Description
A 44-year-old man presented with progressive limb girdle weakness from 10 years of age. The inheritance pattern was autosomal dominant; two siblings, his mother and maternal grandfather were similarly affected. On examination there was an exaggerated lumbar lordosis, wasting of proximal limb musculature, and contractures at elbows, wrists and finger flexors. There was moderate symmetrical proximal upper and lower limb weakness without facial weakness or cardiorespiratory involvement. Previous investigations included electromyography which was myopathic, creatine kinase 2–4× normal and dystrophic muscle biopsy but no definitive diagnosis had been made.
The differential diagnosis is of a collagen VI myopathy (Bethlem), laminopathy or limb girdle muscular dystrophy. This differential diagnosis can be narrowed with lower limb muscle MRI1 which was performed. The pattern (figure 1) was typical of Bethlem myopathy. The muscle biopsy was sent for further analysis which showed marked reduction of collagen VI at the basal lamina of most fibres. Subsequent genetic studies identified a heterozygous missense mutation in COL6A2.
Figure 1.
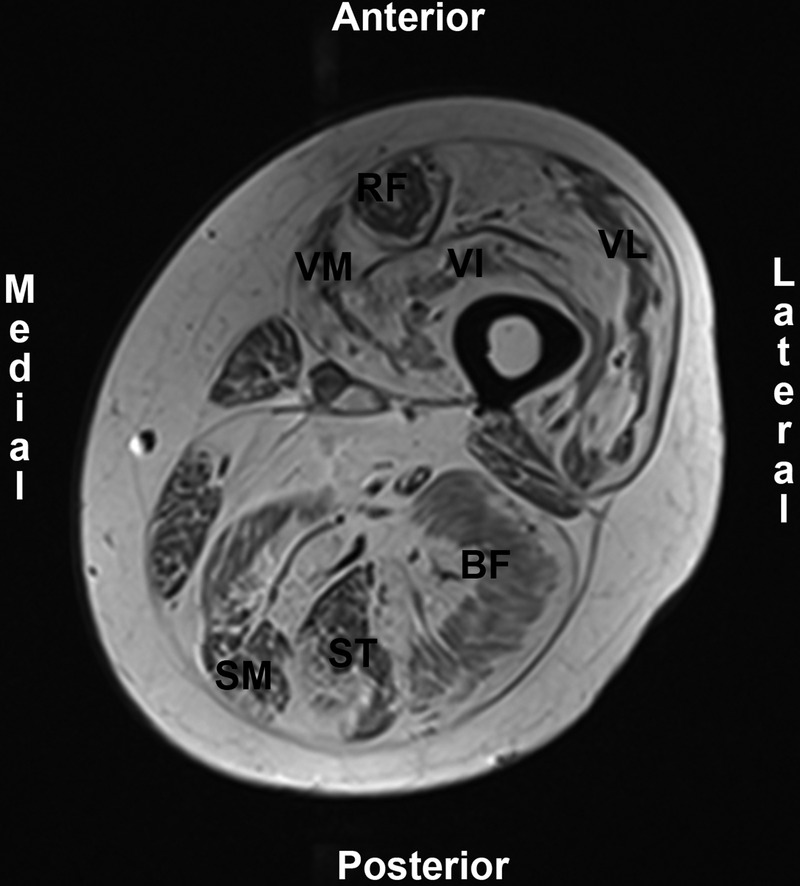
T1-weighted MRI, transverse slice at mid left thigh. Normal muscle has low-signal intensity, fat has high-signal intensity. The quadriceps muscle shows the typical pattern for Bethlem myopathy: peripheral fat infiltration with central sparing of the vasti muscles (VM, vastus medialis; VI, vastus intermedius; VL, vastus lateralis) and both peripheral and anterocentral infiltration of rectus femoris (RF) leaving a ‘U’ shape of less-affected muscle. Central sparing of the hamstring muscles (BF, biceps femoris; ST, semitendinosus; SM, semimembranous) is also apparent.
Bethlem myopathy is the mild end of the collagen-VI-related myopathy spectrum. Although symptoms start in childhood, ambulation is typically maintained into adulthood. Contractures and mildly elevated creatine kinase are also typical.2 Bethlem myopathy has a highly specific pattern of muscle involvement on imaging with 90% sensitivity.1 3 The peripheral involvement of the vasti muscles and anterocentral involvement of rectus femoris1–3 is particularly striking and once seen easily recognised subsequently, facilitating definitive genetic diagnosis.
Learning points.
Consider Bethlem myopathy in adults with progressive myopathy and contractures.
A highly specific pattern of muscle involvement may be seen on lower limb MRI in Bethlem myopathy and guide definitive genetic testing.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Mercuri E, Clements E, Offiah A, et al. Muscle magnetic resonance imaging involvement in muscular dystrophies with rigidity of the spine. Ann Neurol 2010;2013:201–8 [DOI] [PubMed] [Google Scholar]
- 2.Mercuri E, Lampe A, Allsop J, et al. Muscle MRI in Ullrich congenital muscular dystrophy and Bethlem myopathy. Neuromuscul Disord 2005;2013:303–10 [DOI] [PubMed] [Google Scholar]
- 3.Ten Dam L,, van Der Kooi AJ,, van Wattigen M, et al. Reliability and accuracy of skeletal muscle imaging in limb-girdle muscular dystrophies. Neurology 2012;2013:1716–23 [DOI] [PubMed] [Google Scholar]


