Abstract
Context:
In this prospective study, 13 randomly selected patients underwent treatment for zygomatic–complex fractures (2 site fractures) and mandibular fractures using 1.5 / 2 / 2.5-mm INION CPS biodegradable plates and screws.
Aims:
To assess the fixation of zygomatic-complex and mandibular fractures with biodegradable copolymer osteosynthesis system.
Materials and Methods:
In randomly selected 13 patients, zygomatic-complex and mandibular fractures were plated using resorbable plates and screws using Champy's principle. All the cases were evaluated clinically and radiologically for the type of fracture, need for the intermaxillary fixation (IMF) and its duration, duration of surgery, fixation at operation, state of reduction at operation, state of bone union after operation, anatomic reduction, paresthesia, occlusal discrepancies, soft tissue infection, immediate and late inflammatory reactions related to biodegradation process, and any need for the removal of the plates.
Statistical Analysis Used:
Descriptives, Frequencies, and Chi-square test were used.
Results:
In our study, the age group range was 5 to 55 years. Road traffic accidents accounted for the majority of patients six, (46.2%). Postoperative occlusal discrepancies were found in seven patients as mild to moderate, which resolved with IMF for 1-8 weeks. There were minimal complications seen and only as soft tissue infection.
Conclusions:
Use of biodegradable osteosynthesis system is a reliable alternative method for the fixation of zygomatic-complex and mandibular fractures. The biodegradable system still needs to be refined in material quality and handling to match the stability achieved with metal system. Biodegradable plates and screws is an ideal system for pediatric fractures with favorable outcome.
Keywords: Biodegradation, mandibular fractures, resorbable plates, zygomatic-complex
INTRODUCTION
The concept of using degradable materials for implants has been of interest for many years. Surgical suture is one of the earliest clinical implants in recorded history. Catgut suture, obtained from bovine intestinal submucosa, was known in 150 AD in the time of Galen, who treated wounded gladiators. The idea of using polyglycolic acid suture material for fracture fixation plates and screws was patented in 1973.[1]
The interest in the use of bioresorbable materials for internal fixation of fractured bones instead of traditionally applied metallic devices has been increasing since 1965.[2]
The use of polylactic acids (PLA) for the development of surgical implants started in 1966.[3] In 1966, it was reasoned that polylactic acid would be useful for degradable surgical implants.[1] The stabilization of mandibular fractures in dogs with PLA osteosynthesis plates and screws was reported for the first time in 1972. Since 1983, clinical applications of biodegradable osteosynthesis materials were performed in pilot studies.[3]
Aims and objectives of the study
To assess the fixation of zygomatic-complex and mandibular fractures with biodegradable copolymer osteosynthesis system.
To assess the outcome of patients with zygomatic-complex and mandibular fractures that are stabilized with resorbable plates and screws.
To assess stability of fixation of resorbable plates intraoperatively.
To assess postoperative complications with use of resorbable plates and screws.
MATERIALS AND METHODS
In this prospective study, 13 randomly selected patients underwent treatment for zygomatic-complex fractures (2 site fractures) and mandibular fractures using 1.5/2/2.5-mm INION CPS biodegradable plates and screws.
The period of study was from January 2009 to October 2010.
-
(a)
Assessment plan - preoperative, intraoperative, 1st postoperative day, 3rd postoperative day, 6 weeks postoperatively, 3 months postoperatively, and 6 months postoperatively.
-
(b)
Assessment was made with relevant radiographs (Paranasal sinus (PNS), Submentovertex (SMV), Orthopantomogram (OPG) radiographs) and Ultrasonography (USG) imaging of operated site for monitoring resorption-3 months, 6 months, and 1 year postoperatively.
Inclusion criteria
Patients of age group 5 to 55 years.
A dentition complete enough to apply stable Erich arch bars for intermaxillary fixation (IMF) placement.
Non-infected fracture site.
Exclusion criteria
Comminuted fractures.
Simultaneous use of biodegradable and metallic material.
Patients in whom IMF is medically contraindicated (epilepsy, severe asthma, psychiatric condition, and alcohol or drug abuse).
Patients with systemic bone diseases.
If associated with condylar, intracapsular, and coronoid fractures.
The number of days from the injury to operation, average age, gender, American Society of Anaesthesiologists (ASA) classification, and social habits were all recorded. All the subjects received intravenous antibiotics from the time of admission until discharge. Following this, a 5-day course of oral antibiotics were prescribed. Antibiotic dosage for children was calculated depending on age and weight of the child.
In this study, five zygomatic-complex fractures (fronto-zygomatic and zygomatic buttress sites) and eight mandibular fractures were treated, in which patients had five zygomatic-complex, seven Parasymphysis, and one angle fractures. Two patients had associated undisplaced Angle and zygomatic-complex with zygomatic arch fracture. Plates were placed along the Champy's ideal line of osteosynthesis in mandibular fractures. All cases have been followed up for minimum of 6 months and maximum of 1½ years.
Mandibular fractures were reduced with upper and lower Erich's arch bar fixation as a means for IMF intraoperatively. All arch bars were removed 1 to 8 weeks postoperatively. All the patients were operated under general anesthesia following routine laboratory hematological, biochemical investigations, physician's clearance, and routine radiological examination.
All cases have been evaluated clinically and radiologically for the following parameters:
Duration of surgery: Was limited to the operating time.
Need for the intermaxillary fixation and its duration (postoperatively): Cases with mild to moderate occlusal discrepancy were postoperatively put on IMF.
-
Fixation at operation:
Excellent : No movement of plate or bone fragment.
Good : Slight movement of plate but no movement of bone fragment
Acceptable : Movement of bone fragment but no need for other internal fixation
Poor : Movement of fragment and need for other internal fixation
-
State of reduction at operation:
Excellent : No gap between bone fragments
Good : Less than 1 mm gap between bone fragments
Acceptable : Over 1 mm but less than 5 mm gap between bone fragments
Poor : Over 5 mm gap or step between bone fragments
-
State of bone union after operation:
Excellent : Very satisfactory
Good : Satisfactory
Acceptable : No need for treatment
Poor : Need for treatment
-
Occlusal discrepancies: The changes in occlusion over the four weeks were noted. The occlusion was scored as follows:
- Normal occlusion/functional occlusion.
- Moderate derangement – reasonable but not exact contact bilaterally.
- Gross derangement – no contact or contact in one or two teeth or open bite.
-
Anatomic reduction: Assessed with postoperative Paranasalsinus, Submentovertex, and Orthopantomogram radiographs. The fracture was assessed radiographically and was divided into the following:
Excellent : No visible radiographic gap between fracture fragments postoperatively
Good : Less than 5 mm of visible radiographic gap between fracture fragments postoperatively
Fair : More than 5 mm of visible radiographic gap between fracture fragments postoperatively
Non-union and delayed union: Assessed by excessive mobility at the operated site 4 weeks postoperatively.
Paresthesia/Neurosensory changes (preoperative and postoperative): The results of each test were compared with those obtained from the normal (unoperated/uninjured) side both pre- and postoperatively using light touch method and brush directional method.
Infection at the fracture site: Assessed by any swelling, pain, tenderness, wound dehiscence, or pus discharge at the operated site.
Mild to Moderate infection – managed with postoperative antibiotic therapy and/or incision and drainage. Severe/recurrent infection – managed with antibiotic therapy and part of plate removal under local anaesthesia (exposed part only). Any need for the removal of part of plate in case of severe or recurrent infection at the fracture site was managed with antibiotic therapy and plate removal was scored as:
No
Yes
Inflammatory reactions related to biodegradation process- immediate and late reactions: Early reactions such as inflammation, erythema, local swelling, and tenderness were assessed.
Late/delayed reactions (>3 months from the time of operation) such as localized recurrent swelling, suddenly emerging painful, erythematous, fluctuating papule which reveals a sinus discharge of liquid remnants of disintegrated implant materials, osteolytic changes around the implanted material seen in radiographs were assessed.
Surgical technique
All cases were treated under general anesthesia with naso-tracheal intubation. Face was painted with povidone-iodine followed by spirit. The oral cavity was prepared with diluted povidone-iodine. Towels and drapes were applied to expose the surgical area. Local infiltration at the fracture site was done using 2% lignocaine with 1:80 000 adrenaline for vasoconstriction.
For Fronto-Zygomatic (F-Z) region fractures, lateral eyebrow or blepharoplasty incision was used.
For Zygomatic buttress fractures, intraoral upper buccal vestibular incision was used corresponding to the involved side.
For Mandibular fractures, a lower vestibular incision was used in labio buccal sulcus corresponding to the involved site.
For Zygomatic-Complex fractures, blunt dissection was done in layers at F-Z region and mucoperiosteal flap raised in buttress region to expose the fracture site. Great care was taken not to damage the infraorbital nerve. Open reduction was done, fracture segments were reduced.
In case of mandibular fractures, mucoperiosteal flap was raised to expose the fracture site till the lower border of the mandible. Open reduction was done and fracture segments were reduced. Occlusion was established with maxillomandibular fixation. First lower plate was adopted and fixed and then the upper plate was fixed. In case of angle fractures, a single plate was adopted along the external oblique ridge. Care was taken not to injure the inferior alveolar and mental nerves. The occlusion was checked and screws tightened finally.
The resorbable plates were first preactivated in thermo water bath at 55°C for 1-2 minutes, contoured to the desired shape required, and then adapted against the bone segment. Plates are malleable for 10-15 seconds and then they can be reheated for further contouring or cut once cooled. Screw holes were drilled according to the size of the plate used using the corresponding drillbit attached to the handpiece and micromotor with constant saline irrigation. The drilled holes were then manually tapped and screw placement was done using a universal screw driver till a snug fit was achieved. In case of fracture of screw head during placement, the screw hole was redrilled and tapped and screw placed. In our study, overall six screw heads were fractured due to over-tightening of the screws and managed with emergency screws. A transbuccal trocar was used for plating in case of mandibular angle fractures.
The extraoral sites were closed using vicryl 3-0 and prolene 4-0. Intraoral sites were closed using vicryl 3-0. An extraoral pressure bandage was applied. Patients were advised to take liquid diet for a day and thereafter on a soft diet for 2 weeks. Occlusion was checked in case of mandibular fractures on the 1st postoperative day, 3rd postoperative day, and on subsequent visits, and complications were recorded if any.
RESULTS
In our study, the minimum age of the patient was 5 years and maximum was 55 years, with a mean age of 24.7 years. All the patients were males and there were no females in the study. There were no patients in the age group of 36 to 45 years in the study. Etiologies for the fractures in this study included road traffic accident seen in six (46.2%) patients, followed by accidental fall seen in four (30.8%) patients, assault and work-related injuries. In all patients, fixation was assessed intraoperatively and eight patients had excellent results (61.5%) while five patients had good results (38.5%). In the study, state of reduction was assessed intraoperatively and eight (61.5%) patients had good results. In all the patients, state of bone union after operation and anatomic reduction was assessed by preoperative and postoperative radiographs. Eight patients had excellent bone union (61.5%) after surgery and rest showed good results (38.5%). Anatomic reduction was excellent in 53.8% patients and good in remaining 46.2% of patients. Postoperatively, seven patients (53.8%) had mild to moderate occlusal derangement and in patients with occlusal derangement, IMF was done using elastics or tie wires for 1 to 2 weeks followed by guiding elastics if necessary for 1 week. IMF was required for 2 weeks in four patients (30.8%), 3 weeks in two patients (15.4%), and 8 weeks in only one patient (7.7%). Age group of 5 to 15 years and zygomatic-complex fractures without occlusal derangement did not require IMF in the study. Temporary paresthesia was noted to be present in three patients (23.1%) both preoperatively and postoperatively. Paresthesia improved over 8 weeks in two patients and over 2 weeks in another patient. The other ten patients (76.9%) had no neurosensory changes. In the study, soft tissue infection was seen in three patients (23.1%) having mandibular fractures postoperatively due to poor oral hygiene maintenance, which was managed conservatively with antibiotics. Rest of the ten patients (76.9%) had satisfactory healing of wounds.
None of the patients had non-union, immediate, or late inflammatory reactions to resorbable plates and screws after surgery, any signs of recurrent infection, sinus discharge of remnants of implants, any osteolytic changes or any exposure of plates, and need for removal of part of exposed plate. In the study, the complication rate was minimal with only soft tissue infection managed conservatively with antibiotics.
DISCUSSION
Persistent attempts have been made to develop modalities that can minimize complications by fixing the bone fragments after fracture or osteotomy and induce solid bone union with stabilized fixation. The requirements for such a bone fixation device include sufficient strength and rigidity to induce bony union, the absence of a tendency to produce a foreign body reaction or infection within the body, no interference with the bony union, an inability to be palpated or visualized and spontaneous absorption.[4]
The aim of fracture management is to obtain a bone function as close to the pre-fracture state as possible. Absolute stability is the main criteria of fixation which aids in direct bone healing.[5] The use of metal system, i.e., stainless steel and titanium to stabilize facial fractures, is well documented and has stood the test of time. However, they had problems like palpability or visibility of the plate, sensitivity to temperature, metal allergy, secondary infection or bone resorption, possibility of interference with postoperative radiologic assessments, loosening of plates and screws, pain, wound dehiscence, restriction of bone growth in children, and requirement for second surgery in case of repeated infections.[4,6]
These led to the development of biodegradable hardware that was strong, biocompatible, adaptable, small, and provides enough stability to allow fracture healing and then resorb quickly without any foreign body reaction. Since their modulus of elasticity simulates bone, stress shielding effect is not a feature. Due to slow resorption, they transfer stresses slowly to bone preventing osteoporosis. These polymers can be broken down naturally by metabolic system. Bioresorbable polymer science has evolved significantly in the last 20 years and each product is unique in terms of its polymer formulas, manufacturing technique, and handling characteristics, all of which influence strength and workability.[6,7]
Use of biodegradable materials in pediatric craniofacial surgery has been favorable and also used in orthognathic surgery. The 70/30 poly-L/DL-lactide plates and screws are biocompatible in growing patients with facial fractures. Mandible fractures involving small children in the primary or mixed dentition may be readily stabilized with plates and screws placed at the inferior border. Because the hardware resorbs, there is no long-term effect on skeletal growth or tooth development.[6] The disadvantages of the resorbable plates and screws are—they are larger and weaker than their titanium counterparts, they require a heating source to facilitate bending, the working time is limited, and the screws are not self tapping. These properties make them less attractive for use in patients with complex panfacial injuries, severe displacement, and comminuted fractures. In addition, the thin bone of maxilla and medial orbit makes it ill-suited for tapping.[6]
Biodegradation of polylactides starts in the center, a slowly degrading outer layer stays intact and retains degradation products until the swelling of the implants causes it to break. After disruption of the outer layer, the released lactic acid will further disintegrate into CO2 and H2O by the tricarboxylate cycle.[3] The implant slowly disappears while fibrous tissue or bone fills the volume formerly occupied by the implant.[7] Biodegradable plates can be shaped easily by digital pressure once it becomes malleable after immersion in the water bath. These plates are radiolucent and do not interfere with computed tomographic or magnetic resonance imaging and they allow a clear postoperative view of fracture site on plain radiographs.[8]
Ultrasound imaging of biodegradable osteosynthesis materials was first published by Kimmel after in vitro tests. In Figure 1, the outer border of the plate is precisely limited as hyperdense structure in comparison to the hypodense center. Degradation starts with water intake producing increase in distance between the hyperdense outer borders with breaks in the lines [Figure 2]. In Figure 3, the maximum of volume increase is reached; a hypodense structure is seen at the implantation site of the plate. At the end of the degradation process, only a thin hypodense area is visible [Figure 3]. The length and thickness of the osteosynthesis plates can be easily measured during the ultrasound examination.[3]
Figure 1.
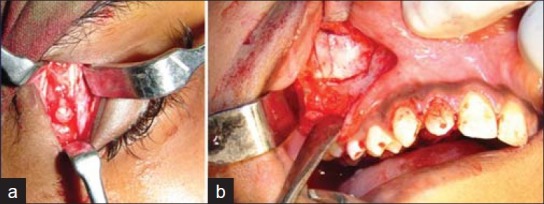
(a) Intraoperative view of resorbable plates and screws at right F-Z region of case no. 1, (b) Intraoperative view of resorbable plates and screws at right zygomatic buttress region of case no 1
Figure 2.
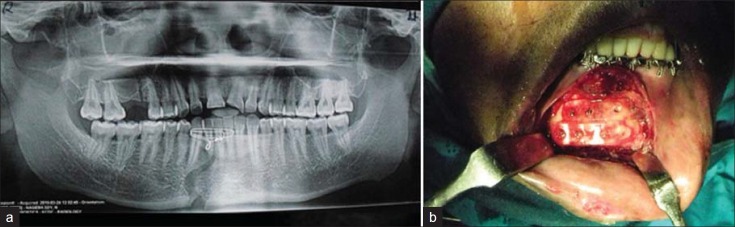
(a) Preoperative OPG radiograph of case no. 2, (b) Intraoperative view of resorbable plates and screws of case no 2
Figure 3.
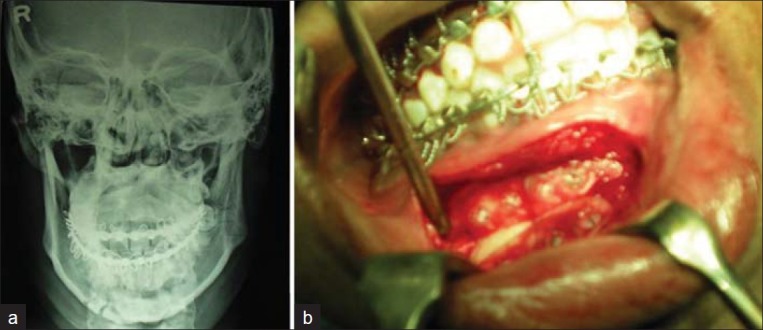
(a) Preoperative postero-anterior mandible radiograph of case no. 3, (b) Intraoperative view of resorbable plates and screws of case no. 3
Figure 1.
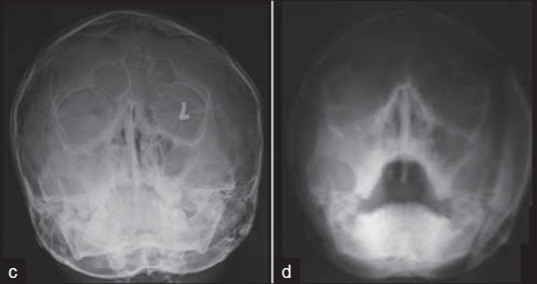
(c) Preoperative PNS radiograph of case no. 1, (d) Postoperative PNS radiograph of case no 1
Figure 1.
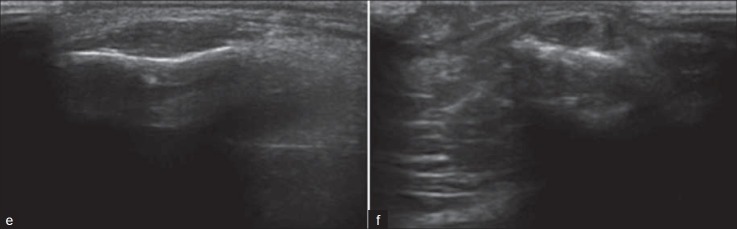
(e) 22 months postoperative USG at F-Z region showing thin hypodense part of remaining plate of case no. 1, (f) 22 months postoperative USG at Zygomatic buttress region showing thin hypodense part of remaining plate of case no 1
Figure 2.
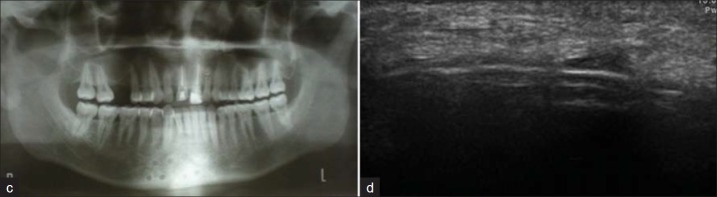
(c) Postoperative OPG radiograph of case no. 2, (d) 9 months postoperative USG showing thin hypodense structure suggestive of resorption of plates of case no 2
Figure 3.
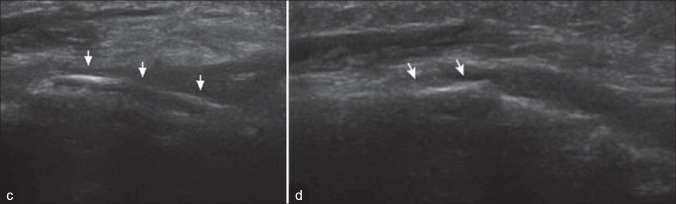
(c) 9 months postoperative USG showing changes in length and discontinuity of plates seen, (d) 18 months postoperative USG showing thin hypodense part of remaining plate suggestive of resorption of case no 3
Figure 3e.

Postoperative OPG radiograph of case no 3
In a study done to evaluate fixation of mandibular fractures with biodegradable plates and screws, ossification of the fracture was seen after 3 months and screw holes were seen as radiolucent areas in the radiologic analysis.[9]
The incidence of malocclusion reported by Champy, et al. in their 183 cases was 0.5%. The incidence of malocclusion with resorbable fixation has been 0% to 2.4%. In a study conducted by Krishna Bhatt, et al., 11% malocclusion was seen in resorbable group, i.e., in two patients.[10] In a study done to evaluate self-reinforced biodegradable plates and screws for fixation of zygomatic fractures, of 25 patients, two patients were found to have local infection with swelling in upper oral vestibule in early postoperative period and were managed by antibiotics, incision, and drainage.[11]
In children, the frequent absence of teeth due to primary teeth exfoliation and the poor retentive shape of deciduous teeth crowns make the traditional use of arch bars and interdental ligatures impossible to apply. Several methods proposed to immobilize mandible in children include the use of acrylic splints and combined circummandibular and transnasal wiring. The length of mandibular immobilization may be shorter.[12]
Bergsma, et al. suggested that the local tissue tolerance and transport potential, in relation to the possibly high amount of polymeric debris formation of the relatively fast-degrading polyglycolide, influences the development of a clinically manifested reaction.[13]
The quantity, degradation characteristics, and associated changes in morphology of the implanted material as well as the characteristics of the tissue in which the material is implanted are entities that may influence the intensity of the tissue reaction. Perhaps, a combination of these factors may account for the clinically manifested foreign body reaction to the high-molecular-weight PLA bone plates and screws.[13]
CONCLUSION
From the study it is suggested that biodegradable osteosynthesis system fulfilled the treatment goals of adequate immobilization, fixation, and stabilization of zygomatic-complex and mandibular fractures. Though the stability of the fractured fragments and handling characteristics of the system were comparable with the metal system, biodegradable system has its own advantages like avoidance of second surgery due to resorption, less interference in craniofacial growth in children, less interference with computed tomographic or magnetic resonance imaging, etc.
The use of biodegradable osteosynthesis system is a reliable alternative method for the open reduction and internal fixation of zygomatic-complex and mandibular fractures. The surgeon must choose the type of fixation and method of placement, taking into account the location of fracture and ease of placement of screws. The biodegradable system still needs to be refined in material quality and handling to maximize the strength and match the stability achieved with metal system. Biodegradable plates and screws is an ideal system for pediatric fractures with favorable outcome. Experimental and clinical success in craniofacial, orthognathic, and trauma surgery is the stimulus for further research and development.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Barrows TH. Degradation implant materials: A review of synthetic absorbable polymers and their applications. Clin Mater. 1986;1:233–57. [Google Scholar]
- 2.Leenslag JW, Pennings AJ, Bos RM, Rozema FR, Boering G. Resorbable materials of poly (L-lactide), In vivo and In vitro degradation. Biomaterials. 1987;8:311–4. doi: 10.1016/0142-9612(87)90121-9. [DOI] [PubMed] [Google Scholar]
- 3.Heidemann W, Gerlach KL. Imaging of biodegradable osteosynthesis materials by ultrasound. Dentomaxillofac Radiol. 2002;31:155–8. doi: 10.1038/sj/dmfr/4600667. [DOI] [PubMed] [Google Scholar]
- 4.Lee HB, Oh JS, Kim SG, Kim HK, Moon SY, Kim YK, et al. Comparison of Titanium and Biodegradable Miniplates for Fixation of Mandibular Fractures. J Oral Maxillofac Surg. 2010;68:2065–9. doi: 10.1016/j.joms.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Menon S, Chowdhury SK. Evaluation of bioresorbable Vis-à-vis titanium plates and Screws for craniofacial fractures and osteotomies. MJAFI. 2007;63:331–3. doi: 10.1016/S0377-1237(07)80008-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bell BR, Kindsfater CS. The use of biodegradable plates and screws to stabilize facial fractures. J Oral Maxillofac Surg. 2006;64:31–9. doi: 10.1016/j.joms.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 7.Enislidis G, Pichorner S, Lambert F, Wagner A, Kainberger F, Kautzky M, et al. Fixation of Zygomatic fractures with a new biodegradable copolymer osteosynthesis system. Preliminary results. Int J Oral Maxillofac Surg. 1998;27:352–5. doi: 10.1016/s0901-5027(98)80063-5. [DOI] [PubMed] [Google Scholar]
- 8.Wood GD. Inion biodegradable plates: The first century. Br J Oral Maxillofac Surg. 2006;44:38–41. doi: 10.1016/j.bjoms.2005.07.026. [DOI] [PubMed] [Google Scholar]
- 9.Peterson LJ. Fixation of mandibular fractures with biodegradable plates and screws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:294–300. doi: 10.1067/moe.2002.122833. [DOI] [PubMed] [Google Scholar]
- 10.Bhatt K, Roychoudhury A, Bhutia O, Trikha A, Seith A, Pandey RM. Equivalence Randomized Controlled Trial of Bioresorbable Versus Titanium Miniplates in Treatment of Mandibular Fracture: A Pilot Study. J Oral Maxillofac Surg. 2010;68:1842–8. doi: 10.1016/j.joms.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 11.Enislidis G, Yerit K, Wittwer G, Kohnke R, Schragl S, Ewers R. Self-reinforced biodegradable plates and screws for fixation of zygomatic fractures. J Cranio-Maxillofac Surg. 2005;33:95–102. doi: 10.1016/j.jcms.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 12.Eppley BL. Use of Resorbable Plates and Screw in Pediatric Facial Fractures. J Oral Maxillofac Surg. 2005;63:385–91. doi: 10.1016/j.joms.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 13.Bergsma EJ, Rozema FR, Bos RM, Bruijn WC. Foreign Body Reactions to Resorbable Poly (L-lactide) Bone Plates and Screws Used for the Fixation of Unstable Zygomatic Fractures. J Oral Maxillofac Surg. 1993;51:666–70. doi: 10.1016/s0278-2391(10)80267-8. [DOI] [PubMed] [Google Scholar]


