOF) is a rare fibro-osseous neoplasm that arises within the craniofacial bones in individuals under 15 years of age, and these lesions are usually benign and tend to grow slowly. The psammomatous type of juvenile ossifying fibroma (PsJOF) mainly involves the bones of the orbit and paranasal sinuses, whereas the trabecular type commonly involves the jaws. We are presenting a case of PsJOF of ramus of mandible in a 7-years-old boy, which is an uncommon condition, and histologically showed predominantly a cellular connective tissue stroma, composed of numerous spindle-shaped cells arranged in fascicular storiform pattern. In between these irregular strands of trabeculae with plump osteoblast, spheroidal ossicles with basophilic in center and eosinophilic in periphery resembling psammoma-like bodies are noticed.
Keywords: Fibro-osseous lesions, mandible, psammomatoid type
INTRODUCTION
Juvenile ossifying fibroma (JOF) appears at an early age and in a majority of the patients, is diagnosed in the first or second decade of life. It originates from periodontal ligament. It constitutes 2% of all oral tumours in children. It has an equal predilection for males and females. JOF commonly occurs in the facial bones (85%), calvarium (12%) and mandibular region (10%). Very rarely it has been reported extracranially (3%).[1] These lesions are variously called as young ossifying fibroma, juvenile aggressive or active ossifying fibroma, and trabecular desmo-osteoblastoma and are unencapsulated but well demarcated from the surrounding bone, and this finding can help in differentiating it from fibrous dysplasia.[2] JOF is a rare fibro-osseous neoplasm and usually benign and tend to grow slowly. The age predilection for psammomatous type JOF is less than 21.8 years. This lesion has clinically more aggressive growth rate than ossifying fibroma and has strong tendency to recur. They are mostly found in extragnathic bones; however, in some cases, maxilla or, rarely, the mandible may be affected.[3] The psammomatous juvenile ossifying fibroma (PsJOF) mainly involves the bones of the orbit and paranasal sinuses, whereas the trabecular type commonly involves the jaws.[4] Computed tomography imaging plays a major role in detecting the extent of such lesions, their diagnosis, and planning the management.[5] The PsJOF are unique lesions that occur commonly in children. Psammoma-like bodies are the hallmark of this neoplasm. Mandibular lesions are uncommon and can be mistaken for an odontogenic cyst. Clinical, radiographic, and histopathological correlation will be beneficial in arriving at the accurate diagnosis.[6] Here, we report an additional case of PsJOF that occurred in the mandible, an uncommon site.
CASE REPORT
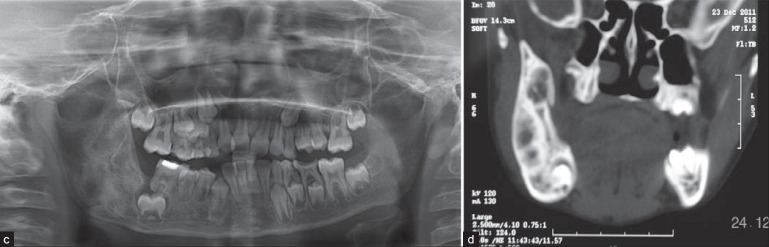
A 7-year-old boy reported to our unit with the complaint of swelling of the face at right posterior region of the mandible and asymmetry of face since 1 year. Patient's parents presented history of extra-oral swelling since 3 years; initially, swelling appeared small in size and reached to present size with asymptomatic. Extra-oral examination revealed a 3 × 3 cm swelling on the right posterior of the mandible, extending from posterior to the corner of the mouth over the ramus and angle of the mandible [Figure 1a]. The swelling appeared bony hard in consistency on palpation and no discharge of pus, paresthesia of the lip or restricted mouth opening. Intraorally, mucosa over swelling appearing in normal color, hard in consistency with expanded cortical plate and also noticed altered vestibular region. Anterioposteriorly, the swelling was extending from permanent first molar to retromolar area and involving the part of ramus region as well. Superioinferiorly, the swelling was extending from retromolar region towards the angle and inferior border of mandible [Figure 1b]. Routine radiographs like panoramic, AP and lateral views of skull showed large radioluceny and well-defined sclerotic border along with radiopacity observed in the center of the lesion (mixed lesion) with inferior border intact. The lesion extending from distal to first molar and 1 cm away from the posterior border of ramus of mandible anterioposteriorly. Superioinferiorly, the lesion extending from sigmoid notch towards the inferior border short about 0.5 cm. The panoramic view showed erupted first molar and the second molar, displaced inferiorly and anteriorly, lying below the apex of first molar [Figure 1c]. Computed tomography revealed mixed radioluceny and radiodensity and well-defined osteolytic mass involving the right posterior region of the mandible [Figure 1d]. Routine blood investigation revealed normal study. Aspiration and biopsy was performed to rule out arteriovenous malformations, cystic lesions, and the fibro-osseous lesions. On aspiration, nothing was revealed and biopsy was done. Histopathology report confirmed psammomatoid type of juvenile ossifying fibroma. Considering the factors like intact inferior border, no involvement of adjacent structures, no paresthesia of lip, and age of the patient, this case was planned primarily for excision and curettage without resection [Figure 2a and b]. Postoperative regular follow-up for 3 years has been done; facial and intra-oral photographs showed normal study [Figure 3a and b]. Panoramic and computed tomography showed osseous regeneration and normal bone pattern [Figure 3c and d]. Regular follow-up has been done since then and there is no evidence of recurrence so far.
Figure 1(a,b).
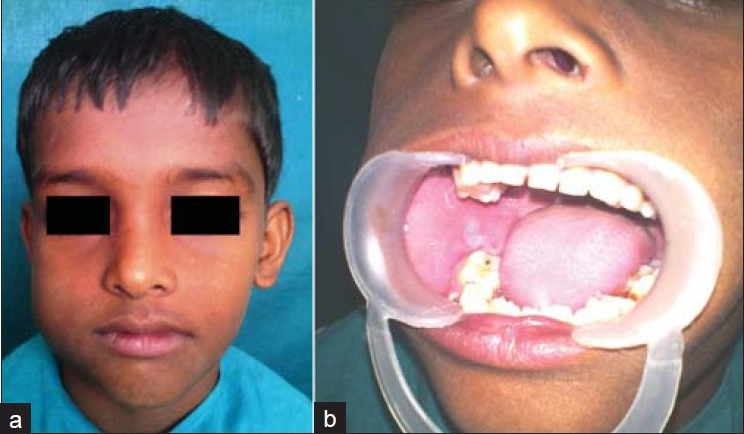
(a) Preoperative facial view showing asymmetry of face at the age of 6 years, (b) Preoperative intra-oral view showing cortical plate expansion and obliterated vestibule
Figure 1(c,d).
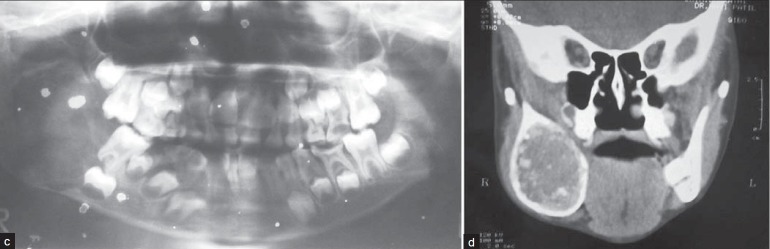
(c) Preoperative panoramic radiograph showing large radioluceny, well-defined sclerotic border along with radiopacity observed in the center of the lesion (Archival), (d) Preoperative computed tomography showing cortical plate expansion, lesion measuring about 4 cms × 5 cms
Figure 2.
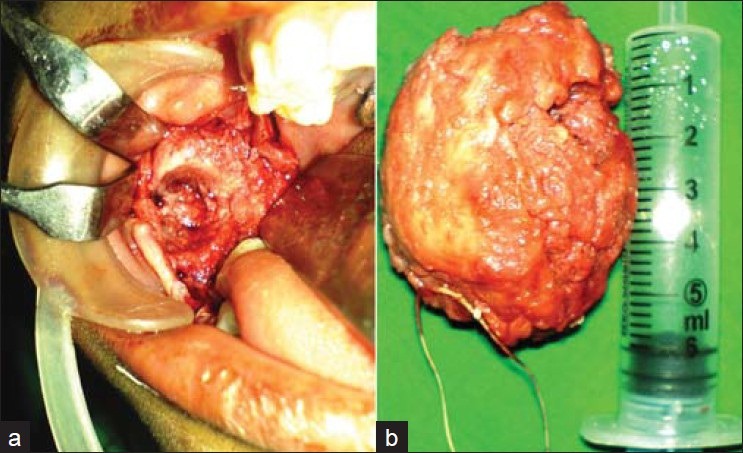
(a) Surgical excised view, (b) Excised specimen measuring about 4.5 cms × 5.5 cms
Figure 3(a,b).
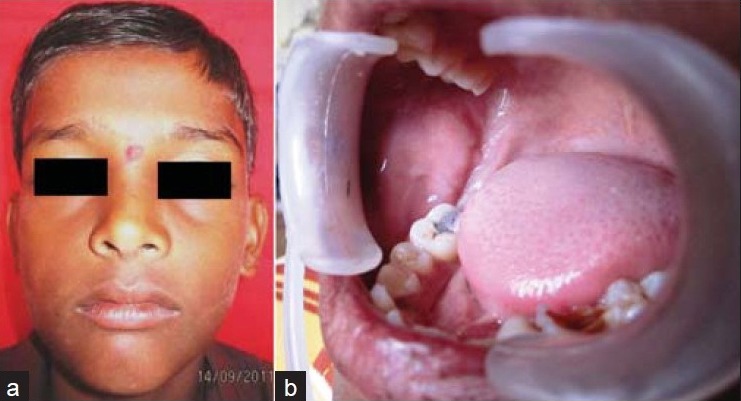
Postoperative facial view showing bilaterally symmetrical of face at the age of 10 years after 3 years of follow-up, (b) Postoperative intraoral view showing normal study with restored 46 tooth
Figure 3(c,d).
(c) Postoperative panoramic radiograph showing normal bone pattern, (d) Postoperative computed tomography
DISCUSSION
Ossifying fibroma, first described in 1872, is a rare, benign primary bone tumor that occurs most commonly in the jaw. In 1927, it was coined as ossifying fibroma, and when this tumor occurs in children, it has been named juvenile aggressive ossifying fibroma.[5] The PsJOF was first reported in 1938, and termed as osteoid fibroma with atypical ossification of the frontal sinus. Later, in 1949, two cases were reported and called as PsJOF.[6] The most recent classification is by El Mofty who identified two categories, trabecular JOF (TrJOF) and psammomatoid JOF (PsJOF) based on histologic criteria.[2] The psammomatous type mainly involves the bones of the orbit and paranasal sinuses, whereas the trabecular type commonly involves the jaws, although there is controversy as to which jaw has greater predilection, maxilla or mandible. These lesions exhibit a slight male predilection.[4] One of the case study series reported 70% of the PsJOF occurred in the paranasal sinus, 20% in the maxilla, and only about 10% in the mandible. In addition to its aggressive behavior, this lesion also has a very strong tendency to recur, and recurrence rate as high as 30%-56% have been reported.[6] Because of their slow asymptomatic growth, they may be quite large on initial presentation.[4]
The pathognomonic feature of this fibro-osseous lesion is the presence of eosinophilic spherical structures dispersed in a fibrous stroma consisting of plump spindle-shaped cells that are arranged as strands and whorls, this unique spherical structure is termed as psammoma-like bodies. These particles vary in appearance, but usually have a central basophilic area and a peripheral eosinophilic fringe. Ultrastructurally, the psammoma–like bodies in PsJOF were found to possess a dark rim of crystals, from which small spicules and needle-like crystalloids project toward the periphery.[6,7]
As in our case, a predominantly cellular connective tissue stroma composed of numerous spindle-shaped cells arranged in fascicular storiform pattern. In between these irregular strands of trabeculae and plump osteoblast spheroidal ossicles basophilic in center and eosinophilic in periphery resembling psammoma-like bodies were seen. There was no atypia or mitotic activity seen [Figure 3e].
Figure 3e.
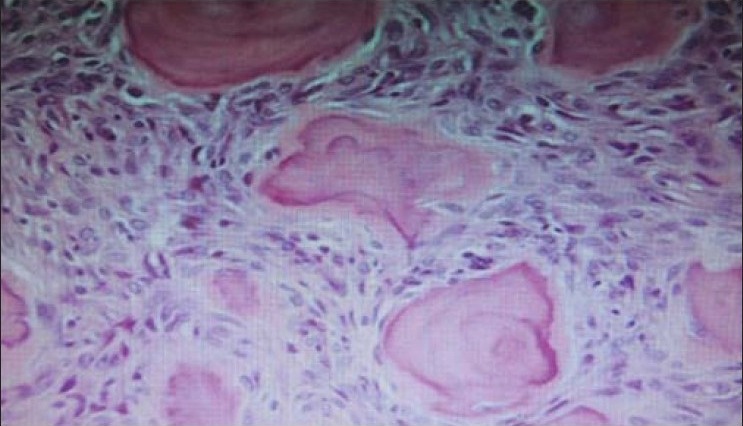
Irregular strands of trabeculae, plump osteoblast spheroidal ossicles with basophilic in center and eosinophilic in periphery resembling psammoma-like bodies.
There is no standardized follow-up protocol in the literature; because of the fairly high recurrence rate, immediate reconstruction is not advised. The smaller tumors may be treated by enucleation and curettage successfully. Resection should be considered also in cases where there is a recurrence, invasion of adjacent cavities, or where preserving the inferior border is not feasible.[4,8,9] The lesion which is not involving the adjacent structures, no paresthesia of lip and the significantly intact inferior border of mandible allow to plan the case primarily for conservative management that is excision and curettage. In addition to high recurrence rate of this fibro-osseous lesion it warrants continued patient follow-up.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Keles B, Duran M, Uyar Y, Azimov A, Demirkan A, Esen HH. Juvenile Ossifying Fibroma of mandible: A case report. [Last accessed on 2010];J Oral Maxillofac Res. 2010 1:e5. doi: 10.5037/jomr.2010.1205. Available from: http://www.ejomr.org/JOMR/archives/2010/2/e5/e5ht.pdf . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ravikumar R, Raghavendra K, Kumar S. Aggressive juvenile ossifying fibroma of the anterior mandible. J Dent Sci Res. 2011;2:26–34. [Google Scholar]
- 3.Tamgadge SA, Tamgadge AP, Bhatt DM, Bhalerao S, Trevillie Periera, Gotmare S. Juvenile ossifying fibroma (Psammomatoid type) of the maxilla: A case report. Sci J. 2009;3:14–6. [Google Scholar]
- 4.Smith SF, Newman L, Walker DM, Papadopoulos H. Juvenile aggressive psammomatoid ossifying fibroma: An interesting, challenging, and unusual case report and review of the literature. J Oral Maxillofac Surg. 2009;67:200–6. doi: 10.1016/j.joms.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 5.Kashyap RR, Naik GR, Gogineni SB. Asymptomatic presentation of aggressive ossifying fibroma: A case report. Case Rep Dent Vol. 2011;2011:523751. doi: 10.1155/2011/523751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Solomon M, Khandelwal S, Raghu A, Carnelio S. Psammomatoid juvenile ossifying fibroma of the mandible: A Histochemical insight. Internet J Dent Sci. 2009;7:2. [Google Scholar]
- 7.Weing BM, Vinh TN, Smirnitopoulous JG, Fowler CB, Houston GD, Heffner DK. Aggressive psammomatoid ossifying fibromas of the sinonasal region: A clinic opathological study of a distinct group of Fibro-Osseous Lesions. Cancer. 1995;76:1155–65. doi: 10.1002/1097-0142(19951001)76:7<1155::aid-cncr2820760710>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 8.Marx RE, Stern D. Carol Stream, IL: Quintessence Publishing Co Inc; 2003. Fibro-osseous diseases and systemic diseases affecting bone, in oral and maxillofacial pathology: A rationale for diagnosis and treatment; p. 781. [Google Scholar]
- 9.MacIntosh RB. Juvenile ossifying fibroma. Oral Maxillofac Surg Clin North Am. 1997;9:713–20. [Google Scholar]


