Abstract
Abnormal liver function tests (LFTs) are a common cause for referral to hepatology outpatient departments. Cross-sectional imaging may reveal a liver lesion. We report the case of a 33-year-old man who presented with abdominal pain and deranged LFTs and was found to have a large liver cyst on ultrasound scanning. Specific Echinococcus multilocularis serology testing was positive and he underwent triple phase CT, MRI and positron emission tomography-CT to further characterise the lesion. He was treated with long-term albendazole with subsequent improvement in symptoms, blood results and cyst size on follow-up imaging.
Background
Echinococcus multilocularis is a rare zoonotic intestinal disease. It resides in the gastrointestinal tract of foxes and is transferred to humans via the faeco-oral route. The intermediate hosts are rodents. Human infection results in the development and spread of hydatid cysts, most commonly in the liver.
The worldwide incidence of E multilocularis is rising and is particularly endemic in parts of Europe. The case highlights the importance of testing for specific forms of echinococcus when investigating cystic liver lesions and discusses current management and follow-up. Early diagnosis and treatment is crucial as it confers a massive survival benefit.
Case presentation
A 33-year-old German man living in London was found to have deranged LFTs upon routine blood testing (bilirubin 15, alanine transaminase (ALT) 140, alkaline phosphatase (ALP) 375, albumin 46, γ glutamyltransferase (GT) 734, C reactive protein (CRP) 5). He complained of mild right upper quadrant abdominal pain, particularly when leaning forward during cycling. His medical history was unremarkable. He worked as an architect, rarely drank alcohol and only took ibuprofen occasionally. He had previously travelled to Australia, America, Venezuela, Cuba and China. On examination, there was four-finger breadth palpable smooth painless hepatomegaly. He was apyrexial and had no stigmata of chronic liver disease.
Investigations
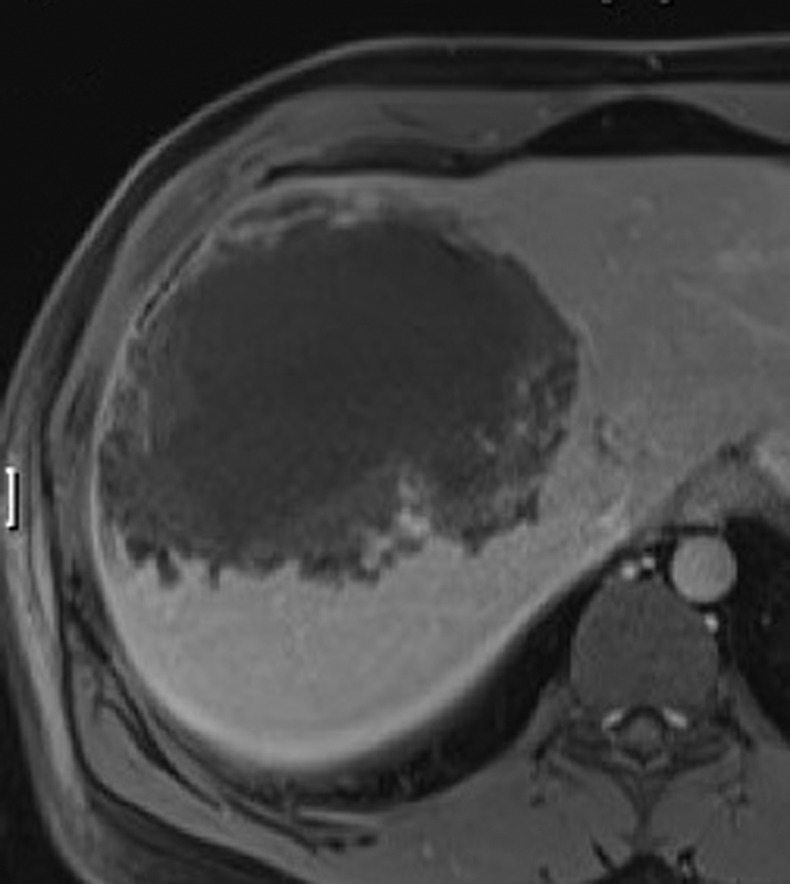
Laboratory tests including a chronic liver disease aetiology screen were unremarkable. An abdominal ultrasound was performed (figure 1) which revealed a large, thick-walled cystic mass in the right lobe of the liver (8.8×11.5×10 cm). He subsequently underwent a triple phase CT scan (figure 2) and MRI (figure 3) to further characterise the mass.
Figure 1.

Ultrasound of the liver.
Figure 2.
Triple phase CT of the liver.
Figure 3.
MRI of the liver.
A hydatid ELISA test was positive. A specific test for E multilocularis serology carried out in Switzerland was also positive, confirming the diagnosis of E multilocularis infection. The precise method of infection was unknown, but the organism could have been acquired in Germany or one of the other countries the patient had travelled to. It is not endemic in the UK.
Treatment
The benzimadazole, albendazole, was started as part of long-term medical treatment. Being a fat-soluble drug, the patient was advised to increase his hard fat intake and as a result gained considerable weight. Surgery was ruled out by the size and position of the cyst.
Outcome and follow-up
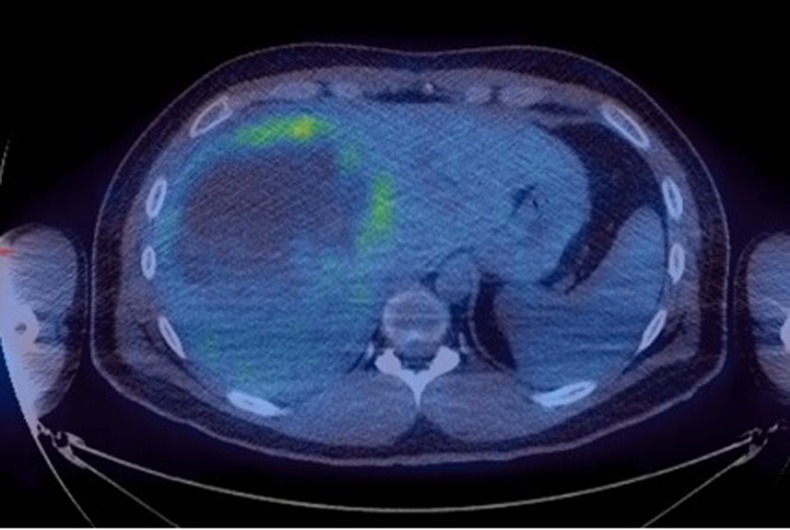
Subsequently, there was a marked improvement in the liver enzymes at 8 months (bilirubin 10, ALT 55. ALP 50, albumin 50, γGT 94, CRP 5) and the patient's abdominal discomfort disappeared. A positron emission tomography (PET)-CT (figure 4) was performed. At 1 year from diagnosis, the patient remains well and follow-up imaging with MR showed a modest reduction in cyst size.
Figure 4.

Positron emission tomography-CT.
Discussion
There are three forms of echinococcus disease: granulosus, multilocularis and vogeli. E multilocularis is a zoonotic intestinal infection. It differs from the more common E granulosus in radiological findings, clinical course, limited treatment options and poorer prognosis. The adult parasite is a 3–6 mm tapeworm that resides in the gastrointestinal tract of the definitive host, commonly foxes. Rodents serve as intermediate hosts and animal to human transmission of eggs occurs via the faecal-oral route.1 Penetration of the organism through the intestinal wall allows blood carriage of the infection. Unlike E granulosus, multilocularis does not form cysts but rather spreads by infiltration or metastasis.2 This leads to development of hydatid cysts in the liver (usually the right lobe) and can spread to the lungs, brain and heart.
E multilocularis is initially characterised by an asymptomatic period of approximately 10 years. Symptoms include cholestatic jaundice, abdominal pain or generalised fatigue and weight loss. The diagnosis is often reached late and depends on a compatible clinical picture, serology and imaging. A WHO PNM classification stages the disease. It denotes the extension of the parasitic mass in the liver (P), the involvement of neighbouring organs (N) and the presence of metastases (M).3 Ultrasound is often performed first but the combination of specific ELISA and CT have been found to be the best diagnostic investigations. ELISA has a sensitivity rate of 84–90%.4 MRI can be used to visualise adjacent structures and MRCP provides information on the cyst's relationship to the biliary tree.2 PET-CT can be used to monitor suppression of periparasitic inflammatory activity and has an important role in ruling out metastatic spread.5
A multidisciplinary approach to treatment should be undertaken, with patients referred to recognised treatment centres. The mainstay of therapy is medical, with life-long albendazole (parasitostatic agent) indicated in all patients. Drug level monitoring every 6–8 weeks with dose titration is recommended to achieve accurate therapeutic efficacy.2 Radical surgical removal of cysts is indicated in cases with small or few lesions, and percutaneous cyst drainage can be used as a palliative measure. Radiological follow-up with six-monthly ultrasound, annual MRI and two-yearly PET-CT is recommended. Mortality of untreated Echinococcus multilocularis remains high and has been historically reported as up to 100% at 3 years from diagnosis.6 However, with treatment, mean survival from diagnosis is now 20 years.7
Epidemiological data suggest that increasing urban migration of foxes in Europe correlates with increased prevalence of human echinoccocosis infection.8 The disease is now a serious public health concern in North America, Asia and Central Europe. It has not yet been shown to be present in UK animal vectors, although we are recently aware of two other cases occurring in the UK in the past year. With the increase in worldwide traffic of populace for work and residence, physicians and gastroenterologists should be increasingly aware of E multilocularis.
Learning points.
The worldwide incidence of E multilocularis is rising, particularly in Europe, and the diagnosis should be considered as a differential for a liver cyst.
E multilocularis infection presents insidiously, demonstrates metastatic behaviour and is best monitored with serial cross-sectional imaging.
A multidisciplinary approach to management and specialist advice should be sought with the mainstay of treatment being life-long albendazole.
Untreated E multilocualris has a very high mortality which is considerably improved by early diagnosis and treatment.
Acknowledgments
Professor Peter Chiodini from the Institute of Tropical Diseases.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Romig T. Spread of echinococcus multilocularis in Europe? In: Craig P, Pawlowski Z. eds. Cestode zoonosis: echinococcosis and cysticercosis. Amsterdam: IOS Press, 2002 [Google Scholar]
- 2.Brunetti E, Kern P, Vuitton DA. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Tropica 2010;2013:1–16 [DOI] [PubMed] [Google Scholar]
- 3.Kern P, Sato N, Vuitton DA. WHO classification of alveolar echinococcosis: principles and application. Parasitol Int 2006;2013:S283. [DOI] [PubMed] [Google Scholar]
- 4.McManus DP, Zhang W, Li J, et al. Echinococcosis. Lancet 2003;2013:1295–304 [DOI] [PubMed] [Google Scholar]
- 5.Stumpe KD, Renner-Schneiter EC, Kuenzie AK, et al. F-18-fluorodeoxyglucose (FDG) positron-emission tomography of Echinococcus multilocularis liver lesions: prosoective evaluation of its value for diagnosis and follow-up during benzimidazole therapy. Infection 2007;2013:11–18 [DOI] [PubMed] [Google Scholar]
- 6.Deplazes P, Eckert J. Veterinary aspects of alveolar echinococcosis-a zoonosis of public health significance. Vet Parasitol 2001;2013:65–87 [DOI] [PubMed] [Google Scholar]
- 7.Torgerson PR, Scweiger A, Deplazes P, et al. Alveolar echinococcosis: from a deadly disease to a well-controlled infection. Relative survival and economic analysis in Switzerland over the last 35 years. J Hepatol 2008;2013:72–7 [DOI] [PubMed] [Google Scholar]
- 8.Deplazes P, Hegglin P, Gloor S, et al. Wilderness in the city: the urbanization of Echinococcus multilocularis. Trends Parasitol 2004;2013:77–84 [DOI] [PubMed] [Google Scholar]


