Abstract
Objectives:
The aim of the current study was to investigate how bilateral cleft lip and palate (BCLP) cases responded differently to presurgical orthopedics (PSO) and primary lip repair (LR) based on premaxillary characteristics. We suggest a clinically oriented descriptive classification for BCLP based on premaxillary characteristics.
Design and Setting:
A retrospective longitudinal comparative study where available records of all non-syndromic patients with complete BCLP attending the Cleft Clinic, affiliated to the Oral and Maxillofacial Surgery department, Ain-Shams University, Cairo, Egypt were assessed.
Sample Population and Methodology:
Twenty-two cases were collected over a 4-years period from 2008 to 2011 (15 boys and 7 girls). Model assessment was performed for serial models representing four stages of treatment; M1: Prior to start of PSO, M2: At the end of PSO, M3: One month after LR, M4: Three months after LR. The premaxillary and vomerine widths were measured on M1. Models (M1-M4) were assessed for changes in anteroposterior projection, anterior arch width, intercanine width and posterior arch width and results were statistically analyzed. Intra-and postoperative surgical findings during and after primary LR were recorded. The sample was divided into two groups based on the premaxillary size and characteristics; Group R: Rudimentary premaxilla and Group P: Prominent premaxilla.
Results:
There was a highly significant difference in premaxillary width between the two groups (P = 0.00), changes in anteroposterior projection of the premaxilla were significant one and three months after LR. Changes in maxillary anterior arch width, intercanine and posterior arch widths were non-significant between groups. Mean age difference between the two groups was only statistically significant at the stage of LR. Surgical differences were noted between the two groups. Postoperatively as compared to group R; group P showed more premaxillary bulge and show at rest, as well as more prolabial stretching. In addition, facial profile was more convex in group P.
Conclusion:
The two types of BCLP outlined in this study are different from several aspects, and hence management should be modified according to each case. This descriptive classification provides a useful tool for evaluation and planning of patients with BCLP.
Keywords: Arch collapse, bilateral cleft lip and palate, lip repair, premaxilla, premaxillary size, presurgical orthopedics
INTRODUCTION
Cleft lip and palate (CLP) is one of the most common congenital facial anomalies. Several factors contribute to development of CLP; most clefts are considered to be of multifactorial origin.[1] Several classifications for oral clefts have been introduced over the years.[2–6] In 1980 Millard[7] stated that “the initial state is the precondition that determines the subsequent state”. Berkowitz[8] suggested that if a single cleft type exhibits multiple variations in morphology, one rigid formula for treatment technique and timing may not be effective. Therefore, accurate delineation of the initial state is essential to final outcome assessment.
Currently a number of approaches are still being developed and modified in attempts to characterize many features of CLP.[9–12] Complete bilateral CLP (BCLP) is the most severe of the common orofacial cleft subtypes. However, great variations in cleft anatomy in BCLP were reported by several authors.[13,14] As described by Hodgkinson, et al.,[15] the premaxilla and prolabial segment can either project or rotate up under the nose or may appear to be missing in some views.
Management of the protruding premaxilla varied along history. Starting from the sixteenth through the eighteenth century management of protruding premaxilla involved surgical excision of the premaxilla followed by surgical union of the lateral lip elements with or without the prolabium. This brutal treatment was associated with deleterious esthetic and functional outcomes. Later on retraction of the protruding premaxilla has been adopted utilizing variable devices. The era of modern presurgical orthopedics date back to 1950's and has steadily evolved ever since. Currently presurgical orthopedics are considered mandatory in severe cases and includes a wide range of devices that are active or passive, extraoral or intraoral, or both.[16–20]
Lip repair is usually performed for infants with BCLP between three to six months as suggested by Mulliken.[21] Variations in arch collapse following lip repair were discussed by several investigators[22–24] but nevertheless were not attributed to the size of the premaxilla.
Throughout our work with infants suffering from BCLP it is agreed that the general term “BCLP” is usually a misleading description as not all bilateral cases possess the same pre-maxillary characteristics. It has been observed that individual cases possess some resemblances and variances during presurgical orthopedics and primary surgical repair of the lip. Arch dimensions varied after presurgical orthopedics, as well as after surgery depending on premaxillary size. Moreover, facial appearance differed accordingly based on the preoperative size of the premaxilla.
Therefore; the aim of the current retrospective study was to find out how different BCLP cases responded to presurgical orthopedics and primary surgical repair of lip based on variations in pre-maxillary characteristics. In this respect, we suggest a clinically oriented descriptive classification for BCLP based on premaxillary characteristics. This classification can aid in treatment planning and outcome prediction.
MATERIAL AND METHODS
This is a retrospective longitudinal comparative study where data were obtained from the records of all patients with non-syndromic complete BCLP attending the Cleft Care Clinic, affiliated to the Oral and Maxillofacial Surgery department, Faculty of Dentistry, Ain-Shams University. This study received exemption from the research ethics committee as it only involved records, models and photographs obtained from the department archives. Data were coded so patient's identity could not be revealed. Twenty-two cases were collected over a 4 years period from 2008 to 2011 (15 boys and 7 girls). Selection of cases was based on the following criteria: a) complete bilateral cleft of lip, primary and secondary palate, b) serial models available from birth until three months after primary lip repair, c) the availability of full records.
Data were collected in two phases of primary treatment; presurgical orthopedics and primary surgical repair of lip phases based on model assessments, intra-and postoperative clinical findings and observations.
All patients included in the study underwent the same pre-surgical orthopedic procedure by the same orthodontist using the same type of orthopedic appliance. An opened jackscrew with a 12 mm range was used to retract the premaxilla as shown in Figure 1. Appliance retention was mainly obtained by peripheral seal phenomenon, in addition to zinc free denture adhesive applied once daily. The parents were instructed to remove the appliance twice daily for cleaning and were instructed to activate the screw only once daily. The baby was followed up weekly and any incidents of appliance misuse or negligence were recorded. When the screw was fully closed and the premaxilla still needed retraction, another appliance with a jackscrew was fabricated and delivered in the same fashion till the required retraction was achieved.
Figure 1.
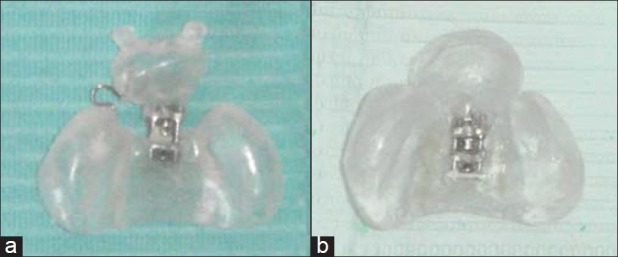
(a) The orthopedic appliance was made from self-cured orthodontic acrylic resin. Appliance was horizontally sectioned into two components, a premaxillary cup that holds the premaxilla and a posterior section that covers the lateral arches. An opened unidirectional jack screw was placed in line with a point representing the premaxillary center between the two sections to retract the premaxilla posteriorly. Retention buttons, described by Grayson,[27] may be added to the premaxillary section whenever additional external retention is needed. In this fi gure, a piece of 0.9 mm wire was placed to resist lateral movement of the already shifted premaxilla. (b) Orthopedic appliance after being fully closed
Bilateral synchronous “Millard”[25] lip repair was performed for all cases, neither gingivoperiosteoplasty nor early alveolar bone grafting was performed.
Model assessment
Measurements of dental models were obtained on four different time frames R. Four mouth casts of each baby were selected from the clinic archives. The four models represent stages of treatment; M1-Prior to presurgical orthopedics, M2-At the end of presurgical orthopedics (prior to lip repair), M3-One month after lip repair, M4-Three months after lip repair.
The following measurements were performed manually on the study models of each patient using vernier caliper [Figure 2]; M1: Measuring anteroposterior projection (I-TT’)[26] of the premaxilla, width of the premaxilla (PP’), width of the vomer (SS’), anterior arch width of the palate (LL’),[26] intercanine width (CC’),[26] and posterior palatal width (TT’).[27] On models M2, M3, M4 changes in L-TT’, LL’, CC’ and TT’ were measured.
Figure 2.
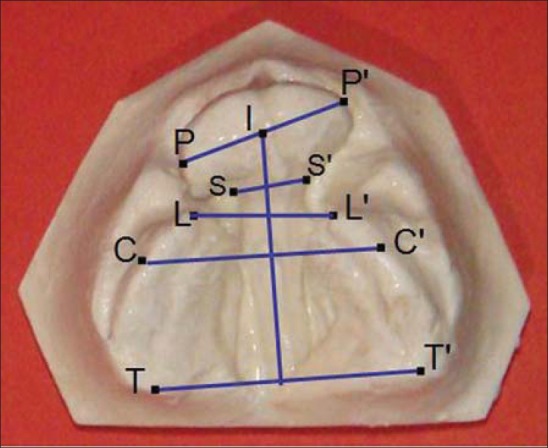
Points identifi ed and linear distances measured. Point P represents the lateral end of the premaxilla at its widest dimension. Point I refers to the point on the alveolar crest where the incisive papilla and labial frenulum meet. Point L is the most anterior point of the alveolar crest of the lateral segment. Point C (cuspid point) it is the point where the lateral sulcus meets the crest of the alveolar ridge. Point T (tuberosity point) is the most posterior point on the maxillary tuberosity. Point S is a point on the nasal septum at its lateral surface just posterior to the premaxilla. PP’ refers to the width of the premaxilla. Distance from point I to the line joining TT’ measures the anteroposterior projection of the premaxilla. LL’ represents the anterior arch width. CC’ refers to the intercanine width. TT’ describes the posterior arch width. SS’ measures the width of the nasal septum just posterior to the premaxilla
Surgical and postsurgical findings
Cases were assessed regarding the following intraoperative findings during primary lip repair: Age at which primary lip repair was performed, size of prolabium, amount of soft tissue dissection needed.
Following lip repair, cases were assessed regarding occurrence of the following postoperative observations: Premaxillary bulge, premaxillary show at rest, shape of palatal arch and prolabial stretching. Comments on patients profile during early follow-up phase were also noted.
The collected data was revised, coded, tabulated and analysed using Statistical package for Social Science (SPSS 15.0.1 for windows; SPSS Inc, Chicago, IL, 2001). Data was presented and suitable analysis was done according to the type of data obtained for each parameter.
Statistical analysis
Descriptive statistics included calculation of mean, standard deviation (±SD), minimum and maximum values (range) for numerical data and frequency and percentage of non-numerical data.
Analytical statistical measurements’ obtained from the two categories were analyzed using paired samples T-test for comparison between different time frame measurements in the same group (intra-group differences). The independent samples T-test was used to assess the statistical significance of the difference between two study group means in each time frame (inter-group differences). Chi-square test was used to examine the relationship between two qualitative variables. The significance and P value were set that P >0.05: Non significant (NS), P <0.05: Significant (S) and P <0.01: Highly significant (HS).
Error of the method
To assess measurement error in both groups, all casts were re-measured by the same examiner after 1 week interval from the date of the first measurements. Alpha (Cronbach) reliability analysis was used to measure intra-observer reliability for all measurements in all four stages of treatment. Reliability was found to be highly significant for all measurements. Means’ summaries was 0.006 for all variables in M1 treatment stage, 0.003 in M2, 0.007 in M3, and 0.002 for all variables in M4 treatment stage.
Cases were divided into two groups according to variation in pre-maxillary characteristics and measurements;
Group P: This signifies BCLP characterized by well-developed (P) prominent pre-maxilla as regards size, as well as response to presurgical orthopedics and lip repair. This category included 16 cases.
Group R: This signifies BCLP characterized by ill-developed (R) rudimentary pre-maxilla as regards size, as well as response to presurgical orthopedics and lip repair. This category included six cases.
RESULTS
Analysis of models at different stages of treatment
The pre-orthopedic treatment width of the premaxilla was 13.2 ± 0.5 for group R and 18.0 ± 0.7 for group P and this difference was highly significant (P = 0.00). While the Vomer thickness was 7.7 ± 1.9 for group R and 8.2 ± 1.7 for group P, and this difference was non-significant (P = 0.69). Mean and standard deviation values for changes in the anteroposterior position of premaxilla in different stages of treatment for groups R and P are presented in Table 1. Statistical analysis of this data [Table 5] showed that these changes were only significant 1 and 3 months after lip repair. Mean and standard deviation values for changes in the maxillary anterior arch width in different stages of treatment for groups R and P are presented in Table 2. Statistical analysis of this data Table 5 showed that these changes were all non-significant. Mean and standard deviation values for changes in the intercanine width in different stages of treatment for groups R and P are presented in Table 3. Statistical analysis of this data Table 5 showed that these changes were non-significant. Mean and standard deviation values for changes in the maxillary posterior arch width in different stages of treatment for groups R and P are presented in Table 4. Statistical analysis of this data Table 5 showed that these changes were also non-significant. Figures 3 and 4 represent changes along different treatment stages for groups R and P.
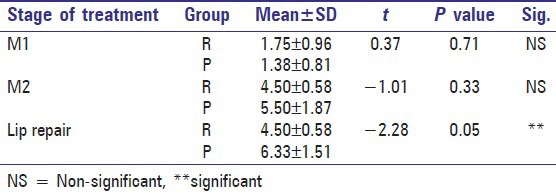
Table 1.
Comparison between means and SD of anteroposterior position of premaxilla in different stages of treatment among group R and P
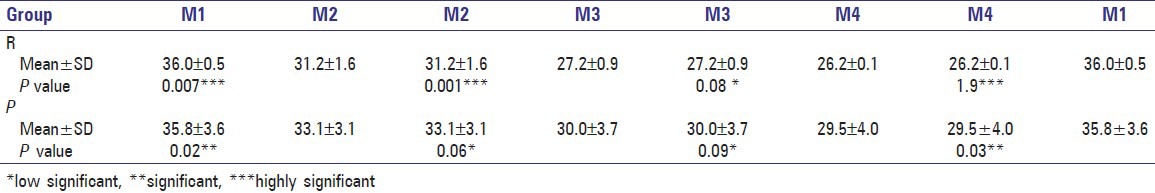
Table 5.
Comparison between means and SD of all assessed parameters of groups R and P at different stages of treatment
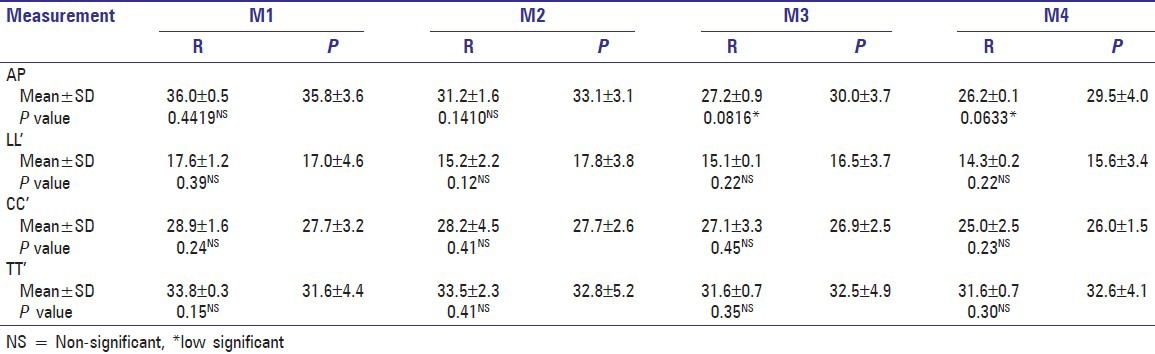
Table 2.
Comparison between means and SD of anterior arch width (LL’) of premaxilla in different stages of treatment among group R and P
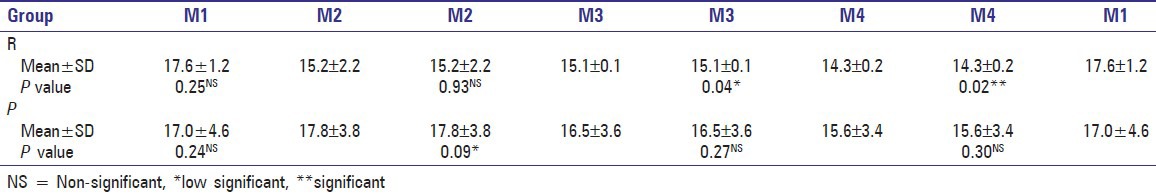
Table 3.
Comparison between means and SD of inter-canine width (CC’) in different stages of treatment among group R and P
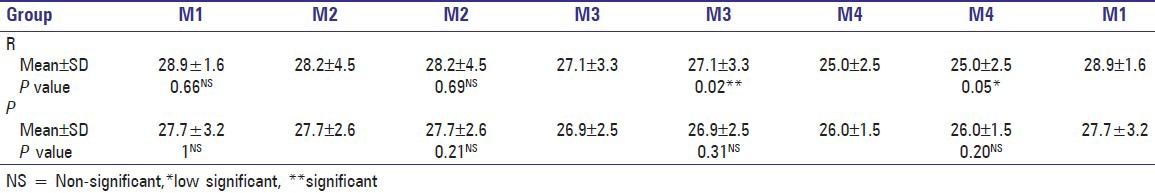
Table 4.
Comparison between means and SD of maxillary posterior arch width (TT’) in different stages of treatment among group R and P
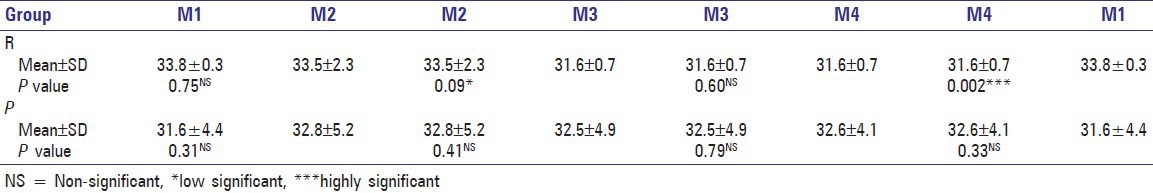
Figure 3.
Case # 1 from group P. Age at start of orthopedic therapy was 1.4 months, at the time of primary lip repair was 6.7 months; (a) Pre-orthopedic treatment, (b) Post orthopedic treatment, just before primary lip repair, (c) One month post primary lip repair, (d) Three months post lip repair (note V-shaped arch)
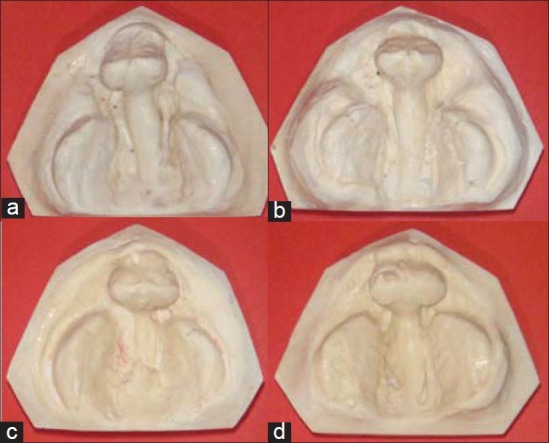
Figure 4.
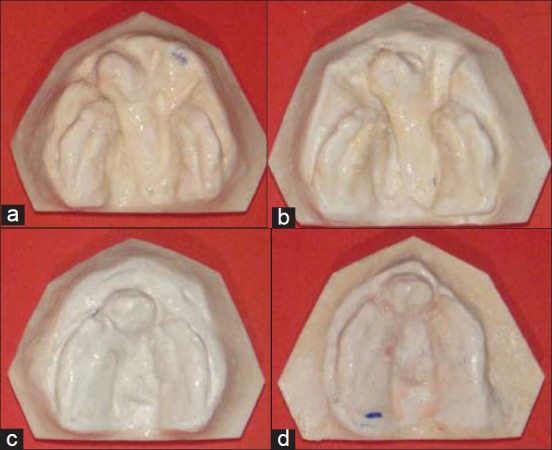
Case #2 from group R. Age at start of orthopedic treatment was 3 weeks and at primary lip repair was 3.2 months; (a) Pre orthopedic treatment, (b) Post orthopedic treatment, (c) One month post lip repair,(d) Three months post lip repair (note U-shaped arch)
The mean ages for groups R and P at different stages of treatment is shown in Table 6. Statistical analysis of these results showed that the difference between both groups was only statistically significant at the stage of lip repair where those from group P were older.
Table 6.
The mean ages between group R and P at different stages of treatment
Intra-and postoperative findings
For group P, the prolabium was evidently larger and tissues covering the premaxilla were firmly adherent keratinized oral mucosa. While for group R, the prolabium was evidently smaller and the premaxilla was covered with loosely adherent vestibular mucosa except for a thin strip of keratinized mucosa at the occlusal aspect [Figure 5].
Figure 5.
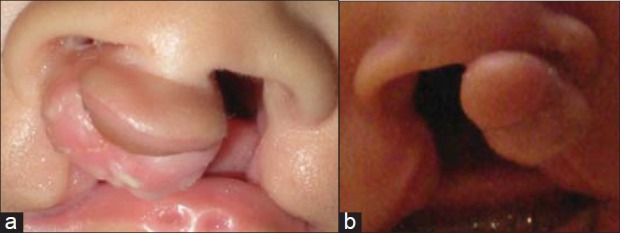
Variation in prolabial width, width and shape of premaxilla and soft tissue coverage between the two BCLP categories; A: Group P, B: Group R
All cases received bilateral Millard synchronous lip repair where reconstruction of the labial vestibule in the anterior region and adequate upper lip length were achieved. The amount of soft tissue dissection needed was far more in group P in order to cross over the anteriorly jutting premaxilla and offer tension free primary closure.
The constant postoperative finding following lip repair in the group P was premaxillary bulge and show at rest. Atleast one third of the premaxilla was exposed underneath the vermillion border of the upper lip [Figure 6]. This was considered an unavoidable outcome in the postoperative phase and was not seen in group R. It was noted that patients profile was more convex in group P unlike the profile in group R, which was more concave.
Figure 6.
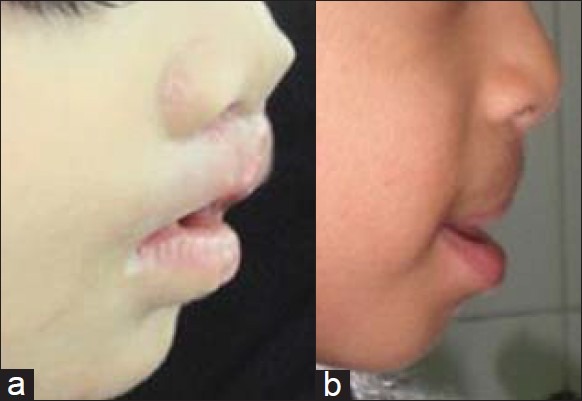
Variation in lateral profi le following lip repair between the two BCLP categories; (a) More convex in group P, (b) More concave in group R
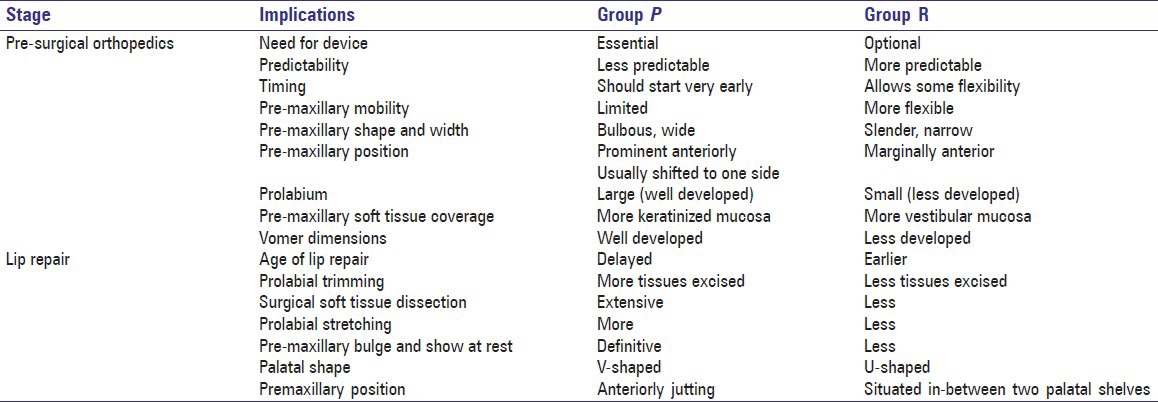
Comparison between group P and group R based on implications on presurgical orthopedics and primary lip repair are shown in Figures 5, 6 and listed in Table 7.
Table 7.
Comparison between group P and R based on implications on treatment stages
DISCUSSION
There is no universally accepted classification of cleft deformities.[2–6,9–12] Current classification systems possess limitations that could be summarized as being complex, exhaustive, time consuming, extensive, difficult to remember, prone to errors and incapable of revealing at a glance what is the original deformity. In addition, those classifications could not predict treatment outcomes in different phases of cleft rehabilitation.[13–15]
During treatment of patients with BCLP over a period of more than 4 years at our cleft clinic, it was observed that cases responded differently to presurgical orthopedics and lip repair utilizing the same surgical technique, irrelevant of the cleft surgeon. Some cases were technically simple while others were particularly challenging. After observing the response, it was thought that not all BCLP cases could be pooled under the same category nor treated following the same regimen nor can we expect the same outcomes. In order to understand how BCLP cases responded differently to presurgical orthopedics and primary lip repair, we assessed available records of patients with BCLP (up to three months following primary lip repair). In this respect we suggest a clinically oriented descriptive classification for BCLP based on premaxillary characteristics.
In agreement with Hodgkinson, et al.,[15] it was observed that the size of the premaxilla varied greatly from one case to the other. Such variability ranged from a small slender pendulum shaped premaxilla to a large bulbous form. Therefore, cases were grouped according to the premaxillary shape and size into two categories; group P and R. In agreement with Ross and Johnston;[28] the width of the premaxilla differed significantly between the two groups. In the current study, the width of the premaxilla varied from 12-18 mm. Therefore, it was considered that a premaxilla 13 mm or less was a small-sized premaxilla and cases were included in group R.
These differences in presentation in BCLP have been attributed to several factors in literature. This might partially be due to varying amount of intrinsic developmental deficiency. The size is strongly affected by alveolar bone apposition, which is associated with the development and eruption of the incisors,[29,30] and partially by the nasal septum.[31,32] Ross and Johnston,[28] as well as Heidbuchel, et al.,[33] suggested that premaxillary protrusion could be be a result of intrinsic anatomical aberrations such as the absence of alveolar, as well as palatal hard and soft tissues and suggested that tongue activity against the flexible unsupported premaxillary bone could be a contributing factor. Furthermore; Latham[34] proposed three contributing factors to the extensively protruding premaxilla: The septo-premaxillary ligament, the abnormal direction of alveolar growth, and underdevelopment of the maxillary segments.
On the other hand, it was observed that patients who had poorly developed nasal septum and small premaxilla (group R) differed significantly from those patients in group P. Noordhoff, et al.[35] suggested that some cleft patients show deficient median facial structures without any gross abnormalities of the brain. Noordhoff, et al.[35] and most recently Allam et al., in 2011,[36] referred to patients with non-syndromic BCLP who present with small premaxilla and poor maxillary growth as microforms of median facial dysplasia.
To our knowledge the percentage of occurrence of the two groups described in this article has not been mentioned elsewhere in literature. Based on the literature describing management and etiology of prominent premaxilla versus that describing small premaxilla, and according to the sample size included we suggest that patients with prominent premaxilla (group P-sixteen case) were almost three folds more than those with rudimentary premaxilla (group R- six cases). In order to confirm these findings larger sample size is needed.
The results of the current study showed that patients in group R showed a highly significant reduction in the anteroposterior projection of the premaxilla in the phases M1-M3 and a significant one after lip repair (M3-M4). This could be attributed to the small size of the premaxilla and the more flexible attachment between the premaxilla and vomer observed in group R. On the other hand, in the group P, reduction in the anteroposterior projection was significant only between the M1-M2 phases and the change was of lower significance after lip repair i.e. between M3-M4. This could be attributed to the more firm attachment between the premaxilla and the vomer in group P. Moreover; the larger sized premaxilla in group P cannot fit in between the two palatal shelves located posterior to it, hence it stays locked anteriorly contributing to the V-shaped arch observed in this group. In agreement with da Silva, et al,[37] the most significant finding consequent to lip repair was reduction of the premaxillary anterior projection and lingual tipping of the upper incisors. Retropositioning of the premaxilla, especially in the alveolar part, is a desired effect of lip repair, especially in group P.
The mean ages at the time of primary lip repair was 4.50 ± 0.58 for group R and 6.33 ± 1.51 for group P. This difference was statistically significant where those from group P were older. This could be attributed to the more flexible premaxillary-vomerine junction in group R. There is correlation between the highly significant change in anteroposterior projection observed in phases M1-M3 and reduced time prior to lip repair. Furthermore, this difference could be attributed to the longer presurgical orthopedics phase in infants in group P where one case might require more than one device to achieve acceptable outcome. This seems to be in accordance with the age range reported by LaRossa in year 2000[20] for primary cleft lip repair in cases with BCLP; where 90% of cleft teams in the world repair the lip between three and six months of age.
According to the model measurements and in agreement with Mulliken,[21] after lip repair in infants with protruding premaxilla; establishment of a continuous band of orbicularis oris muscle will help mold the premaxilla back to a varying degree. This molding depends on several factors: Whether the orbicularis oris muscle was repaired in an end to end fashion underneath the prolabium, whether there is space in-between the palatine shelves to accommodate the mediolateral width of the premaxilla and the original degree of protrusion.
With respect to palatal changes following lip repair; reduction in the most anterior arch width (LL’) and intercanine width (CC’) were only significant in group R after lip repair in M3-M4. This could be explained by the direct transmission of compressive muscular forces exerted by the lip on the lateral sides of the upper arch after lip repair (where the premaxilla is retracted posteriorly in-between the two palatine shelves giving a U-shaped arch). On the other hand, the change in anterior arch width was of lower significance in group P (where change is seen one month after lip repair). This could be attributed to the presence of the prominent premaxilla that is locked in front of the palatal shelves preventing lateral forces from being directly transmitted to palatal shelves.
In agreement with Hagerty, et al.,[22] and Vargervik[23] who described the influence of musculature after lip repair on dental arch dimensions, they suggested that arch collapse occurs consequent to tight upper lip following lip repair. They noted that in normal arches both the buttresses and tongue counteract constricting muscle forces. In cases with BCLP prior to lip repair, forces from the tongue flares-out the anteriorly suspending premaxillary segment more upwards and forwards and in the same time allows expansion of the unbounded palatal shelves. The tongue forces are not balanced by compressive lip forces. Lip repair results in bilateral arch collapse in all samples studied with palatal segments meeting anteriorly behind the premaxilla, locking it out of the arch therefore, the arch tends to be more V-shaped in group P.
Regarding the changes in the maxillary posterior arch width (TT’), there was only low significant change in group R one month after lip repair. There was a highly significant difference at the end of three months after lip repair as compared to M1. Change in posterior arch width was of no significance in group P. This could be attributed to position of the premaxilla in relation to the palatal shelves and transmitted lip pressure after lip repair. Moreover it could be suggested that the type of bone in midface buttresses might differ in between the two groups as observed in the more flexible premaxillary-vomerine attachment in group R. This is a beneficial finding which explains why patients with BCLP always suffer anterior collapse rather than collapse along the whole length of the upper arch.[22,23] This finding is important when planning orthodontic expansion for those patients later on prior to alveolar cleft grafting as suggested by Heidbuchel and Kuijpers-Jagtman.[38]
It is worthy to mention that in the sample included, the amount of keratinized oral mucosa covering the premaxilla differed between the two groups. This finding was not otherwise reported in literature. We suggest that several factors could attribute to this finding, including possible difference between the two groups regarding the etiologic nature of the cleft, the size of the premaxilla and the number of teeth present in the group P, which was observed to be more than that seen in group R. This last finding was in agreement with the work of Atherton and King et al.[29,30]
Corresponding to the size and shape of the premaxilla, the size of prolabium was evidently larger in group P as compared to group R. Prolabial size has certain implications on the surgical technique of lip repair. It is known that the prolabial size (length and width) is one of the cleft elements that is programmed for rapid growth and should be trimmed to a smaller than-normal size to overcome future prolabial stretching.[39,40] In group P, wide prolabium could be easily trimmed due to the abundance of prolabial tissues.[21] However, in group R the prolabium is already small in width and trimming should be performed with great caution to preserve blood supply to this critically small portion of soft tissue. Moreover prolabial stretching was observed postoperatively in group P as compared to narrow prolabium and inconspicuous scar in group R. This could be possibly attributed to the backward tension effect applied on the repaired lip from the prominent premaxilla as opposed to the lateral pull from lateral lip elements that could be higher in group P. Furthermore in agreement with Liao, et al.,[41,42] there is a correlation between differences in growth potential between the two groups based on the infantile size of the premaxilla.
As related to other aspects of lip repair, cases from group P were considered more challenging. Where staged closure of BCL, one side and then the other side, has been abandoned in the last quarter century. Synchronous repair of the BCL, and nose has become the “state of the art” during the past decade.[21] In the current study, it was found that the wide gap between the premaxilla and lateral lip elements, as well as the firm premaxillary-vomerine attachment required more extensive sub-or supraperiosteal dissection was needed as suggested by Delaire.[43] This wide dissection was done to allow lateral lip elements to cross over the firmly attached, anteriorly jutting premaxilla and offer tension free primary closure. On the other hand, cases from group R were less challenging in this respect. Limited dissection was required, as lateral lip elements were already in close approximation to the premaxillary and prolabial segment and the premaxillary- vomerine attachment was more flexible and thus pushed backwards during surgical lip repair.
One of the most striking features after lip repair in patients in group P is the premaxillary bulge and show at rest. We suggest that the reason for this unpleasing finding was explained by Mishima, et al., in 1997,[24] after lip repair the vomer and premaxilla shifts downwards and posteriorly with a tendency for collapse seen in the lateral segments as explained earlier. This downward shift and collapse in lateral segments results in and explains the reason for premaxillary bulge and show at rest after lip repair. This retroclination appears secondary to tension exerted by scar tissues formed following lip repair.
It is worthy to mention that dentoskeletal abnormality and midfacial growth deficiencies is thought to be both an inherent aspect of CLP and a possible consequence of surgical intervention.[44,45] Liao, et al.,[41,42] demonstrated in their study that the size of the premaxilla in infants with BCLP varied greatly. The size of a premaxilla may give indication of growth potential of maxillary growth. This was in agreement with the findings of the current study where facial profile varied between the two groups; in group P it was more convex as compared to concave profile in group R. Handelman and Pruzansky in 1968[45] reported about the occurrence of anterior cross bite in patients with BCLP, and suggested that the size of the premaxilla in infants with BCLP can be used to predetermine subsequent craniofacial morphology at the age of 5 years. Children with BCLP with a large premaxilla demonstrated a more favorable maxillary growth, in length, than those with a small premaxilla. The same finding is reinforced in our study. All cleft patients have a certain amount of tissue deficiencies. These deficits are most severe in bilateral medial facial dysplasia patients.[35,36,46]
In an attempt to offer better future prediction, standardization and better quality of treatment for patients of different categories of BCLP, this study was conducted in agreement with Liao, et al.,[41,42] who suggested that the initial size of the infantile premaxilla could be used as a predictor for the final treatment outcome. In our sample studied premaxillary characteristics influenced treatment outcomes with respect to postoperative facial appearance and maxillary arch form. In contrast to what have been reported by Perlyn, et al.,[47] the patterns of variation within the initial dysmorphology of the maxillary arch in infants with complete BCLP cannot be used to predetermine subsequent occlusal relationships and that early treatment of cleft patients cannot be adopted on an evidence-based fashion.
CONCLUSION
Within the limitations of this study, it can be concluded that the two types of BCLP outlined in this study group P and group R are different from several aspects, and hence expectations and management should be modified according to the individual needs of each case. In conjunction with other general classifications, this descriptive classification for the characteristics of premaxilla provides a useful tool for evaluation and planning of patients with BCLP.
Recommendations
Genetic and radiographic assessments are mandatory for young patients with BCLP to delineate categorical differences on both levels. Multilevel modeling at older age groups is needed to verify the effect of premaxillary characteristics on alveolar cleft grafting and occurrence of maxillary deficiency. Longitudinal follow-up for the patients and larger study sample size are necessary to confirm the results.
Footnotes
Source of Support: Nil
Conflict of Interest: No.
REFERENCES
- 1.Lidral AC, Moreno LM, Bullard SA. Genetic factors and orofacial clefting. Semin Orthod. 2008;14:103–14. doi: 10.1053/j.sodo.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thornton JB, Nimer S, Howard PS. The incidence, classification, etiology, and embryology of oral clefts. Semin Orthod. 1996;2:162–8. doi: 10.1016/s1073-8746(96)80011-9. [DOI] [PubMed] [Google Scholar]
- 3.Pruzansky S. Description, classification, and analysis of unoperated clefts of the lip and palate. Am J Orthod. 1953;39:590–611. [Google Scholar]
- 4.Kernahan D, Stark R. A new classification for cleft lip and cleft palate. Plast Reconstr Surg. 1958;22:435–41. doi: 10.1097/00006534-195811000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Elsahy NI. The modified striped Y: A systematic classification for cleft lip and palate. Cleft Palate J. 1973;10:247–50. [PubMed] [Google Scholar]
- 6.Millard DR. Primary correction of unilateral cleft nose: A more accurate diagram. Plast Reconstr Surg. 1999;103:2094–8. doi: 10.1097/00006534-199906000-00073. [DOI] [PubMed] [Google Scholar]
- 7.Millard DR. The alar cinch in the flat, flaring nose. Plast Reconstr Surg. 1980;65:669–72. doi: 10.1097/00006534-198005000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Berkowitz S. Primary repair of cleft lip and nasal deformity. Plast Reconstr Surg. 2002;109:2158–61. doi: 10.1097/00006534-200205000-00067. [DOI] [PubMed] [Google Scholar]
- 9.Friedman HI, Sayetta RB, Coston GN, Hussey JR. Symbolic representation of cleft lip and palate. Cleft Palate Craniofac J. 1991;28:252–60. doi: 10.1597/1545-1569_1991_028_0252_srocla_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 10.Smith AW, Khoo AK, Jackson IT. A modification of the Kernahan “Y” classification in cleft lip and palate deformities. Plast Reconstr Surg. 1998;102:1842–7. doi: 10.1097/00006534-199811000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Ortiz-Posadas MR, Vega-Alvarado L, Maya-Behar J. A new approach to classify cleft lip and palate. Cleft Palate Craniofac J. 2001;38:545–50. doi: 10.1597/1545-1569_2001_038_0545_anatcc_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 12.Rossell-Perry P. New diagram for cleft lip and palate description: The clock diagram. Cleft Palate Craniofac J. 2009;46:305–13. doi: 10.1597/08-070.1. [DOI] [PubMed] [Google Scholar]
- 13.Friede H, Johanson B. A follow-up study of cleft children treated with vomer flap as part of a three-stage soft tissue surgical procedure. Facial morphology and dental occlusion. Scand J Plast Reconstr Surg. 1977;11:45–57. doi: 10.3109/02844317709025496. [DOI] [PubMed] [Google Scholar]
- 14.Ishii K, Vargervik K. Nasal growth in complete bilateral cleft lip and palate. J Craniofac Surg. 1996;7:290–6. doi: 10.1097/00001665-199607000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Hodgkinson PD, Rabey GP. Three-dimensional nasal morphology in adult bilateral cleft palate patients: A morphanalytic study. Br J Plast Surg. 1986;39:193–205. doi: 10.1016/0007-1226(86)90082-2. [DOI] [PubMed] [Google Scholar]
- 16.Winters JC, Hurwitz DJ. Presurgical orthopedics in the surgical management of unilateral cleft lip and palate. Plast Reconstr Surg. 1995;95:755–64. doi: 10.1097/00006534-199504000-00024. [DOI] [PubMed] [Google Scholar]
- 17.Rosenstein SW, Jacobson BN. Early maxillary orthopedics: A sequence of events. Cleft Palate J. 1967;4:197–204. [PubMed] [Google Scholar]
- 18.Latham RA. Orthopedic advancement of the cleft maxillary segment: A preliminary report. Cleft Palate J. 1980;17:227–33. [PubMed] [Google Scholar]
- 19.Huebener DV, Liu JR. Maxillary orthopedics. Clin Plast Surg. 1993;20:723–32. [PubMed] [Google Scholar]
- 20.LaRossa D. The state of the art in cleft palate surgery. Cleft Palate Craniofac J. 2000;37:225–8. doi: 10.1597/1545-1569_2000_037_0225_tsotai_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 21.Mulliken JB. Repair of bilateral complete cleft lip and nasal deformity: State of the art. Cleft Palate Craniofac J. 2000;37:342–7. doi: 10.1597/1545-1569_2000_037_0342_robccl_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 22.Hagerty RF, Andrews EB, Hill MJ, Calcote CE, Karesh SH, Lifeschiz JM, et al. Dental arch collapse in cleft palate. Plast Reconstr Surg. 1964;34:25–35. [Google Scholar]
- 23.Vargervik K. Morphologic evidence of muscle influence on dental arch width. Am J Orthod. 1979;76:21–8. doi: 10.1016/0002-9416(79)90296-3. [DOI] [PubMed] [Google Scholar]
- 24.Mishima K, Sugahara T, Mori Y, Sakuda M. Palatal configuration in complete bilateral cleft lip and palate infants before and after cheiloplasty. Cleft Palate Craniofac J. 1997;34:475–82. doi: 10.1597/1545-1569_1997_034_0475_pcicbc_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 25.Trier WC. Repair of bilateral cleft lip: Millard's technique. Clin Plast Surg. 1985;12:605–25. [PubMed] [Google Scholar]
- 26.Sillman JH. Dimensional changes of the dental arches: Longitudinal study from birth to 25 years. Am J Orthod. 1964;50:824–42. [Google Scholar]
- 27.Grayson BH, Santiago PE, Brecht LE, Cutting CB. Presurgical nasoalveolar molding in infants with cleft lip and palate. Cleft Palate Craniofac J. 1999;36:486–98. doi: 10.1597/1545-1569_1999_036_0486_pnmiiw_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 28.Ross RB, Johnston MC. The effect of early orthodontic treatment on facial growth in cleft lip and palate. Cleft Palate J. 1967;4:157–64. [PubMed] [Google Scholar]
- 29.Atherton JD. The natural history of the bilateral cleft. Angle Orthod. 1974;44:269–78. doi: 10.1043/0003-3219(1974)044<0269:TNHOTB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.King BF, Workman CH, Latham RA. An anatomical study of the columella and the protruding premaxillae in a bilateral cleft lip and palate infant. Cleft Palate J. 1979;16:223–9. [PubMed] [Google Scholar]
- 31.Friede H, Morgan P. Growth of the vomero-premaxillary suture in children with bilateral cleft lip and palate.A histological and roentgencephalometric study. Scand J Plast Reconstr Surg. 1976;10:45–55. doi: 10.1080/02844317609169745. [DOI] [PubMed] [Google Scholar]
- 32.Vargervik K. Growth characteristics in the premaxilla and orthodontic treatment principles in bilateral cleft lip and palate. Cleft Palate J. 1983;20:289–302. [PubMed] [Google Scholar]
- 33.Heidbuchel KL, Kuijpers-Jagtman AM, Kramer GJ, Prahl-Andersen B. Maxillary arch dimensions in bilateral cleft lip and palate from birth until four years of age in boys. Cleft Palate Craniofac J. 1998;35:233–9. doi: 10.1597/1545-1569_1998_035_0233_madibc_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 34.Latham RA. Development and structure of the premaxillary deformity in bilateral cleft lip and palate. Br J Plast Surg. 1973;26:1–11. doi: 10.1016/s0007-1226(73)80028-1. [DOI] [PubMed] [Google Scholar]
- 35.Noordhoff MS, Huang CS, Lo LJ. Median facial dysplasia in unilateral and bilateral cleft lip and palate: A subgroup of median cerebrofacial malformations. Plast Reconstr Surg. 1993;91:996–1007. [PubMed] [Google Scholar]
- 36.Allam KA, Wan DC, Kawamoto HK, Bradley JP, Sedano HO, Saied S. The spectrum of median craniofacial dysplasia. Plast Reconstr Surg. 2011;127:812–21. doi: 10.1097/PRS.0b013e318200aa08. [DOI] [PubMed] [Google Scholar]
- 37.da Silva Filho OG, Valladares Neto J, Capelloza Filho L, de Souza Freitas JA. Influence of lip repair on craniofacial morphology of patients with complete bilateral cleft lip and palate. Cleft Palate Craniofac J. 2003;40:144–53. doi: 10.1597/1545-1569_2003_040_0144_iolroc_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 38.Heidbuchel KL, Kuijpers-Jagtman AM. Maxillary and mandibular dental-arch dimensions and occlusion in bilateral cleft lip and palate patients form 3 to 17 years of age. Cleft Palate Craniofac J. 1997;34:21–6. doi: 10.1597/1545-1569_1997_034_0021_mamdad_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 39.Mulliken JB. Bilateral complete cleft lip and nasal deformity: An anthropometric analysis of staged to synchronous repair. Plast Reconstr Surg. 1995;96:9–26. [PubMed] [Google Scholar]
- 40.Kim SK, Lee JH, Lee KC, Park JM. Mulliken method of bilateral cleft lip repair: Anthropometric evaluation. Plast Reconstr Surg. 2005;116:1243–51. doi: 10.1097/01.prs.0000181518.97734.bf. [DOI] [PubMed] [Google Scholar]
- 41.Liao YF, Huang CS, Liou JW, Lin WY, Ko WC. Premaxillary size and craniofacial growth in patients with cleft lip and palate. Changgeng Yi Xue Za Zhi. 1998;21:391–6. [PubMed] [Google Scholar]
- 42.Liao YF, Huang CS, Tsai YY, Noordhoff MS. Craniofacial morphology in children with complete bilateral cleft lip and palate: Does infantile size of the premaxilla predetermine outcome? Cleft Palate Craniofac J. 2004;41:410–5. doi: 10.1597/03-021.1. [DOI] [PubMed] [Google Scholar]
- 43.Delaire J, Precious DS, Gordeef A. The Advantage of Wide Subperiosteal Exposure in Primary Surgical Correction of Labial Maxillary Clefts. Scand J Plast Reconstr Surg. 1988;22:147–51. doi: 10.3109/02844318809072387. [DOI] [PubMed] [Google Scholar]
- 44.Friede H, Pruzansky S. Longitudinal study of growth in bilateral cleft lip and palate, from infancy to adolescence. Plast Reconstr Surg. 1972;49:392–403. doi: 10.1097/00006534-197204000-00005. [DOI] [PubMed] [Google Scholar]
- 45.Handelman CS, Pruzansky S. Occlusion and dental profile with complete bilateral cleft lip and palate. Angle Orthod. 1968;38:185–98. doi: 10.1043/0003-3219(1968)038<0185:OADPWC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 46.Chen PK, Noordhoff MS, Liou EJ. Treatment of Complete Bilateral Cleft Lip-Nasal Deformity. Semin Plast Surg. 2005;19:329–42. [Google Scholar]
- 47.Perlyn CA, Brownstein JN, Huebener DV, Marsh JL, Nissen RJ, Pilgram T. Occlusal relationship in patients with bilateral cleft lip and palate during the mixed dentition stage: Does neonatal maxillary arch configuration predetermine outcome? Cleft Palate Craniofac J. 2002;39:317–32. doi: 10.1597/1545-1569_2002_039_0317_oripwb_2.0.co_2. [DOI] [PubMed] [Google Scholar]


