Abstract
The medical management of a patient with Crohn's disease should take into account the activity, site and behaviour of disease, and should be discussed with the patient, and 5-aminosalicylates are a group of medications which have been commonly used. Sulfasalazine is a combination of 5-aminosalicylic acid and sulfapyridine which acts only as a carrier to the colonic site of action but can still cause systemic side-effects1 including lung disease. In mesalazine the specific sulfapyridine-related side-effects, especially pulmonary reactions, are avoided. However, we present a case of lung fibrosis which was associated with mesalazine in a Crohn's patient.
Background
Crohn's disease is a chronic inflammatory gastrointestinal disease characterised by transmural granulomatous inflammation. It may affect any part of the gut from mouth to anus, but favours the terminal ileum (in 50%) and proximal colon.
Drug therapy has been a mainstay in the management of Crohn's disease and the appropriate choice of medication is influenced by weighing benefits against potential side-effects; previous response to treatment and the presence of extraintestinal manifestations or complications. Aminosalicylates have been commonly used in mild-to-moderate Crohn's disease since early days. Serious side-effects were faced with sulfasalazine, so the newer sulfapyridine-free agents were introduced, such as mesalazine and olsalazine. Randomised controlled trials were conducted to test the efficacy of those drugs, and these trials yielded conflicting results. Here, we discovered that serious side-effects similar to those of sulfasalazine can also be faced with these agents, as with lung fibrosis secondary to mesalazine.
Case presentation
An 82-year-old man whose Crohn's disease was diagnosed in 1964, and led to pan-proctocolectomy and ileostomy, thereafter he received no maintenance treatment for Crohn's disease. More recently he had intermittent flare-ups of pain, diarrhoea and subacute bowels obstruction, which were initially managed conservatively. In the last few years the flare-ups became more frequent and occasionally led to hospital admissions. They involved the small bowels, mainly distal ileum and the ileostomy itself as shown on a CT of his abdomen. As a result he was referred back to the Gastroenterology team for further management.
His medical history includes osteoarthritis and hypertension.
He does not smoke, used to drink to excess with intermittent pancreatitis but recent alcohol intake is minimal. He lives alone independently and tends an allotment.
Following the most recent flare-up he was discharged from the surgical team with a reducing regime of prednisolone and when seen in the gastroenterology clinic he was in remission while taking prednisolone 10 mg daily. His thiopurine methyltransferase was checked with a view to starting azathioprine, but in the meantime he started pentasa (mesalazine) 1 g three times a day as a steroid sparing agent.
Nine days following mesalazine, the patient was admitted to the emergency department with severe dyspnoea.
On admission he was hypothermic with a temperature of 34.3°C, hypoxic with arterial blood gas showing a pH of 7.293, pCO2 of 4.09, pO2 of 4.98 and a base excess of –10.7 while breathing 10 litres of oxygen via a non-rebreathing mask. His troponin was raised, ECG showed atrial fibrillation with fast ventricular response and he was hypotensive with a blood pressure of 74/54 mm Hg. The cardiologist on duty was called to see him who started treatment with Digoxin.
His C reactive protein (CRP) was 136.2, a chest x-ray (CXR) showed consolidation on the right side with pleural effusion. He had impaired renal function with urea 16.7 and creatinine 264, both significantly raised above his baseline values.
He was transferred to a high-dependency unit (HDU) for high flow oxygen and continuous positive airway pressure therapy.
The provisional diagnosis was of a community acquired pneumonia with acute kidney injury, and he was treated with antibiotics and fluid resuscitation.
Subsequent CXRs showed deterioration of the consolidation and the pleural effusion, extending to the left lung.
Blood samples were sent for culture, atypical serology, urine was sent for Legionella, sputum for cultures and throat swabs for virology.
He was administered with antifungals besides antibiotics as empirical treatment, and steroids were continued in the form of intravenous hydrocortisone.
His sputum culture showed moderate growth of candida and was given fluconazole, and antibiotics were continued in the light of microbiology advice; unfortunately, the patient continued to deteriorate
Investigations
A high resolution CT thorax (figure 1) was requested which showed some ground glass changes in the lungs parenchyma consistent with among others lung fibrosis or atypical infection. As a result additional tests were sent off, mainly induced sputum for India Ink stain, Pneumocystis jerovecii (PCJ) immunofluorescence and PCR, cytomegalovirus (CMV) PCR, more fungal cultures and tuberculosis culture, as well as blood samples were sent for vasculitis screen. He was treated as PCJ empirically.
Figure 1.
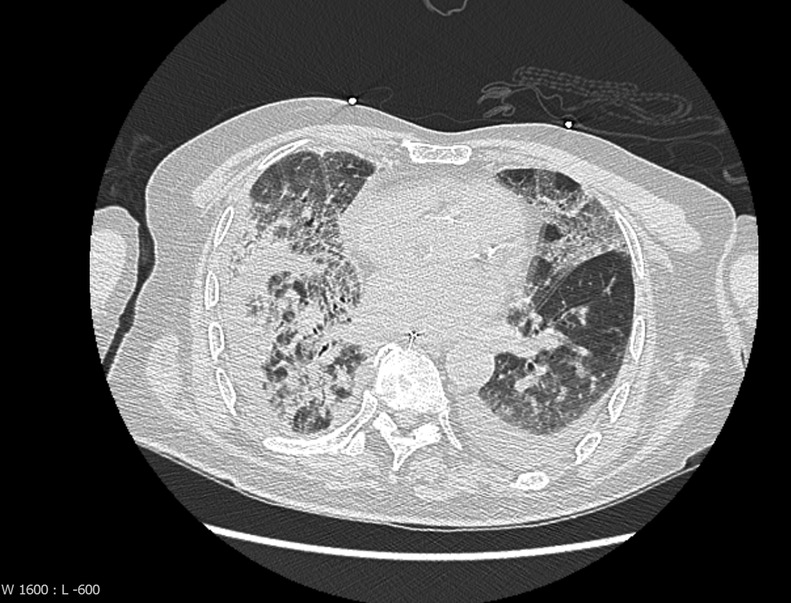
High-resolution CT thorax while on mesalazine.
Results came back as weakly positive for antineutrophil cytoplasmic antibody (ANCA) and CMV PCR, and there was a debate about how significant they were. However he was treated with antivirals after discussion with the virologists; meanwhile, he was having oral prednisolone instead of intravenous hydrocortisone.
Regardless of all the interventions mentioned, our patient continued to deteriorate, and all other tests came back as neutral.
Given the ambiguity of the aetiology in this case, the medical history of our patient was investigated carefully looking for any history of radiation, relevant occupational history, family history and more importantly his drug history. Here we learnt that the patient was started on mesalazine recently for his Crohn's symptoms and after the medical literature review we discovered a few case reports of mesalazine-induced lung disease.
Treatment
At this point it was decided to discontinue this medication and immediately place the patient on intravenous methylprednisolone followed by a high dose of oral prednisolone.
Outcome and follow-up
Within a few days our patient improved dramatically. He was weaned off non-invasive ventilation and was discharged to a respiratory ward, his CRP went down to 5 (figure 2), his creatinine was 121 and his urea was 7.2.
Figure 2.
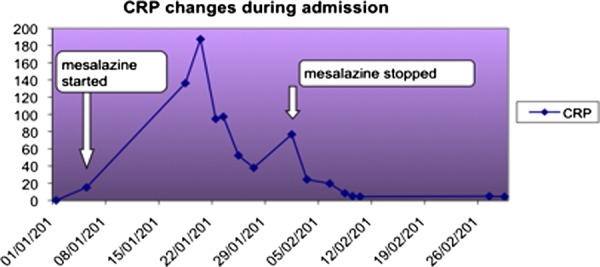
C reactive protein changes in relation to mesalazine.
Subsequently having left HDU to recuperate on the ward he had non-ST-segment elevation myocardial infarction, Norovirus diarrhoea and further acute kidney injury but was eventually discharged home with a full package of care due to poor mobility.
He was seen in the chest clinic 6 weeks after discharge, still short of breath and was in a wheelchair with oxygen saturation of 85% on room air. However repeat high-resolution CT (figure 3) showed much improvement. Spirometry showed a restrictive defect.
Figure 3.
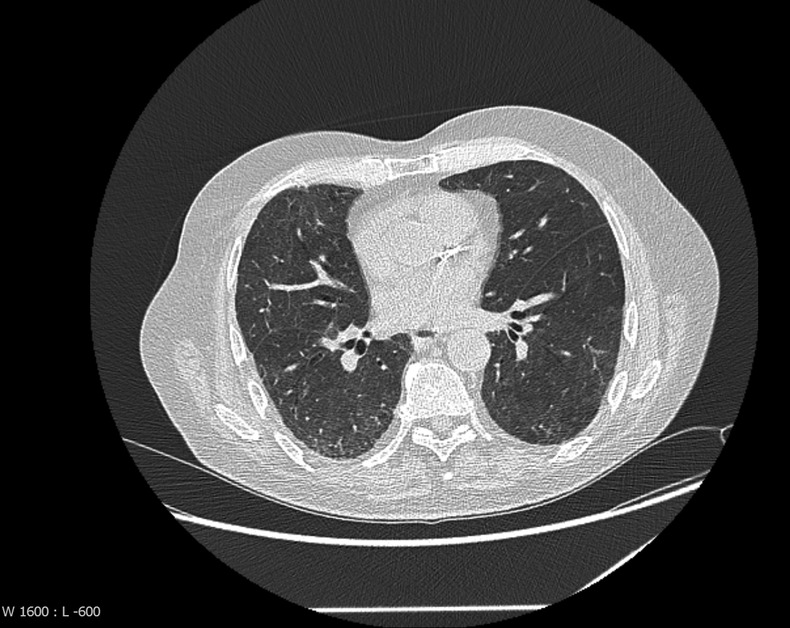
High-resolution CT thorax after discontinuation of mesalazine.
Discussion
The use of aminosalicylates in mild to moderate Crohn's disease was based on large controlled trials from the 1970s and the 1980s. However, a recent meta-analysis of the three placebo-controlled trials of Pentasa (a time dependent delayed release formulation of mesalazine) for active Crohn's disease demonstrated a statistically significant (p=0.04), but a non-clinically relevant deference in Crohn's Disease Activity Index, benefit of 18 points compared with placebo.2
Consequently, mesalazine should be considered clinically no more effective than placebo for active ileal or colonic Crohn's disease. This was reflected in the latest guidelines from the American College of Gastroenterology and European Crohn's and Colitis Organisation.
Interstitial lung disease includes a wide variety of conditions that individually are uncommon. There are more than 100 known causes of interstitial lung disease, and these include familial and genetic disorders, inhaled substances, infections, medications and connective tissue disease.
There are more than 380 drugs that are known to cause pulmonary toxicity.3 4
The incidence of interstitial lung disease from inflammatory bowel disease is unknown; however, there is evidence that more than 50% of patients with ulcerative colitis and Crohn's disease have pulmonary function impairment without clinical or radiographic findings.5
Respiratory complications attributed to IBD that are not related to medications have also been noted. Camus et al6 reviewed IBD-associated lung diseases and grouped them into categories of airway disease, interstitial disease, necrobiotic parenchymal nodules and serositis.
In patients treated with sulfasalazine or mesalazine, lung disease can develop as a reaction to one of these medications. Pulmonary toxicity was infrequent with sulfasalazine, but over the last decade, reports from mesalazine-induced lung disease have increased and the pathogenesis still unknown.
Corticosteroids therapy can lead to rapid recovery. However several reports also describe full recovery after discontinuation of mesalazine without steroids therapy.7 8
Learning points.
Mesalazine should be considered clinically no more effective than placebo for active ileal or colonic Crohn's disease.
Mesalazine should be considered seriously as a potential cause for any presentation of lung disease in a Crohn's patient.
In mesalazine-induced lung disease full recovery can occur after withdrawal of mesalazine without other interventions.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Cullen G, Vaughn B, Ahmed A, et al. Abdominal phlegmons in Crohn's disease: outcomes following antitumor necrosis factor therapy. Inflamm Bowel Dis 2012;2013:691–6 [DOI] [PubMed] [Google Scholar]
- 2.Hanauer SB, Stromberg U. Oral Pentasa in the treatment of active Crohn's disease: a meta-analysis of double-blind, placebo-controlled trials. Clin GastroenterolHepatol 2004;2013:379–88 [DOI] [PubMed] [Google Scholar]
- 3.Camus P, Rosenow EC., III Iatrogenic lung disease. ClinChest Med 2004;2013:XIII–XIX [DOI] [PubMed] [Google Scholar]
- 4.Flieder DB, Travis WD. Pathologic characteristics of drug-induced lung disease. Clin Chest Med 2004;2013:37–45 [DOI] [PubMed] [Google Scholar]
- 5.Kuzela L, Vavrecka A, Prikazska M, et al. Pulmonary complications in patients with inflammatory bowel disease. Hepato-gastroenterology 1999;2013:1714–19 [PubMed] [Google Scholar]
- 6.Camus P, Piard F, Ashcroft T, et al. Colby TV. The lung in inflammatory bowel disease. Medicine 1993;2013:151–83 [PubMed] [Google Scholar]
- 7.Reinoso MA, Schroeder KW, Pisani RJ. Lung disease associated with orally administered mesalamine for ulcerative colitis. Chest 1992;2013:1469–71 [DOI] [PubMed] [Google Scholar]
- 8.Tanigawa K, Sugiyama K, Matsuyama H, et al. Mesalazine-induced eosinophilic pneumonia. Respiration 1999;2013:69–72 [DOI] [PubMed] [Google Scholar]


